|
Abstract:
Objective: Determine the practices of South Asian Association of
Regional Cooperation (SAARC) knee surgeons with at least 5 years
of ACL reconstruction experience.
Methods: A 15-item survey
was distributed at the Fourth SAARC Orthopaedic Association
Conference.
Results: Fourteen surgeons representing five SAARC
countries (70% of eligible attendees) completed and returned the
survey. Most (42.9%) performed 10-25 ACL reconstructions/year.
The primary graft used was a bone-patellar tendon-bone (BPTB)
autograft (57.1%). Most (50%) used a BPTB autograft >
95% of the time and a hamstring autograft < 5%, while 43%
used a hamstring autograft > 80% of the time and a BPTB
autograft < 20%. The primary tibial (85.7%) and femoral
(57.1%) fixation was interference screws. Most (62.5%) released
BPTB autograft patients back to sports at six months
post-surgery. An equal percentage (50%) released hamstring
autograft patients back to sports at six or nine months
post-surgery. Most (57.1%) did not perceive a benefit changing
to an anatomical double bundle ACL reconstruction. Concerns
were expressed about patients presenting later following index
ACL injury with more associated injuries, referring physicians
providing incomplete information, fewer surgical options due to
limited resources, the need to improvise techniques, more
frequent post-surgery hospitalization, and the need for more
educational and technology information exchanges. Conclusions:
Most experienced SAARC surgeons performed < 50 ACL
reconstructions/year with increasing hamstring autograft use.
Concerns were expressed regarding the need for additional
resources, for improved educational and technology information
exchanges, and for earlier referral with improved
documentation. Further study with greater subject numbers and
representation from all SAARC countries is needed.
J.Orthopaedics 2010;7(2)e2
Keywords:
knee; arthroscopy; survey
Background:
The South Asian
Association of Regional Cooperation (SAARC) was created in
response to economic and societal adversities experienced by
South Asian nations.1,2 The leaders of state from
seven nations, Bangladesh, Bhutan, India, Maldives, Nepal,
Pakistan and Sri Lanka adopted the original SAARC charter in
1985. In 2007, Afghanistan was formally introduced as a full
member. Committees have been established by SAARC to facilitate
seven areas of development: Agriculture-rural issues, science
technology-meteorology, health-population activities,
transportation, women-youth-children issues, human resource
development, and environment-forestry.1,2
Anterior cruciate
ligament (ACL) injuries of the knee and their sequelae are a
global healthcare concern among active individuals, particularly
females.3,4 Additionally, surgical and
rehabilitation management for this condition remain somewhat
controversial.5 Compared to Western medical
literature few reports have addressed issues related to the ACL
reconstruction and rehabilitative practices specific to SAARC
countries. Our literature search revealed that all previously
published reports come from one SAARC member nation, India.6-8
Clinical medicine as it relates to
health-population activities and SAARC standard practices,
surgical and patient outcomes following ACL injury,
reconstruction, and rehabilitation have not been previously
reported. The purpose of this pilot descriptive study was to
identify the ACL reconstruction and rehabilitation practices of
experienced SAARC knee surgeons. It is our intent that this
work will help develop prospective multi-center studies.
Materials and Methods:
A 15-item survey was
distributed at the Fourth SAARC Orthopaedic Association
Conference held in Kathmandu, Nepal to surgeons that
specialized in knee arthroscopy and who had been performing ACL
reconstruction for a minimum of five years. A departmental
ethics review board approved this study. After providing
demographic data including country of residence and age,
surgeons answered multiple choice questions regarding the number
of ACL reconstructions performed annually, how long after the
index injury ACL reconstruction was generally performed, the
primary ACL reconstruction graft choice, how many months
following ACL reconstruction the patient was allowed to return
to sports, and if prescribed for what length of time functional
knee braces were used.
Fill in the blank type
questions identified surgeon practices for current and
historical ACL reconstruction graft use (bone-patellar tendon
bone, doubled hamstring tendon, quadrupled hamstring tendon,
quadriceps tendon, or allograft), preferred ACL graft fixation
method, perceptions of how current ACL reconstruction and
treatment practice differ from current Western country practices
based on medical journals, web-based medium, or direct
observations, and on what they deem to be important for Western
country peers and companies to know about ACL reconstruction in
their country. Lastly, fill in the blank type questions were
used to identify whether or not knee braces were routinely
prescribed following ACL reconstruction, if they perceived any
advantage in changing to an anatomical double bundle ACL
reconstruction technique, and if so, to describe the ideal
patient for this technique.
Descriptive statistical analysis (SPSS
version 11.0, Chicago, IL, USA) was performed using Chi-Square
or Fisher’s Exact tests (when Chi-Square test assumptions were
not met) for categorical data comparisons. An alpha level of p
< 0.05 was selected to indicate statistical significance.
Results:
From approximately 200
hundred conference attendees, 35 surgeons were identified that
primarily performed knee arthroscopy. Of these attendees 20 had
been performing arthroscopic ACL reconstruction for a minimum of
five years prior to survey completion. Fourteen surgeons from
five SAARC countries (India = 5, Nepal = 4, Bangladesh = 2,
Pakistan = 2, and Bhutan = 1) completed the survey for a 70%
(14/20) return rate from eligible conference attendees. Surgeon
age (mean ± standard deviation) was 43.4 ± 10.4 years (range =
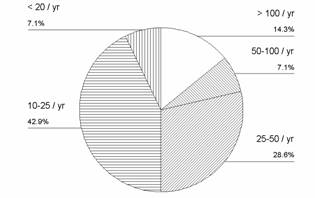
30-71 years). Most (42.9%) performed 10-25 ACL
reconstructions/year (Fig. 1).
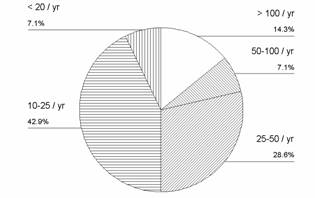
Fig.1. Number
of ACL reconstructions performed/year by experienced SAARC knee
surgeons.
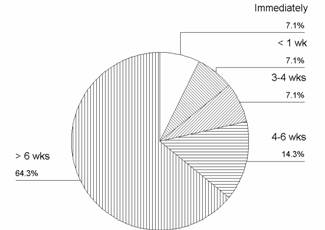
Most
performed ACL reconstruction surgery at more than six weeks
post-injury (64.3%) (Fig. 2).
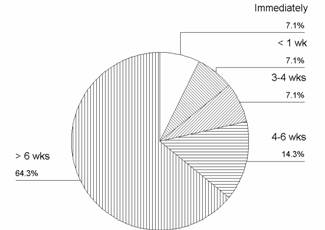
Fig. 2. Time period between index ACL injury and
surgery.
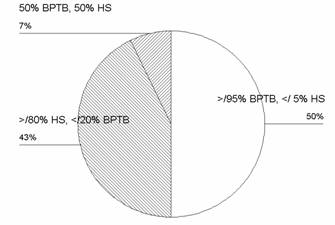
The primary graft
selected for ACL reconstruction was a bone-patellar tendon-bone
(BPTB) autograft (57.1%), with 42.9% choosing hamstring
autografts. Slightly more respondents used a BPTB autograft
> 95% of the time and a hamstring autograft < 5%
(50%) than used a hamstring autograft > 80% of the time
and a BPTB autograft < 20% (43%)(Fig. 3).
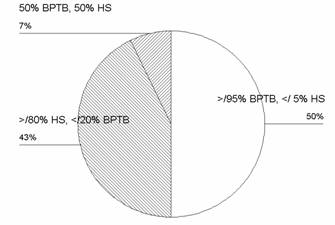
Fig. 3.
Current ACL reconstruction graft preference (BPTB = bone-patella
tendon-bone autograft; HS = hamstring autograft) of experienced
SAARC knee surgeons.
Two experienced surgeons
that had recently changed their primary ACL reconstruction graft
preference switched from either 100% BPTB autograft or 75% BPTB
autograft and 25% double strand hamstring graft use to greater
use of two or four strand hamstring autografts. The primary
method of tibial (85.7%) and femoral (57.1%) graft fixation was
interference screws. The second most frequent femoral fixation
method was endo-buttons (35.7%) and the second most frequent
tibial fixation method was a screw-post combination (7.1%). The
most frequent time of release to unrestricted activities of
daily living for BPTB autograft patients was 5-6 months (37.5%)
followed by 10-12 months (25%), 3-4 months (25%), and 1-2 months
(12.5%). The most frequent time of release to unrestricted
activities for hamstring autograft patients was 7-9 months
(66.7%), 5-6 months (16.7%) and 1-2 months (16.7%). The time of
release to unrestricted activities of daily living between graft
types did not display statistically significant differences
(Fisher’s Exact Test = 3.2, p = 0.61). Most surgeons released
patients with a BPTB autograft (62.5%) back to sports at six
months post-surgery followed by nine months post-surgery (25%)
and > 12 months post-surgery (12.5%). Surgeons were equally
divided (50%) for releasing patients with a hamstring autograft
back to sports either at six or nine months post-surgery. The
timing of release back to sports did not display statistically
significant differences between graft types (Fisher’s Exact
Test = 1.4, P = 0.77). Most surgeons (57.1%) did not routinely
prescribe a functional knee brace post-surgery. Of those who
prescribed knee braces, most (60%) recommended use for less than
six months post-surgery while 40% recommended their use for six
months – one year. Experienced knee surgeons from India were
more likely to prescribe a functional knee brace post-surgery
(80%, 4 of 5 surgeons) than experienced knee surgeons from the
other SAARC countries (22.2%, 2 of 9 surgeons). Most surgeons
(57.1%) did not perceive a substantial benefit in changing from
their current ACL reconstruction method to use of an anatomical
double bundle ACL reconstruction technique. Surgeons who
believed that a benefit would exist believed that it would be
most advantageous for high re-injury risk athletes such as
competitive soccer players and revision cases.
Perceived ACL
reconstruction practice differences compared to Western
countries based on what surgeons had observed in Western
journals, web-based medium, or travels, included, fewer surgical
options due to limited facility, equipment and implant
availability (Bangladesh), a widespread need to improvise
surgical techniques (Pakistan), a higher percentage of male
cases (India), fewer opportunities for revision surgery with the
athlete remaining active in sports (India), the need for 2-3 day
post-surgery hospitalization (Nepal), and patients tending to
present for treatment later following the index ACL injury with
a greater number of associated injuries (India, Nepal).
Surgeons who provided comments as to what they believed their
peers and companies in Western countries should know about ACL
reconstruction in their country suggested that many patients
present to them a considerable time period following the index
ACL injury (Pakistan), there is often poor or inaccurate
documentation from the referring general care physician
regarding the patient’s injury history (India), limited
facility, equipment, and implant resource availability (Nepal),
the belief that comparable patient outcomes can be achieved
despite existing facility and other patient care difficulties
(Nepal), the effectiveness of simple, inexpensive knee braces
(India) and the need for more arthroscopic and sports medicine
education and technology information transfer and fellowship
experiences (India).
Discussion :
A similar percentage of
SAARC knee surgeons selected BPTB and hamstring autografts for
ACL reconstruction. This is not surprising given the history of
similar patient outcome effectiveness between these graft types9
and the growing trend toward greater hamstring autograft use.10
Additionally, the majority of respondents performed < 50 ACL
reconstructions/ year, which also is comparable to Western
country practices.11,12 Knee surgeons in Western
countries often prescribe functional knee braces following ACL
reconstruction to prevent graft strain, decrease pain, improve
knee extension range of motion and restrict end range movements
to facilitate graft healing. In a systematic review that
assessed knee joint range of motion, ACL graft laxity, knee pain
level, and re-injury risk however, Wright et al13
reported that none of these variables were influenced by knee
brace use following ACL reconstruction. The more restricted use
of functional knee braces by experienced SAARC knee surgeons
suggests a better use of limited resources, particularly given
the limited evidence supporting the efficacy of regular
functional knee brace use. Perhaps knee surgeons in Western
countries should re-examine their routine prescription of
expensive custom or “off the shelf” knee braces following ACL
reconstruction given this limited evidence. Two experienced
SAARC knee surgeons (India, Pakistan) recommended that
short-term use of simple, inexpensive knee braces was
sufficient.
A growing number of knee
surgeons are attempting to more closely replicate native ACL
function via the use of anatomical double bundle ACL
reconstruction techniques. This trend is occurring
despite the considerable body of evidence that supports
conventional ACL reconstruction methods and the limited evidence
for improved patient outcomes that exist supporting anatomical
double bundle ACL reconstruction. Most experienced
SAARC knee surgeons did not believe that anatomical double
bundle ACL reconstruction would provide a significant advantage
over conventional single bundle ACL reconstruction methods.
Those who did suggested that sportsmen such as competitive
soccer athletes and revision cases would benefit most.
Surgeon perceptions regarding what
they deemed important that Western country knee surgeons and
companies should know about ACL reconstruction in their country
differed somewhat based on the SAARC country of origin. For
example, experienced knee surgeons from Nepal, Pakistan,
Bangladesh, and Bhutan expressed greater concerns related to
limited medical resource availability, the need to more
frequently improvise or modify surgical techniques, and the more
common need for post-surgery hospitalization. In contrast,
experienced knee surgeons from India more commonly expressed
concerns related to the need for arthroscopy and sports medicine
educational information and technology exchanges. In contrast
to knee surgeons in India who seek technique refinement and
updates, knee surgeons in other SAARC countries were more
interested in obtaining basic assistance at the immediate
patient care level.
A recurrent theme from
most experienced SAARC knee surgeons was a concern regarding low
public health awareness as to the significance of the index ACL
injury and how delayed treatment is associated with injury to
adjacent knee tissues, progressive lower extremity dysfunction,
and decreased general health (India, Nepal, Pakistan). This
finding is similar to rural healthcare issues experienced in
many Western countries where limited medical personnel and
facility resources, increased travel distances, and decreased
public awareness combine to lead patients to only seek
healthcare after their condition or disease has progressed to
being chronic, extremely painful, and highly debilitating.
Optimized use of
available equipment and personnel resources is essential to the
development of improved public health education and awareness
regarding the seriousness of ACL injury. These initiatives may
help to identify currently untapped resources, to better
distribute existing resources, and to facilitate better resource
sharing between SAARC member nations. Cooperative planning in
the prescriptive development of arthroscopy and sports medicine
educational and technology information exchange programs would
help insure that the needs of all SAARC member countries are met
(both basic necessities and technique refinement), better
supporting the organization’s overall vision and mission.
This study is limited in
that it represents only a small sample of experienced SAARC knee
surgeons that specialize in arthroscopic ACL reconstruction.
However, this is a very unique group of experienced knee
surgeons whose ACL reconstruction practice experiences have not
been previously reported. Our literature search did not
identify any previous reports that focused on ACL reconstruction
practices solely in this region of the world. Pilot studies
such as this are important to collect preliminary data, refine
prospective research questions and plans, and develop research
instruments. Based on our study findings, future research
should focus on increasing the awareness of the general public
regarding the potential impact of ACL injury on general health
and quality of life and to increase the awareness of general
practice physicians as to the need to improve examination
documentation and/or to expedite referral to a knee arthroscopy
specialist when indicated. Further study needs to be performed
recruiting a larger number of experienced knee surgeons
including representatives from other SAARC countries such as the
Maldives, Sri Lanka, and Afghanistan.
Given the other
important healthcare problems that exist in the region served by
SAARC14-15 issues related to arthroscopic ACL
reconstruction may not initially seem to be of particular
importance. However, untreated or inappropriately treated lower
extremity musculoskeletal injuries are a serious worldwide
health concern that directly impacts general health status.
Information such as that provided by this study will better
enable the SAARC medical community to establish arthroscopy and
sports medicine education and technology information exchange
program goals in addition to helping design multi-center,
prospective research studies to improve patient healthcare and
quality of life.
Conclusions:
Experienced SAARC knee surgeons displayed similar ACL
reconstruction practices to surgeons from Western countries.
Most of the experienced SAARC knee surgeons that participated in
this study perform < 50 ACL reconstructions per year. There was
trend toward increasing hamstring autograft use and did not
routinely prescribe functional knee braces. Most experienced
SAARC knee surgeons also did not perceive a benefit to changing
their current surgical procedure to an anatomical double bundle
ACL reconstruction technique. Many experienced SAARC knee
surgeons expressed concerns regarding the need for additional
medical and surgical resources, improved arthroscopy and sports
medicine educational and technology information exchange and
fellowship experiences, earlier patient referral with improved
documentation, and improved public awareness regarding the
impact of ACL injury on general health status. Our findings can
assist the SAARC sports medicine community in establishing
realistic organizational goals and in designing prospective
multi-center studies to better serve the needs of all member
nations.
Reference :
1.
South Asian Association
for Regional Cooperation. [http://www.saarc-sec.org/]
Wikipedia. [http://en.wikipedia.org/w/index.php?title=South
Asian Association for Regional Cooperation&olddid=23181920]
2. Prodromos CC, Han
Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence
of anterior cruciate ligament tears as a function of gender,
sport, and knee injury-reduction regimen. Arthroscopy 2007,
23(12):1320-25.e6
3. [http://download.journals.elsevierhealth.com/pdfs/journals/0749-
8063/PIIS074980630700686X.pdf]
4.
Renstrom P, Ljungqvist
A, Arendt E, Beynnon B, Fukubayashi T, et al. Non-contact ACL
injuries in female athletes: An International Olympic Committee
current concepts statement. Br J Sports Med
2008;42(6):394-412. [http://bjsm.bmj.com/content/42/6/394.full.pdf]
5.
Marx RG, Jones EC, Angel
M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members
of the American Academy of Orthopaedic Surgeons regarding the
treatment of anterior cruciate ligament injury. Arthroscopy
2003;19(7):762-70. [http://download.journals.elsevierhealth.com/pdfs/journals/0749-8063/PIIS0749806303003980.pdf]
6.
Chaudhary D, Monga P,
Joshi D, Easwaran R, Bhatia N, Singh AK. Arthroscopic
reconstruction of the anterior cruciate ligament using
bone-patellar tendon-bone autograft: Experience of the first
100 cases. J Orthop Surg (Hong Kong) 2005;13(2):147-52.
[http://www.josonline.org/pdf/v13i2p147.pdf]
7.
Nag HL, Neogi DS,
Nataraj AR, Kumar VA, Yadav CS, Singh U. Tubercular infection
after arthroscopic anterior cruciate ligament reconstruction.
Arthroscopy 2009;25(2):131-6. [http://download.journals.elsevierhealth.com/pdfs/journals/0749-8063/PIIS0749806308007263.pdf]
8.
Dhillon MS, Mohan P,
Nagi ON. Does harvesting the medial third of the patellar
tendon cause lateral shift of the patella after ACL
reconstruction? Acta Orthop Belg 2003;69(4):334-40. [http://www.actaorthopaedica.be/acta/download/2003-4/06-dhillon-nagi-.pdf]
9.
Biau DJ, Tournoux C,
Katsahian S, Schranz P, Nizard R. ACL reconstruction: A
meta-analysis of functional scores. Clin Orthop 2007;458:180-7.
[http://www.ncbi.nlm.nih.gov/pubmed/17308473]
10.
West RV, Harner CD.
Graft selection in anterior cruciate ligament reconstruction. J
Am Acad Orthop Surg 2005;13(3):197-207. [http://www.jaaos.org/cgi/content/abstract/13/3/197]
11.
Duquin TR, Wind WM,
Fineberg MS, Smolinski RJ, Buyea CM. Current trends in anterior
cruciate ligament reconstruction. J Knee Surg 2009;22(1):7-12.
[http://www.ncbi.nlm.nih.gov/pubmed/19216345]
12.
Forssblad M, Valentin A,
Engstrom B, Werner S. ACL reconstruction: Patellar tendon
versus hamstring grafts-economical aspects. Knee Surg Sports
Traumatol Arthrosc 2006;14(6):536-41. [http://www.springerlink.com/content/r146507716477710/]
13.
Wright R, Fetzer GB,
Spindler KP. Bracing after ACL reconstruction: A systematic
review. Clin Orthop 2007:455:162-8. [http://www.ncbi.nlm.nih.gov/pubmed/17279043]
14.
Nishtar S. South Asian
health: What is to be done? SAARC: Regional cooperation for
sustainable health. BMJ2004;328:837-9.[http://www.bmj.com/cgi/content/full/328/7443/837-a?view=long&pmid=15070648]
15.
Khan IM, Khan S, Chotani
R, Laaser U. SARS and SAARC: Lessons for preparedness.
J Ayub Med Coll Abbottabad
2003;15(2):1-2. [http://www.ncbi.nlm.nih.gov/pubmed/14552237]
|