|
Abstract:
The use of Autologous blood transfusion (ABT) has been
recommended in primary total knee arthroplasty and also in
revision hip arthroplasty. Currently, however, no guidelines
exist regarding its use in primary total hip arthroplasty (THA).
The purpose of this study was to assess whether the use of ABT
in primary THA reduced the overall rate of allogeneic
transfusion.
We prospectively reviewed 80 patients who underwent primary THA
with ABT between June 2005 and January 2007 (study group). 33
patients who underwent primary THA without ABT during the same
period were used as controls. All patients were operated on by
the senior author (SLK). We compared the pre-op and post-op
haemoglobin and PCV, intra and post operative blood loss, volume
of blood re-transfused using the ABT system and volume of
allogeneic blood transfused in both groups.
A significantly higher number of patients received allogeneic
blood transfusion in the control Group (45.5%) compared to
patients in the study group (27.5 %) p<0.03. The mean volume of
allogeneic blood transfused per person in the study group was
0.65 units (195mls) compared to 0.82 units (245mls) in the
control group.
Of the 80 patients in the study group, 34 had autologous blood
transfused. The mean volume transfused in these 34 patients was
309.26 mls which equated to a mean of 131.44 mls of autologous
blood transfused per person in the study group. There was no
significant difference in the mean drop in Hb or PCV,
immediately post op or at discharge between the two groups.
Our study suggests that the use of autologous blood transfusion
reduces the requirement of allogeneic blood transfusion in
primary THA.
J.Orthopaedics 2009;6(3)e12
Keywords:
Primary hip replacement;
autologous blood transfusion
Introduction:
Salvage of blood following surgery and reinfusion has been shown
to reduce the need for allogeneic blood transfusion in several
studies.( 1,2,3 ) There are many recognised
complications following allogeneic blood transfusion including
disease transmission, transfusion reactions and immunomodulation.(1,2)
Reduction in infections after orthopaedic procedures has been
associated with the avoidance of allogeneic transfusion.(4)
Although the implementation of blood screening measures have
greatly reduced the risk of transmission of blood borne
infection, this still remains a major concern. Current options
for blood management in Orthopaedic procedures include good
anaesthetic and operative technique, preoperative autologous
blood donation, intraoperative and postoperative blood salvage,
acute normovolemic haemodilution, unit by unit allogeneic blood
transfusion and pharmacologic interventions eg Epoetin alfa,
Tranexamic acid and Aprotinin.(1,3) Nonetheless, recent studies
have reported an allogeneic blood transfusion rate of 39% -57%
following joint replacement surgery.(6,7) Autologous
drains are increasingly used in total knee arthroplasty (TKA)
and guidelines issued by the British Orthopaedic Association
recommend their use.(5) Currently, however, no guidelines exist
in the UK regarding the use of autologous drains in primary
Total Hip Arthroplasty (THA).
We have been using autologous drains in all patients undergoing
primary THA since January 2006. The aim of this study was to
evaluate the efficacy of autologous drains in primary THAs. We
assessed whether a reasonable volume of blood was collected for
re-infusion in a sufficient number of patients and whether this
resulted in an overall reduction in allogeneic transfusion
requirements.
Materials
and Methods:
All primary THAs carried out for Osteoarthritis of the hip by
the senior author between June 2005 and January 2007 were
included in the study. 13 patients in whom a complete data set
was not available were excluded. Data for the study group was
collected prospectively and comparison made with a control
group. All patients in the control group underwent THA without
the use of ABT. All procedures were carried out under general
anaesthetic by the senior author or under his direct
supervision. The posterior approach was used in all cases with
the patient in the lateral position. The same standard peri-operative
regimen was used throughout. All patients received aspirin 150mg
post operatively for six weeks as thrombo-embolic prophylaxis
(unless there was a specific contraindication to aspirin). IRB/Ethics
Committee approval was not required for this study.
Between June 2005 and January 2006, 33 patients received a
standard deep drain. These patients formed the Control group.
The standard drainage system used was the Bellovac low-vacuum
drain (Astra Tech, Gloucester),™ referred to as
‘normal drains’ throughout the rest of this paper. Since January
2006, 80 consecutive patients had a single autologous drain
lying deep to the fascia lata. These patients formed the Study
group. The autologous drainage system used was the Bellovac
A.B.T (Astra Tech) ™. These are referred to as
‘autologous drains’ throughout the rest of this paper. Blood
drained in the first 6 hours was re-infused. After six hours the
drain continued to function as a ‘normal drain’. All drains were
removed within 24 hours following surgery.
The criteria for allogeneic blood transfusion was determined
according to the protocol established by the hospital
transfusion committee and it remained constant throughout the
study. Only symptomatic patients with haemoglobin less than 8.0
g/dl received allogeneic blood transfusion. The decision to
transfuse was made in conjunction with the senior author (SLK).
The patients’ case notes, and electronic patient records were
reviewed. The volume of blood drained, volume of autologous
blood re-infused, volume of allogeneic blood transfused, pre and
post operative haemoglobin, packed cell volume (PCV), length of
hospital stay, age, sex, and ASA grade was reviewed in all
patients in both groups.
Statistical analysis was carried out using the SPSS version 11
statistical package (SPSS, Chicago, IL, USA). Independent
samples t test was used to assess the difference between the
preoperative and postoperative haemoglobin and PCV. The z-test
was used to compare the volume of allogeneic blood transfused
and the chi-squared test to compare the transfusion rates
between each group.
Results :
A total of 113 patients were reviewed. 80 patients in the study
group had an autologous drain while 33 patients in the control
group had the ‘normal drain’. All patients had osteoarthritis of
the hip. The patient characteristics in both groups were
matched (Table 1).
|
|
Study group |
Control group |
|
Patients |
80 (33M,47F) |
33 (8M, 25F) |
|
Mean age |
68.8 (45 – 87) |
66.4 (51 – 81) |
|
Mean ASA |
1.95 (1 – 3)
|
1.88 (1 – 3) |
|
Pre-operative Haemoglobin |
13.5 (8.0–15.8) |
13.5 (9.9–15.6) |
Table 1: Patient characteristics of the two groups
There was no significant difference when comparing the pre-op
haemoglobin and the haemoglobin on discharge in both groups.
There was no significant difference in the immediate
postoperative PCV in either group, thus peri-operative
haemodilution was comparable in both groups. Length of
stay was similar in both groups as well.
There was no significant difference in the mean volume of
blood drained in both groups (205ml in the study group,
209 ml in the control group). The mean volume of allogeneic
blood transfused per person in the study group was 195ml
compared to 245ml in the control group (Table 2).
|
|
Study group
(n = 80)
|
Control group
(n = 33) |
|
Mean vol. drained (mls) [range]
|
205 (10-1200) |
209 (60 – 1050) |
|
Mean allogeneic transfusion
(mls per patient) [range] |
195 (0 – 1500) |
245 (0 – 1200) |
Table 2:
Drainage and transfusion in the two groups
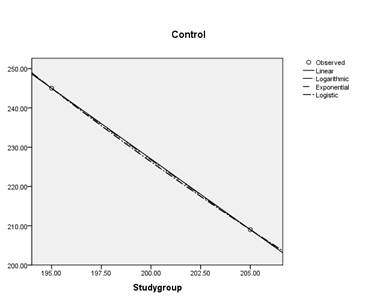
This difference of 50 mls per person was however, not
statistically significant (Graph-1).
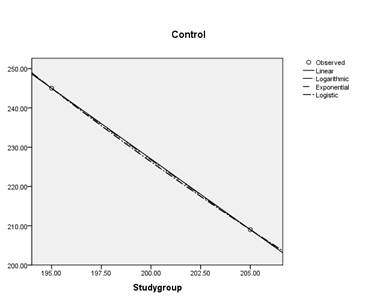
Graph 1: Curve fit model (regression analysis) shows no
significant difference
26.3% (21/80) of patients in the autologous drain group required
allogeneic blood transfusion while 45.5% (15/33) of those in the
normal drain group required allogeneic blood transfusion. This
was statistically significant (p<0.03) {z-test of proportions}.
The mean volume of drainage in the THAs with uncemented implants
was significantly higher than in the THAs using cemented
implants.(p<0.03)(Table 3)
|
|
Study Group
|
Control Group |
|
Number of patients |
Mean Volume Drained (mls) |
Number of patients |
Mean Volume Drained (mls) |
|
Cemented Implants |
19 |
113.3
Range (0 - 500) |
8
|
117.1
Range (0 – 460) |
|
Uncemented Implants |
51
|
224.6
Range (0 – 1200) |
9
|
258.7
Range (0 – 1050) |
|
Hybrid
Implants |
10 |
312.0
Range ( 0 – 540) |
16 |
204.4
Range (0 – 820) |
|
p value |
|
p<0.03 |
|
p<0.03 |
Table
3:
Drainage
in Cemented vs. Uncemented implants
In the autologous drain group, 34/80 (42.5%) had some autologous
blood reinfused. The mean volume of autologous blood reinfused
in this group was 309ml per person (range 100-1100ml). 46
patients in the study group did not have any autologous blood
reinfused. In 43 cases this was due to an insufficient volume
(<100ml) of blood drained within the stipulated time of six
hours. In the remaining 3 cases the documentation was incomplete
and consequently the autologous blood collected had to be
discarded. The volume of blood re-infused using the autologous
drainage system is shown in Figure 1.
Figure 1:Volume
of blood re-infused (ABT) in study group
The allogeneic blood transfusion requirements in each group are
shown in Figures 2a and 2b.
Figure 2a:Volume
of allogeneic blood transfused in Study group
Figure 2b:Volume
of Allogeneic blood transfused in Control group
Discussion:
Arthroplasty surgery is associated with significant blood loss
and allogeneic blood transfusion is required in many cases.
Despite numerous advances in operative technique and peri-operative
pharmacological interventions, blood loss in primary hip and
knee arthroplasty may be considerable. In the UK, 10% of
allogeneic blood is used by orthopaedic patients and 40% of this
by patients undergoing hip and knee arthroplasty.(11) The
ultimate goal of blood management by Orthopaedic surgeons is to
eliminate the need for allogeneic blood transfusion.(13)
Postoperative blood salvage using autologous re-infusion drains
have been shown to reduce allogeneic transfusion requirements in
total knee arthroplasty by 86% (9) with obvious economic and
clinical benefits. Allogeneic blood transfusion has been
reported to be associated with a five fold increase in inpatient
infection rates (12) and increase in the length of hospital stay
(9). In TKA the mean total blood loss ranges from 520-1600ml
almost all of which occurs postoperatively, following release of
the tourniquet. In comparison the mean total blood loss in THA
has been reported to be between 550-2200ml, approximately half
of which is lost post-operatively.
Slagis et al have reported that postoperative blood salvage was
not economically justified in THAs. (2) However, they
used a washed cell salvage system which resulted in significant
costs. Keating et al have reported that blood salvage was not
cost effective in THA because not enough blood was collected
post operatively. (11) Our study has shown that a
mean volume of blood of 309ml was collected for re-infusion in
almost half of our patients. This has resulted in a significant
reduction in the incidence of allogeneic blood transfusion. Some
authors have reported side effects including hypotension,
hyperthermia and febrile reactions to the transfusion of
unwashed, filtered salvaged blood.(15) In our study we did not
encounter any adverse reactions to the autologous blood
transfusion.
Sturdee et al have recently reviewed their use of autologous
drains in primary THAs and concluded that they should be used.
(11) Our results would support their findings.
In the recent past un-cemented implants have been increasingly
used for primary THA in the UK and this popular trend is
reflected in our study. We have shown a significant increase in
the volume of blood drained in un-cemented THAs as compared to
cemented THAs and this would further justify the usage of ABT
drains in patients undergoing primary THA using un-cemented
implants.
Conclusion:
The routine use of surgical drains in total hip arthroplasty (THA)
remains controversial (4) Ritter et al reported no difference in
transfusion rate or haemoglobin decrease between patients with
or without drains in THA.(15) Nonetheless, in the UK, drains are
widely used following primary THA. We recommend that if a drain
is to be used, then an autologous drainage system should be
considered in preference to a ‘normal’ drain, especially if
un-cemented implants are being implanted.
Acknowledgements:
We are grateful to Mr J. Turner, Statistician, Cardiff
University, for his help with statistical analyses.
References:
-
Majkowski RS, Currie IC, Newman JH.
Postoperative collection and reinfusion of autologous blood in
total knee arthroplasty. Ann R Coll Surg Engl 1991; 73:381-4.
-
Slagis SV, Benjamin JB, Volz RG, Giordano GF.
Postoperative blood salvage in total hip and knee arthroplasty:
A randomised controlled trial. J Bone Joint Surg(Br)
1991;73:591-4.
-
Dalen T, Skak S, Thorsen K, Fredin
H. The efficacy and safety of blood reinfusion in avoiding
homologous transfusion after Total Knee Arthroplasty. American
Journal of Knee Surgery 1996;9(3):117-120.
-
Faris PM, Ritter MA, Keating EM,
Valeri CR. Unwashed filtered shed blood collected after hip
and knee arthroplasties. J. Bone Joint Surg (A) 1991; 73-A:
1169-78.
-
Walmsley PJ, Kelly MB, Hill RN,
Brenkel I. A prospective, randomised, controlled trial
of the use of drains in total hip arthroplasty. J Bone Joint
Surg (Br) 2005; 87-B(10): 1397-1401.
-
Blood Conservation in elective
orthopaedic surgery: British Orthopaedic Association, April
2005.
-
Bierbaum BE, Callaghan JJ, Galante
JO. An analysis of blood management inpatients having a total
hip or knee arthroplasty. J Bone Joint Surg (Am)
1999;81-A:2-10.
-
Hatzidakis AM, Mendlick RM, McKillip
T. Preoperative autologous donationfor total joint
arthroplasty. J Bone Joint Surg (Am) 2000; 82-A:89-100.
-
Newman JH, Bowers M, Murphy J. The
Clinical advantages of Autologous Transfusion A randomised
controlled study after knee replacement. J Bone Joint Surg
(Br)1997; 79-B(4): 630-32.
-
Keating EM, Ritter MA. Transfusion
options in total joint arthroplasty. J Arthroplasty 2002; 17:
125-8.
-
Sturdee SW, Beard DJ, Nandhara G,
Sonanis SV. Decreasing the blood transfusion rate in elective
hip replacement surgery using an autologous drainage system.
Ann R Coll Surg Engl 2007;89:136-139
-
Triulzi DJ, Vanek K, Ryan DH,
Blumberg N. A Clinical and immunologic study of blood
transfusion and postoperative bacterial infection in spinal
surgery. Transfusion 1992; 32(6): 517-524
-
Keating EM. Current options and
approaches for blood management in orthopaedic surgery. An
instructional course lecture. J Bone Joint Surg 1998; 80-A
(5): 750-762.
-
Ritter MA, Keating EM, Faris PM.
Closed wound drainage in total hip or knee replacement. A
prospective randomised study. J Bone Joint Surg Am 1994;
76:35-8
-
Blevins FT, Shaw B, Valeri CR,
Kasser J, Hall J. Reinfusion of shed blood after orthopaedic
procedures in children and adolescents J Bone Joint Surg(Am)
1993; 75: 363-71.alysis) shows no significant difference.
|