|
Abstract The deposition of
gouty tophi in the hand occurs relatively late in the disease.
Involvement of carpal bones is nowhere reported in the
literature. We present a 40-year-old man with a long duration of
gouty arthritis involving the carpal bones.
J.Orthopaedics 2006;3(4)e10
Introduction:
Gouty arthritis has various modalities of presentations in
the hand. Metacarpo-phalangeal joints are most commonly involved
in gouty arthritis. The differential diagnosis includes
Psoriasis, Osteoarthritis, Infection, Calcium pyrophosphate
dehydrate de-position of disease (CPPD) and Rheumatoid
arthritis. Proper clinical examination, laboratory evaluations,
and histological examinations will confirm the diagnosis.
We present a 40-year-old man with gouty arthritis and
deposition of tophi over the dorsal aspect of wrist involving
the carpal bones.
Case Report
A 40-year-old man, presented to the clinic with complaints of
left knee pain. His medical history included 18-year-old history
of gouty arthritis and on and off treatment for the same. He
used to take non-steroidal anti-inflammatory drugs for
occasional pain in both feet. He also took allupurinol along
with non-steroidal inflammatory drugs during acute attacks of
joint pain and prophylaxis up to the age of 35 years.

On examination of the left knee, there was a no effusion.
Knee movements were clinically normal. Multiple small nodules
were seen on the dorsum of the left hand with a 2*3 cm large
nodule over the base of third metacarpal. They are not warm, not
tender, and cystic to firm in consistency and the underlying
extensors tendons were free. The skin over the nodules was
normal and pinchable. No discharging sinus or ulcer noted.
Multiple tophaceous deposits, grayish discoloration, hallux
valgus deformity were noted on the great toe on both sides. A
large localized swelling was seen in the retrocalcaneal region
of this patient that was cystic in nature, not warm and tender
and free from the tendo calcaneus.
Erythrocyte sedimentation rate was 25 mm in the first hour
(normal <14). His blood parameters revealed hemoglobin 11.2gms,
TLC 7,500cu\mm. Complete blood counts, C-reactive protein, liver
function tests, creatinine, electrolytes, and thyroid function
test and protein electrophoresis were normal. Tests for
anti-nuclear body, rheumatoid factor and HLA- B27 were negative.
Serum uric acid was 4.1mgs (Normal 3-7 mgs). Ultrasound KUB was
normal. Urine examinations were normal.
Radiograph of the wrist Fig (1) showed, a circular
punched-out lytic lesion involving scaphoid, capitate and
trapezoid bones. Metacarpals, phalanges were normal. Radiograph
of the feet revealed a classic ‘punched-out’ lytic lesion,
marginal erosions and an associated overhanging edge at the
distal metatarsals.
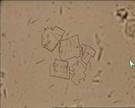
Straw colored fluid was aspirated from both retrocalcaneal
region and left wrist dorsal swelling. Microscopic examination
and culture for aerobic, anerobic, acid fast, and fungal
organisms were negative. Rhomboidal shaped urate crystals were
seen with few RBC’s in between Fig (2). Pus cells were not seen.
He was treated with non-steroidal anti-inflammatory drugs,
protected weight bearing and physiotherapy. Four weeks after the
visit, he had improved, with decreased pain and increased
movement.
Discussion :
Deposition of gouty tophi in the hand occurs relatively late
in the disease and is uncommon with good medical management4.
Radiographic manifestations of gouty arthritis may precede
symptoms in up to 25% of patients and may precede deposition of
gouty tophi in up to 42% 5.
Gouty arthritis has various modalities of presentations in
the hand. This includes acute suppurative flexor
tenosynovitis4,6, carpal tunnel syndrome4,7, and a localized
painful mass in the mid-palm1,2,3, tophi over the dorsal aspect
of the interphalangeal and metacarpophalangeal joints1,2,3.
Neglected cases can produce intratendinous infiltration, flexion
contractures, tendon rupture, and skin ulceration in extreme
cases1,6.
Gouty tenosynovitis in the hand can be present without tophi
or previous involvement of upper extremity6. Often called “the
imitator”, gout may masquerade as septic arthritis, rheumatoid
arthritis or neoplasm, and the diagnosis is often delayed by
weeks or months.
Gout can rarely coexist with rheumatoid arthritis,8 but it is
perhaps more frequently misdiagnosed as rheumatoid arthritis
because of its proliferative synovitis6 and because 10% to 20%
of patients with rheumatoid arthritis have elevated uric acid
levels.
The early radiological signs of gout are joint effusion and
periarticular edema, caused by the deposition of the non-opaque
crystals within the synovial and cartilaginous tissues1,2,3.
Radiographic examination eventually reveals a classic
‘punched-out’ lytic lesion with an associated overhanging edge
at the distal metatarsals2. Multiple marginal erosions and
decreased joint space are seen at several metacarpal-phalangeal
joints. These erosions contain sclerotic borders5.
Osteopenia and the loss of joint space are usually not seen
until advanced disease stages2. Additionally, the advanced stage
is also characterized by joint destruction and severe
deformities. Proliferative osseous change, intraosseous cysts,
chondrocalcinosis and olecranon bursitis can occasionally be
seen in the patients with gout1.
The diagnosis of gout should not be based on laboratory
values alone. Joint or tenosynovial aspiration, Gram stain, and
examination under polarized light is 85% sensitive for the
diagnosis of gout and may be helpful in differentiating acute
gouty tenosynovitis from rheumatoid arthritis or infection3.
The asymmetry and lack of joint space narrowing not seen
until advance stages allow differentiation from other
similar-appearing disorders (e.g., Psoriasis, Osteoarthritis,
Infection, and Rheumatoid arthritis). Calcium pyrophosphate
dehydrate de-position disease (CPPD) can have symptoms
resembling that of gout and can also occur concomitantly in up
to 40% of patients with gout9.
Our patient who was on long duration of treatment for gouty
arthritis presented to our clinic with non-specific knee pain
and an incidental radiological evaluation of left hand showed
the involvement of carpal bones.
Our review of literature did not show carpal involvement in
gouty arthritis. Our patient had multiple tophi deposition on
the dorsum of hand. Histological examination demonstrated urate
crystals from the aspirate of hand and retrocalcaneal region and
confirmed the carpal involvement.
Conclusion
Gouty arthritis can also occur in carpal
bones. It can occur alone or along with or without the
associated findings. One should always have a high index of
suspicion. Systematic, good clinical examination and proper
radiographs should be carried out. Histology confirms the
diagnosis. Carpal involvement in gouty arthritis should also be
kept in the differential diagnosis in any case of unusual lytic
lesions in carpal bones.
Gouty arthritis has a various presentations
in hand. They include acute tenosynovitis, carpal tunnel
syndrome, tophi deposition in palm, punched-out lytic lesions;
metacarpals are usually involved. Carpal bones are not involved.
This case showed the involvement of carpal bone. One should be
careful in interpreting hand radiographs. A systematic clinical
examination along with radiographs and aspiration cytology
confirms the diagnosis.
Reference :
- Zayas VM, Calimano MT, Acosta AR, et al. Gout: The
radiology and clinical manifestations. Appl Radiol. 2001;
30(11): 15-23
- Uri DS, Dalinka MK. Crystal Disease. Radiol Clin North
Am.1996; 34:359-364
- Becker MA: Clinical aspects of monosodium urate
monohydrate crystal deposition disease (gout). Rheum Dis Clin
North Am 14:377-394, 1988.
- Moore JR, Weiland AJ: Gouty tenosynovitis in the hand. J
Hand Surg [Am]10: 291-295, 1985.
- Barthelemy CR, Nakayama DA, Carrera GF, et al: Gouty
arthritis: Aprospective radiographic evaluation of sixty
patients. Skeletol Radiol 11:1-8,1984.
- Abrahamsson SO: Gouty tenosynovitis simulating an
infection: A casereport. Acta Orthop Scand 58:
282-283,1987.7.
- Janssen T, Rayan GM: Gouty tenosynovitis and compression
neuropathy ofthe median nerve. Clin Orthop Mar (216):
203-206,1987.
- Atdjian M, Fernandez-Madrid F: Coexistence of chronic
tophaceous goutand rheumatoid arthritis. J Rheumatol 8:
989-992,1981.
- Lagier R, Boivin G, Gerster JC: Carpal tunnel syndrome
associated withmixed calcium pyrophosphate dihydrate and
apatite crystal deposition intendon synovial sheath. Arthritis
Rheum 27: 1190-1195,1984.
|