|
Abstract:
Aim: The
implantation of short stem prostheses in hip arthroplasty is
gaining in importance. Because these implants have only become
available for a few years, there is little data to facilitate
the learning curve and clinical outcome. By nature, therefore,
long-term results are missing.
Methods:Clinical
and radiographic results and complications are documented in a
single surgeon, retrospective study using our own patient
population. The study group totals 108 patients receiving 120
short stem implants. Of all treatments (n=120), the data in
respect of surgery, perioperative complications, implant size
and position are reported. All surgical cases underwent clinical
and radiographic follow-up, with complete postoperative
reporting on 79 patients for one year, 46 patients for 2 years,
and 25 patients for 3 years.
Results: No
perioperative or immediate postoperative complications
necessitating surgery, such as revisions, infections, etc.,
occurred in the study group. In one case, the stem had to be
replaced after 12 months due to malpositioning. Intraoperatively,
there were 2 cases of stem fissure during implantation, both of
which were treated by wire cerclage. Subsequent migration was
not observed. In one case the stem migrated perioperatively, but
spontaneous consolidation ensued thereafter. The Harris Hip
Score (HSS) was 92.4 (SD 9.7) at 12 months, 93.8 (SD 11.9) at 24
months, and 94.2 (SD 10) at 36 months. The subjective assessment
of satisfaction by all patients was found to be "very satisfied"
or "satisfied" at 12 and 24 months. Only one patient was
unsatisfied with the outcome.
Conclusions:
Overall, this short hip stem prosthesis provides a useful
expansion to the prosthetic spectrum. The short-term results are
promising and the learning curve acceptable. Combined with a
ceramic bearing, it is a favorable option for young and active
patients.
J.Orthopaedics 2010;7(4)e8
Keywords:
arthroplasty; hip; short stem; Metha
Introduction:
The implantation of short stem prostheses in hip arthroplasty is
gaining in importance1. This is reflected by an
increasing number of surgical procedures, as well as an
increasing number of implant models available on the market1.
The anticipated advantages are seen in smaller sized implants
which help to reduce the loss of bone and support metaphysical
anchorage. In addition, the prostheses are also well suited to
implantation with less invasive procedures. There are drawbacks,
however, in that the implants are relatively new to the market
and consequently little data is available on early risks and
complications (learning curve). Long-term results are lacking
therefore1.
We report on our initial experience and results with the Metha
modular short hip stem prosthesis over a maximum follow-up
period of about 3 years, paying special attention to early
problems.
Materials
and Methods:
This study included all patients receiving a short hip stem
implant (Metha, B. Braun Aesculap, Tuttlingen/ Germany) in our
department between the beginning of July 2006 and March 2010.
All patients were under the care of one surgeon (HGS), underwent
conservative pre-treatment and were suffering from advanced,
painful coxarthrosis (stage IV) as evidenced clinically and
radiographically.
The exclusion criteria covered male patients aged over 68 and
female patients over 60, poor bone quality or anatomical
variants which complicate implantation of a short stem
prosthesis (severe Coxa vara or valga, severe antetorsion),
status post fracture of the coxal femur, post infection or post
tumor. In all cases planning ensued preoperatively, the surgical
approach was less invasive 1 and in a supine
position, and the implant position was basically controlled
intraoperatively by X-ray. Postoperatively, the patients were
asked not to strain the operated leg with more than 20 kg in the
first 6 weeks, after which they underwent radiographic
follow-up, and total loading was permitted.
All patients underwent clinical and radiographic follow-up in
order to identify all immediate perioperative complications. The
postoperative findings are recorded as Harris hip scores (1969)
1. The postoperative X-rays were analyzed in both
planes using the Gruen zone system (1979) 2. Zones 1,
2 and 6, 7 were defined on the coated area of the short stem,
and zones 3, 4 and 5 on the distal, uncoated area. Periarticular
ossification was classified according to Brooker (1973)3.
Results :
The study group includes 120 cases of short stem implant. Of all
treatments (n=120), the data in respect of surgery,
perioperative complications, implant size and position are
reported. All cases were monitored clinically and
radiographically for a follow-up period of at least 3 months and
maximally 36 months.
The mean age of the entire population (n=120) was 54 years
(35.9-67.3). There were 52 women and 56 men, with a mean weight
at the time of surgery of 88.2 kg (55-134), equivalent to a mean
BMI of 31 (23-47). The surgical indication was idiopathic
coxarthrosis in 72%, hip dysplasia in 18%, femoral head necrosis
in 6%, and other indications in 4%.
Postoperatively, full follow-up data are available for 79
patients at 12 months, 46 patients at 24 months, and 25 patients
at 36 months. The Harris Hip Score (HSS) was 92.4 points (SD
9.7) at 12 months, 93.8 points (SD 11.3) at 24 months and 94.2
points (SD 10) at 36 months postoperatively. The subjective
judgment of satisfaction by all patients in the group at 12 to
36 months was "very satisfied" in 75%, and "satisfied" in 24%.
Only one patient was dissatisfied with the outcome. 76.0% (91)
of patients claimed to have "no pain or ignorable pain", 16.0%
(19) "occasional or mild pain/minimal pain", and 8.1% (10)
described "tolerable or moderate pain". No patient had "serious
pain" or "total disability".
The mean degree of motion improved in
all patients by the last follow-up examination, reaching mean
values of 109 degrees of flexion (90-130 degrees), 36 / 0 / 19
degrees of abduction/adduction (10-60 / 10-30 degrees) and 20 /
0 / 27 degrees of inner rotation/outer rotation (5-40 / 10-40
degrees).
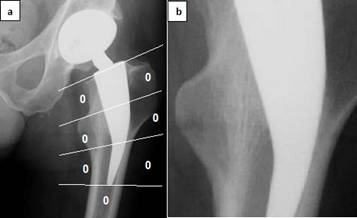
No radiolucencies are found at any time, in any patient, in the
Gruen zones of the metaphysically coated stem component (AP and
lateral projection) on radiographic analysis (Fig. 1a). In 75%
of cases (n=90) the tip of the implant reaches the lateral
corticalis on AP projection. In the transition of the coated
margin, 71% of cases reveal medial, and 62% lateral
densification zones at 12 months with alignment of the bone
structures (AP projection) to the implant surface. At 24 months,
82% of cases show medial, and 74% lateral densification zones.
Osteointegration, with reorientation of the trabeculae, was
found in all cases at 12 months (Fig. 1b).
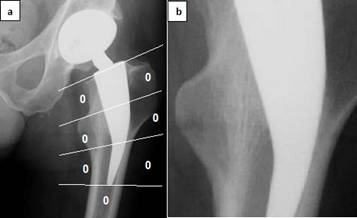
Fig. 1:
a) Lack of lucencies in the Gruen zones on 2-year follow-up. b)
Alignment of trabecular structures
Computer-assisted review of the postoperative pelvic imaging
revealed restoration of leg length in 107 cases, and leg
lengthening of up to 0.8 cm in 4 cases, 0.8-1cm in 6 cases, and
1 - 1.5 cm in 2 cases. In one case the stem had migrated
approximately 1cm during the 6 weeks postoperatively. No further
migration is seen in subsequent controls; the cause was found to
be an undersized implant. The patient is free of symptoms
(Fig.2).

Fig. 2:
Postoperative migration of stem with stabilization on follow-up
The majority of the implants proved to be of moderate size, as
described in the literature [[i]].
In 39.8% (48) of cases 130° neck adapters were used, in 53.4%
(64) 135°, and in 3.4% (5) 140°. Only
in 1.4% (1) was an antetorsion version, and in 2.2% (2) a
retrotorsion version selected. In 92.5% of cases
ceramic-on-ceramic bearings were chosen, and in 7.5% of cases a
PE-on-ceramic bearing whereby optimal positioning of the cup was
not always possible (Fig. 3).

Fig. 3:
AP and lateral view of a typical Metha short hip stem implant
No perioperative or postoperative complications necessitating
surgery, such as revisions, infections, etc., occurred.
Intraoperatively, stem fissure resulted in 2 cases during
implantation of the prostheses, both of which were medial in the
direction of the lesser trochanter. Both cases were treated by
wire cerclage. Subsequent migration was not observed. In one
case involving a heavily obese female patient, the consolidated
stem had to be replaced after about 12 months by a cementless
standard stem on account of postoperative, initially unnoticed
malpositioning and increasingly severe symptoms. Replacement
with a standard straight stem was possible without complications
(Fig. 4). Heterotopic ossification > Brooker 2 was not found in
this study.

Fig. 4:
Revision of a malpositioned short stem after 12 months, replaced
by a straight stem (CLS).
Discussion :
Our initial results with the Metha short hip stem prosthesis are
encouraging with a view to the perioperative rate of
complications. The learning curve is acceptable. Of the first
120 implantations, there were 2 stem fissures which could be
safely treated by cerclage and remained stable without the need
for further intervention. In one additional case the chosen
prosthesis was too small and resulted in migration of the stem
(Fig. 2). The implant stabilized spontaneously thereafter. As
experience was gained, fewer such problems arose. Fissuring of
the stem is also a well-known phenomenon with established
implant models, however. Only in one case the stem had to be
replaced as a result of initially unnoticed malpositioning in an
overweight female patient. Replacement with a standard straight
stem was possible in this case without complications. To begin
with, there was a relatively high percentage of suboptimal stem
positioning without lateral corticalis contact (25% of all
cases). All of these stems could be easily consolidated,
however. Introduction of a modified insertion instrument
rendered implantation of the prosthesis more straightforward and
reduced the likelihood of valgic implantation without guaranteed
lateral corticalis contact. After such modification, the tip of
the implant abuts with the lateral corticalis in virtually all
cases.
The clinical results, measured by Harris Hip Score and visual
analog scale for pain, are found to equate with the good results
already known for conventional and minimally invasive hip
arthroplasty [[i],
[ii],
[iii],
[iv]].
Harris hip scores of > 90 points were achieved at 12 and 36
months postoperatively. One fact which is certainly favorable is
the configuration of the prosthesis, which enables preservation
of bone stock at the greater trochanter area and facilitates a
minimally invasive approach while sparing the gluteal
musculature.
We recorded two cases of leg lengthening of over one centimeter
more than the opposite side using computer-assisted analysis of
the postoperative pelvic X-rays. Severe bilateral dysplasia of
the hip joint was found in one of these clinically significant
cases. The lengthening was accepted on the reasons of stability.
Since the femoral ring should be completely preserved for the
purpose of primary stability, restoration of leg length may
entail certain problems since extension tends to result from a
short femoral neck due to the inevitable preservation of the
femoral ring even when using a short head. This should be
considered during preoperative planning.
Overall, this short hip stem prosthesis provides a useful
expansion to the prosthetic spectrum. The short-term results are
promising and the learning curve acceptable. Its design enables
preservation of the bone stock of the greater trochanter and
selection of an approach which conserves the soft tissue. The
alignment of the bone structures appears to confirm the
assumption of proximal force transmission, as was also shown by
the Santori et al. study team [[v]].
Combined with a ceramic bearing, it is a promising option for
young and active patients [[vi],
[vii]].
However, patients need to be fully informed that so far no
long-term results are available for such an implant.
Reference:
-
Buecking PK, Feldmann P, Wittenberg R. Metha - Modulare
Kurzschaftprothese. Orthop. Praxis 2006; 8: 474-477
-
Morrey BF, Adams RA, Kessler M. A conservative femoral
replacement for total hip arthroplasty. A prospective study. J
Bone Joint Surg Br. 2000; 82(7):952-958
-
Stukenborg-Colsman C. Schenkelhalsendoprothesen. Orthopäde
2007; 36(4):347–352
-
Hube R, Zaage M, Hein W, Reichel H. Frühe
funktionale Ergebnisse einer Kuzschaftprothese des Hüftgelenks
mit metaphysär-intertrochantärer Verankerung. Orthopäde 2004
Nov;33(11):1249-1258
-
Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement:
the factors governing bone ingrowth, stress shielding and
clinical results. J Bone Joint Surg 1987; 69-B: 45-55
-
C. V. Albanese, Lucidi M, Rendine M, Santori N, Pavan L,
Passariello R, Santori FS. Effect on bone mineral density of
progressive shortening of the femoral stem in a short stemmed
prosthesis evaluated by DXA. JBJS Britisch Volume 2009, V91-B,
Issue suppl_I, 145
-
Wollmerstedt N,
Nöth U,
Mahlmeister F,
Lotze A,
Finn A,
Eulert J,
Hendrich C. Aktivitätsmessung von Patienten mit
Hüfttotalendoprothesen.
Orthopäde 2006; 35(12):1237-45
-
Eben R. Walk B. Summer S. Maier M. Thomsen P. Thomas.
Implantatallergieregister – ein erster Erfahrungsbericht.
Orthopäde 2009, 38:557–562
|