|
Abstract:
The purpose of this study was to clarify the natural history of
the supero-lateral bipartite fragment of the patella in
children. Twenty-three patients with bipartite fragment of the
patella (27 knees) under 15 years old at initial examination
were followed until they were over 16 years old. Among them,
spontaneous bone union of bipartite fragment was gained in 13
knees (united group) and not gained in 14 knees (non-united
group). These bipartite fragments of the united group were
thought to be accessory ossification centers of the patella and
these of the non-united group were thought to be usual bipartite
patellas. The gap between the bipartite fragment and body of
patella of the united group at initial examination (median; 1
mm, range 1-2 mm) was significantly narrower than that of the
non-united group (median; 3 mm, range 2-4 mm) (p<0.0001).
Therefore, the development of bipartite patella may be predicted
in bipartite fragments with large gap.
J.Orthopaedics 2010;7(4)e5
Keywords:
bipartite fragment; accessory ossification center; bipartite
patella; natural history; bone union; children.
Introduction:
As the ossification center of the patella enlarges, the
expanding margins become irregular and associated with accessory
ossification centers and these are most common supero-laterally1.
Bipartite patella is supposed to be developed from a failure of
an accessory ossification center of the patella to unite with
the main portion of the patella1-5. However, it is
not clear why an accessory ossification center of the patella
fail to unite with the main portion of the patella. Until now,
few authors reported the differences between supero-lateral
accessory ossification center and bipartite patella. Therefore,
it is important to clarify the natural history of the supero-lateral
bipartite fragment of the patella in children.
The purpose of this study was to clarify the natural history of
the supero-lateral bipartite fragment of the patella in
children. Our hypothesis was that development of bipartite
patella would be predicted in bipartite fragments with large
gap.
Materials
and Methods:
Forty patients (46 knees) with bipartite fragment of the patella
under 15 years old at initial examination were examined by the
first author between 1973 and 2007. Among them, those patients
who could be followed until they were over 16 years old without
any interventions were included in this study. Five patients (7
knees) were lost to follow up and those patients were excluded.
Fragments of 10 bipartite and 2 tripartite patellae were excised
at surgery due to pain in 12 patients and those patients were
also excluded. Surgical treatment was considered for those
patients who had failed to respond to at least 3 months of
conservative treatment, including rest and restriction of sports
activities. In all those operated patients, tenderness over the
supero-lateral or lateral aspect of the patella disappeared
within 4 weeks after surgery and all returned to their previous
sports activities at 2 months. Finally, twenty-three patients
(27 knees) were included in this study. Accessory ossification
center is defined as asymptomatic bipartite fragment that will
unite spontaneously without any intervention until 16 years of
age. Bipartite patella is defined as a bipartite fragment that
will not unite spontaneously over 16 years of age. Symptomatic
bipartite patella is defined as both pain at the separated
fragments during or after strenuous activity and localized
tenderness over the separated fragments6.
Asymptomatic bipartite fragment is defined as an incidental
finding when the knee is radiographed for other reasons.
According to a classification for developmental anomaly of
ossification type bipartite or tripartite patellae6,
all bipartite fragments were supero-lateral bipartite type. In
those patients, both bone union of the bipartite fragment and
symptoms at initial examination and at follow-up were
investigated. The gap between the bipartite fragment and the
body of patella at initial examination was measured in
1-millimeter increments at the widest gap by a ruler on AP
roentgenograms. All measurements were made once by the same
observer (Yoshikazu Oohashi).
Statistical analysis
The measured gap between bipartite fragment and the body of
patella did not follow a normal distribution; therefore,
non-parametric the Wilcoxon Rank Sum test with the R program was
used. All analyses were two-tailed, and p<0.05 was considered
statistically significant. Differences in proportions of the
bone union of bipartite fragment between symptomatic and
asymptomatic bipartite fragment were analyzed using Fisher’s
exact probability test with the R program. P<0.05 was considered
statistically significant.
Results :
Spontaneous bone union of bipartite fragment was seen in 13
knees (11 patients) (united group) (Fig.1). These bipartite
fragments of the united group were thought to be accessory
ossification centers of the patella. The mean age at initial
examination was 11.3±1.5 years (range, 7 years 9 months to 12
years 9 months). Mean age of patients with bone union of the
bipartite fragment was found to be 12.9±1.2 years (range, 10
years to 14 years 7 months) (Fig.2). Mean follow-up period of
patients until bone union was observed was 2.1±1.2 years (range,
8 months to 3 years 11 months). The gap between the bipartite
fragment and body of patella of the united group (13 knees) at
initial examination was 1-2 mm (median, 1 mm). Eight were male
and 3 were female. All 13 bipartite fragments that united were
asymptomatic.
Spontaneous bone union of bipartite fragment was not obtained in
14 knees (12 patients) (non-united group) at final examination
at mean age of 17.9±2.6 years (range, 16 years to 24 years 1
month) (Fig.3). These bipartite fragments of the non-united
group were thought to be usual bipartite patellas. The mean age
at initial examination was 13.9±0.7 years (range 13 years to 15
years 5 months). Mean follow-up period was 3.9±2.8years (range,
1 year 4 months to 10 years 9 months). The gap between the
bipartite fragment and body of patella (14 knees) at initial
examination was 2-4 mm (median, 3 mm). All were male. Among
them, ten bipartite patellae (8 patients) were symptomatic and 4
(4 patients) were asymptomatic at initial examination; however,
4 bipartite patellae (3 patients) were symptomatic and 10
bipartite patellae (9 patients) were asymptomatic at final
examination.
The gap between the bipartite fragment and body of patella at
initial examination of the united group was significantly
narrower than that of the non-united group (p<0.0001) (Table 1).
Bone union of the bipartite fragment was seen more frequently in
asymptomatic bipartite fragments (13 of 17 patellae, 76%) than
that seen in symptomatic bipartite fragments (0 of 10 patellae,
0%) (p<0.001).

a.
b.
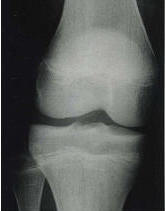
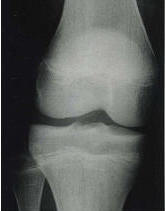
Fig.1 Radiographs of a girl with asymptomatic supero-lateral
bipartite fragment of the right knee (united group)
a. Antero-posterior radiograph showing a bipartite fragment of
patient at 12 years, 7 months old. The gap between the bipartite
fragment and body of the patella is 1- mm (arrow).
b Antero-posterior radiograph showing union of the bipartite
fragment in the same patient at 13 years, 6 months old.
Fig.2 Frequency of bone union of the bipartite fragment noted by
age.
The peak incidence is seen in 13-year-olds.
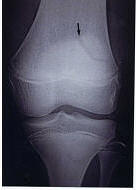 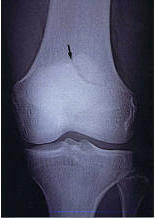
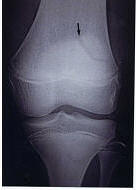
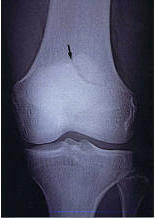
Fig.3 Radiographs of a boy with a symptomatic supero-lateral
bipartite fragment of the left knee (non-united group).
a. Antero-posterior radiograph showing a bipartite fragment at
13 years, 10 months old. The gap between the bipartite fragment
and body of the patella is 2-mm (arrow).
b Antero-posterior radiograph of the same patient showing a
bipartite patella (arrow) at 22 years, 9 months old.
Discussion :
The most important finding of the present study was that the gap
between the bipartite fragment and body of patella of the united
group was significantly narrower than that of the non-united
group. Furthermore, bone union of the bipartite fragment was
seen more frequently in asymptomatic bipartite fragment than
that seen in symptomatic bipartite fragment.
Several theories have been proposed to explain the development
of bipartite patella. Ogden et al. suggested etiology involving
a traumatically induced, chondroosseous disruption of the
superolateral pole of the incompletely ossified patella,
analogous to Sinding -Larsen-Johansson or Osgood-Schlatter’s
disease7. Furthermore, van Holsbeeck et al. reported
four patients with an association of a dorsal defect of the
patella and a multipartite patella and they suggested a common
genesis for these two ossification variants by which the
traction lesion at the insertion of the vastus lateralis muscle
plays an important role8 . Although Devas presented a
symptomatic superolateral fragment as a result of stress
fracture9 , Bourne et al. described that his evidence
was not convincing [3]. Until now, the more likely explanation
is that bipartite patella is a failure of an accessory center of
ossification to unite with the main portion of the patella1-5
. However, it is not clear why an accessory ossification center
of the patella fail to unite with the main portion of the
patella. Present study may suggest that supero-lateral accessory
ossification center that gap between the bipartite fragment and
body of patella is greater than 2mm may remain separate and lead
to bipartite patella.
A few cases have been reported in which knees that appeared
normal on radiograph later developed an acute fracture of the
superolateral patella10 or bipartite patella7,
or late appearance of accessory ossification center3,11.
Echeverria et al. reported a rare case of an acute fracture of
the superolateral patella in a 17-year-old high school soccer
player10. X-ray films of his same knee 10 weeks
before injury were normal and they concluded that the lesion
seen at this injury represent an acute fracture 10.
Bourne et al. reported a case in which knee that appeared normal
on radiograph later developed bipartite patella and described
that delayed ossification of the accessory ossicle is a possible
explanation in such case 3. Similarly, Zumstein et
al. also reported a case of bilateral radiographic progression
of the supero-lateral fragment of a bipartite-into a tripartite
patella and they concluded etiology involving a late appearance
of a third ossification center11.
On the other hand, bone union of bipartite patella in children
and adolescents has been reported following procedures to reduce
traction force of the vastus lateralis muscle on the bipartite
fragment12-14 or after treatment with low-intensity
pulsed ultrasound15 or after treatment with cast
immobilization7. Adachi et al.
reported arthroscopic vastus lateralis release in patients with
an average age of 13.8 years, resulting in 64.7% bone union, and
bone union in patients 15 years or younger was significantly
better than that seen in patients over 15 years of age14.
Ogden et al. also reported the incorporating the accessory
center into the main patellar ossification center after cast
immobilization for 3 weeks in a 12-year-old boy7.
However, present study shows that it is necessary to distinguish
symptomatic bipartite patella from supero-lateral accessory
ossification center that unite spontaneously when such
treatments are considered in children and adolescents.
According to the natural history of the symptoms of bipartite
patella, few studies have been reported. In present series,
among symptomatic bipartite patella under 15 years old at
initial examination, only a few were symptomatic at the
follow-up. Therefore, it is necessary to investigate long-term
symptom amelioration.
This study has several limitations. First, the number of cases
investigated in this study is small and a further randomized
controlled study is needed. Second, the gap between the
bipartite fragment and the body of patella was measured in
1-millimeter increments on roentgenograms by the same observer
(Yoshikazu Oohashi) and all measurements were made only once.
Therefore, there was not a study of inter- and intra-personal
validity.
Conclusion:
Development of bipartite patella may be predicted in patients 14
years old or younger, particularly in symptomatic bipartite
fragments in which the gap between the bipartite fragment and
the body of patella is more than 2mm.
Reference:
-
Ogden J.A. Radiology of postnatal skeletal development. X.
Patella and tibial tuberosity. Skeletal Radiol 1984; 11:
246-257.
-
Adams JD, Leonard RD. A developmental anomaly of the patella
frequently diagnosed as fracture. Surg Gynecol Obstet 1925;
41:601-604.
-
Bourne MH, Bianco AJ. Bipartite patella in the adolescent:
Results of surgical excision. J Pediatr Orthop 1990; 10:69-73.
-
George R. Bilateral bipartite patellae. Br J Surg 1935;
22:555-560.
-
Oohashi Y, Noriki S, Koshino T, Fukuda M. Histopathological
abnormalities in painful bipartite patellae in adolescents.
The Knee 2006; 13:189-193.
-
Oohashi Y, Koshino T, Oohashi Y Clinical features and
classification of the bipartite and tripartite patella. Knee
Surgery, Sports Traumatology, Arthroscopy in press. DOI
10.1007/s00167-010-1047-y.
-
Ogden JA, McCarthy SM, Jokl P. The painful bipartite patella.
J Pediatr Orthop 1982; 2:263-269.
-
van Holsbeeck M, McCally WC. Dorsal defect of the patella:
concept of its origin and relationship with bipartite and
multipartite patella. Skelet Radiol 1989; 16:304-311.
-
Devas MB. Stress fractures of the patella. J Bone Joint Surg
Br 1960; 42:71-74.
-
Echeverria T S, Bersani F A.
Acute fracture simulating a symptomatic bipartite patella.
Report of a case.
Am J Sports Med 1980; 8:48-50.
-
Zumstein M, Sukthankar A, Exner G U. Tripartite patella: late
appearance of a third ossification center in childhood. J
Pediatr Orthop B 2006; 15:75-76.
-
Ogata K. Painful bipartite patella. A new approach to
operative treatment. J Bone Joint Surg Am 1994; 76:573-578.
-
Mori Y, Okuno H, Iketani H, Kuroki Y. Efficacy of lateral
retinacular release for painful bipartite patella. Am J Sports
Med 1995; 23:13-18.
-
Adachi N, Ochi M, Yamaguchi H, Uchio Y, Kuriwaka M. Vastus
lateralis release for painful bipartite patella. Arthroscopy
2002; 18:404-411.
-
Kumahashi N, Uchio Y, Iwasa J, Kawasaki K, Adachi N, Ochi M.
Bone union of painful bipartite patella after treatment with
low-intensity pulsed ultrasound: Report of two cases. The Knee
2008; 15: 50-53.
|