|
Abstract:
Objective:The
aim of this study was
to asses the relationship between meniscal extrusion and the
joint space loss with meniscal tears in patients under 60 years
old
Materials and methods:The
study group consisted of 108 of 623 patients ( 73 female, 35
male) (mean age 43.14 ± 7.01) with meniscal extrusion and 60
patients (29 female, 31 male) (mean age 47.04 ±7.8) without
meniscal extrusion as control group under 60 years old.
Results:A
statistically significiant association was found between the
medial meniscal extrusion and the posterior horn of medial
meniscal tear in the study group. Statistically significant
medial joint space narrowing was found in both the study and
the control group. Statistically significiant lateral joint
space widening was detected in the study group when compared to
control group. Also lateral joint space widening was found to
have been directly affected from the degree of meniscal
extrusion.
Conclusion: Medial
meniscal extrusion greater than 3 mm is significantly associated
with radial and oblique tears which results in disruption of
meniscal stability. Also as in occur in menisectomies, medial
meniscal extrusion may results in tendency to varus alignment
that results in an increased stress in the medial compartment
which is known to be a major factor in the development of medial
gonarthrosis.
J.Orthopaedics 2010;7(4)e2
Keywords:
MRI; Meniscal Extrusion; Joint space
Introduction:
The meniscus is essential for distributing axial forces on the
knee through its hoop mechanism. The absence of the meniscus
increases the peak pressure in the knee joint. Resection of as
little as 15–34% of the meniscus increases contact pressures by
more than 350%(1,2).
Medial meniscal extrusion (MME) has been defined as pathologic
displacement (>3 mm) of the peripheral edge of the medial
meniscus beyond the central margin of the medial tibial
plateau(3). MME has been demonstrated to occur with tears of
the medial meniscal root, radial tears, complex tears, meniscal
degeneration and degenerative joint disease(4). In the setting
of MME, the meniscus is no longer able to redistribute and
transmit load. Increased stresses are transferred to the
femorotibial articular cartilage, leading to degenerative
articular cartilage wear, flattening of the femoral condyles and
osteophyte formation. The aim of this study was to asses the
relationship between meniscal extrusion and the joint space
width and also correlate with meniscal tears in a large
patient population younger than 60 years old.
Materials
and Methods:
An experienced musculoskeletal radiologists retrospectively
reviewed the 1.5-T MR scans of 9568 knees in 9148 consecutive
patients between April 2008 and June 2009. All study procedures
were approved by the local ethical committee. Of the 623
patients with medial meniscal extrusion, 108 patients ( 73
females and 35 males; mean age 43.14 ± 7.01 years) were included
in the study group. Control group was consisted of 60 patients
(29 females and 31 males; mean age 47.04 ±7.8 years) without
meniscal extrusion. Exclusion criterias were the presence of
severe osteoarthritis, complex meniscal tears, chondrocalcinosis
or signs of trauma and acute or chronic infections. All MR
imaging were performed using one of the two 1.5 T MR scanner
(Integra and Achieva, Philips Medical Systems, Netherland)
equipped with dedicated knee coil. All studies were performed
using coronal oblique fat supressed T2 (TR range / TE range ,
4500-5000/60-92), and proton dansity (PD) weighted image (TR
range / TE range , 3000-4500/25-35), sagittal proton dansity (TR
range / TE range, 1200-1500/6-12) and T2 weighted (TR range /
TE range , 1200-1500/80-95) dual spin echo, axial fat supressed
PD images (TR range / TE range , 4500-5000/25-35) with a 4 mm
section thickness and 0,4 mm gap. The total acquisition time was
between 15 and 20 minutes. A field of view of 16-18 cm with a
matrix size of 256x256 was used for all images. Three
measurements were done and the mean of these three measurements
was recorded for each patient.
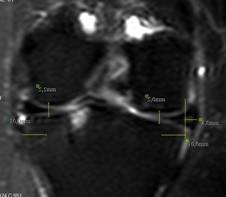
In the coronal plane, extrusion measurements were made using the
technique described by Breitenseher et al (5). The criterion for
meniscal extrusion was a distance of 3 mm or more between the
peripheral border of the meniscus and the central margin of the
tibial plateau as measured in the coronal plane (Figure 1). A
distance of less than 3 mm was not considered as meniscal
extrusion. Also the medial and lateral tibiofemoral joint spaces
of the knees of each patient were measured separately at the
level of tibial medial eminencia (Figure 1). Cartilage was
scored as being either normal or abnormal (partial or full
thickness defects as abnormal) on both the femoral and tibial
sides of the joint by the review of T2 and proton density
images.
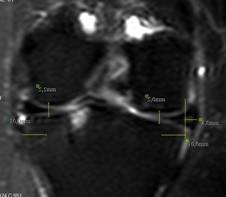
Figure 1: Measurement of meniscal extrusion,
lateral and medial joint space in 45 years old woman. Coronal
Turbo spin-echo ( TSE) T2 weighted image (TR/TE, 4620/72) of
right knee obtained through mid portion medial femoral condyle.
Vertical line (yelllow line) is drawn intersecting margin of
medial tibial plateau at the site of transition from horizontal
to vertical. Extrusion is measured from this line to outer edge
of meniscus. At the same slice, Medial and lateral joint spaces
are measured separately approximately 1 cm away from outer
edge of tibia. Horizontal tear at posterior horn of medial
meniscus and ostechondral lesion in the lateral plateau of tibia
(arrow) are seen.
An internal meniscal signal extending to the articular surface
was considered as meniscal tear. Meniscal tears were classified
into one of five configurations using previously described
criteria (6) (Figure 2, 3). A tear parallel to the tibial
plateau separating the meniscus into upper and lower parts was
considered as horizontal tear; which is vertical (perpendicular
to the tibial plateau) and propagating parallel to the main
(circumferential) axis of the meniscus as longitudinal tear;
which is vertical and propagating perpendicular to the main axis
as radial tear and which are intermediate tears between
horizontal and vertical as oblique,flap or parrot-beak tears.
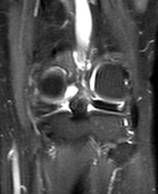

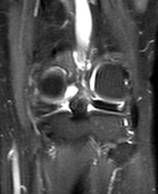
Figure 2: 53-year-old man with radial root tear of
posterior horn of medial meniscus on coronal PD image with fat
saturation (TR/TE 3948/30) and (b) sagittal PD image ( TR/TE
1692/6)


Figure 3: 24 year old man with oblique tear of posterior
horn of medial meniscus on coronal PD image with fat saturation
(3948/30) and (b) sagittal PD ( TR/TE 1692/6) image.
Medial and lateral joint space width was seperately compared
with meniscal extrusion level, meniscal tears and cartilage
defects. Results of of study group was also compared with the
results of control group.
Statistical analysis was performed by using SPSS for Windows
release 11.5 ( Chicago IL, USA ) software. Chi-square test is
used for
categorical data and Student’s t test is used for comparing
independent groups.
A paired t test was used to compare the joint space width
between medial and lateral sides in each group. Statistical
significance level was set as P value < 0.05.
Results :
In 92% of patients of the study
group, meniscal tears were detected. 55 (50,9%) radial (mostly
root tear), 29 (26,9%) oblique, 6 (6.5%) bucket handle, 2 (1.9%)
longitidunal and 2 (1.9%) horizontal tear were detected in the
study group (Table 1). Mean extrusion value was 4.1417 mm (±
0,778) in study group (Table 2). A statistically significiant
association was found between the medial meniscal extrusion and
the radial and oblique tears at posterior horn of medial
meniscus in the study group (in 88% of the knees) (P<0,001).
No association was found between the anterior horn and the
body tear.
|
|
number |
Meniscal tear |
Radial |
Oblique or Flap |
horizontal |
longitidinal |
Bucket Handle |
|
Study |
108 |
94
(% 88) |
55
(% 50.9) |
29
(% 26.9) |
2
(% 1.9) |
2
(% 1.9) |
6
(% 6.5) |
|
Control |
60 |
13
(% 21.6) |
3
(% 5) |
5
( % 8.3) |
4
(% 6.6) |
1
(%1.6) |
|
Table 1:
Number of Patients and Frequency of
Meniscal Tear Type in Both Groups
Mean medial and lateral joint space
width were 3.27mm (±0,93) and 4.26 mm (±1,12) respectively in
the study group, and 3,61mm (±0,85) and 3,86 mm ( ±0.77)
respectively in the control group. Statistically significant
medial joint space narrowing and lateral joint space widening
was found in the study group in comparision to that of control
group. . Statistically significant narrowing was detected in
medial joint space in comparison to lateral joint space both in
the study (p<0,001) and in the control group (p <0,01).
Correlation coefficients were as 0,692 in the study and 0,652 in
the control group. No correlation was found between medial joint
space narrowing and MME degree. Statistically significiant
lateral joint space widening was detected in the study group
when compared to the control group (p < 0.05). Lateral joint
space widening was also found to be directly affected from the
degree of meniscal extrusion (Table 2). (r=0,206) (p<0,05).
Cartilage defects was detected in 28 of 108 patients of the
study group. There was no statistically significant relation
between the joint space narrowing and the cartilage defects or
thinning in the femur medial condyle.
|
|
Extrusion Degree
(mm) |
Medial Joint Space (mm) |
Lateral Joint Space
(mm) |
|
Study |
4,417 |
3,27 |
4,26 |
|
Control |
0 |
3,61 |
3,86 |
Table 2:
Mean Value of extrusion degree , Medial and Lateral Joint
Space
Discussion :
In this study we found an asymetric joint space narrowing (JSN),
as narrowing of the medial compartment and widening of the
lateral compartment, due to the meniscal extrusion. A
significiant association was found between the medial meniscal
extrusion and the posterior horn of medial meniscal tear in
the study group. Joint space narrowing was not seemed to be
affected by the cartilage defects.
As found in our study, Kesmezacar et al. reported that narrowing
of medial compartment and widening of lateral compartment of
knees in which medial menisectomy was done. Also they stated
that significiant increase in the varus of knees was observed
after partial menisectomy(7). Also significant narrowing of
medial joint space was observed in the study of rabbit model
of total menisectomy which was conducted by Mesner et al. They
reported that removal of the medial meniscus led to a permanent
narrowing without resulting in any cartilage changes(8). The
degree of varus (bowing) present in a knee joint is a
combination of the geometric alignment of the femur and tibial
(congenital), and the degree of narrowing in the medial
compartment (due to loss of cartilage and/or bone), and/or
widening of the other joint space compartments (due to ligament
laxity or injury to other soft tissue structure. Any medial
displacement occurring in the gravity center of the body results
in an increased stress in the medial compartment, which is known
to be a major factor of medial gonarthrosis (9,10). Sharma et
all reported that varus alignment increases the risk of medial
osteoarthritis progression, that valgus alignment increases the
risk of lateral osteorthritis progression. Also they stated that
severity of varus was correlated with greater medial joint space
loss, severity of valgus was correlated with lateral joint
space loss in a 18 month period (11). We didn’t measure varus
and valgus angle which was one of limitation of our study but
theoretically, the decrease in the medial and the increase in
the lateral joint space which was detected in our study will
probably increase the varus alignment which can increase
osteoarthritis progression at the medial joint space.
Widening of lateral compartment is also seen in knees with
discoid lateral meniscus. Discoid lateral meniscus was not
detected in our patientss
Asymetric joint space narrowing (JSN) was detected in our study.
When JSN is detected, it is important to differentiate
inflammatory from degenerative causes. Asymetric JSN is seen in
osteoarthritis, especially involving medial femorotibial
compartment. In the previous studies, joint space narrowing of
knee has been linked to loss of articular cartilage. However
meniscal damage also contributes to joint space narrowing
(12,13,14). Previous studies have reported that changes in the
articular cartilage in the medial tibiofemoral compartment were
less marked, even where there was a linear correlation between
mean cartilage volume and radiographic JSN. Radiographic JSN is
not a reliable tool for assessing cartilage status in patients
with early osteoarthritis. Joint space narrowing was not
affected by the cartilage defects in our study as reported in
some previous studies. Adams et al, who conducted a study in
patients older than 60 years with osteorthritic knees, reported
that early narrowing of the joint space observed on conventional
radiographs (Kellgren 1-3) appears to be a function of meniscal
extrusion rather than loss of articular cartilage, but joint
space narrowing in advanced disease (Kellgren 4) was appears to
be related primarily to loss or changes in articular cartilage
(15).
Also significant association was found between the medial
meniscal extrusion and the tear of posterior horn of medial
meniscus, especially of radial and oblique. In a study of
Costa et al, which was conducted in patients aged between 34- 83
years (mean age 56 years), it was reported that major medial
meniscal extrusion (>3mm) was associated with a tear of
medial meniscus especially of radial tear(4). Kenny published
a study relating radial displacement of medial meniscus and
“Fairbank’s” signs. These concern three radiographic
abnormalities in the knee after meniscectomy, as a result of
loss of meniscal function: an anteroposterior osseous ridge
projecting downward from the femoral condyle, generalized
flattening of the marginal half of the femoral articular
surface, and narrowing of the joint space. Kenny concluded that
these abnormalities could develop in knees with radial
displacement (i.e., extrusion) of the medial meniscus and loss
of meniscal function. Also, unstable meniscal tears have been
associated with development of osteoarthritis ( 16, 17). As
detected in our study, Mage et al and Lerer et al found that
radial or root tear was strongly associated with meniscal
extrusion (3,18). However no association was found between
oblique tear and meniscal extrusion in these studies. Only in a
study of Costa it was found that oblique tears was associated
with minor extrusion that was less than 3 mm. Contrary to the
previously reported findings , we found a statistically
significant association with oblique tear and MME. Oblique or
flap tears which represent a composite of a longitudinal and
radial tear, start on the free edge of the meniscus and will
extend to the meniscal fibrocartilage. They are the most common
type of meniscal tear (19,20), Flap tear frequently develops
after minimal meniscal trauma superimposed on a degenerative
process resulting from chronic shear forces. Usually, they have
either a predominantly horizontal or vertical component with
some degree of distruption of meniscal structure, which can
result in meniscal subluxation.
There are some limitations in our study. Since our study was a
retrospective study, we had no reference or gold standard
because MRI was used as the surrogate documentation of the
abnormality. The absence of arthroscopic confirmation of our
findings could also represent a limitation. A selection bias
exists because these cases were selected on the basis of the
presence of some degree of extrusion.
To conclude, medial meniscal extrusion is significantly
associated not only with radial tears and also with oblique or
flap tears which results in disruption of meniscal stability.
Also as in occur in menisectomies, decrease in medial and
increase in lateral comparment of knee joint was found in our
study. These changes may results in tendency to varus alignment
that results in an increased stress in the medial compartment
which is known to be a major factor in the development of medial
gonarthrosis. Also widening of lateral comparment was directly
affected by extrusion degree but narrowing of medial comparment
wasn’t affected.
Reference:
-
Rennie WJ, Finlay DB. Meniscal extrusion in young athletes:
associated
knee joint abnormalities. AJR Am J Roentgenol. 2006
Mar;186(3):791-94.
-
Baratz ME, Fu FH, Mentago R. Meniscal tears: the effect of
meniscectomy and of repair on intraarticular contact areas and
stress in the human knee—a preliminary report. Am J Sports
1986; 14:270–275.
-
Lerer DB, Umans HR, Hu MX, et al. The role of meniscal root
pathology
and radial tear in medial meniscal extrusion. Skeletal Radiol
2004;33:569–74.
-
Costa CR, Morrison WB, Carrino JA. Medial meniscal extrusion
on
knee MRI: Is extent associated with severity of degeneration
or type of tear?
American
Journal Radiol 2004; 183:17–23.
-
Breitenseher MJ, Trattnig S, Dobrocky I, et al. MR imaging of
meniscal
subluxation in the knee. Acta Radiol1997; 38:876 -879.
-
Won-Hee Jee, Thomas R. McCauley, Jung-Man Kim, Dong-Jin Jun,
Young-Joon Lee, Byung-Gil Choi, and Kyu-Ho Choi Meniscal Tear
Configurations: Categorization with MR Imaging Am. J.
Roentgenol.,
Jan 2003; 180: 93 - 97.
-
Hayrettin Kesmezacar, M.D.,1 R›fat Erginer, M.D.,1 Tahir Ögüt,
M.D.,1 Ali Uzpak, M.D.,1 Turgut Dinçal, M.D.,1 Günay Can,
M.D.,2 Muharrem Babacan, M.D. Clinical and radiographic
results
of arthroscopic partial meniscectomy Artroskopik parsiyel
menisektominin klinik ve radyografik sonuçlar.
Joint Dis Rel Surg 2006;17(1):21-27
-
Messner K,
Fahlgren A, Persliden J, Andersson BM. Radiographic
joint
space narrowing and histologic changes in a rabbit
meniscectomy
model of early
knee osteoarthrosis. Am J Sports Med 2001;29:151-60
-
Allen PR, Denham RA, Swan AV. Late degenerative changes
after meniscectomy. Factors affecting the knee after
operation.
J Bone Joint Surg [Br] 1984;66: 666-71
-
Odenbring S, Lindstrand A, Egund N, Larsson J, Heddson B.
Prognosis for patients with medial gonarthrosis.A 16-year
follow-up study of 189 knees. Clin Orthop Relat Res
1991;(266):152-5
-
harma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD.
The role of knee alignment in disease progression and
functional
decline in knee osteoarthritis. JAMA. 2001 Jul
11;286(2):188-95
-
Hunter DJ, Zhang YQ, Tu X, et al. Change in joint space width:
hyaline articular cartilage loss or alteration in meniscus?
Arthritis Rheum 2006;54: 2488–2495
-
Sugita T,
Kawamata T, Ohnuma M, Yoshizumi Y, Sato K.
Radial displacement of the medial meniscus in varus
osteoarthritis
of the knee. Clin Orthop 2001;387: 171–177.
-
Gale DR, Chaisson
CE, Totterman SM, Schwartz RK,
Gale ME, Felson D. Meniscal subluxation: association with
osteoarthritis and joint space narrowing. Osteoarthr Cartil
1999;7: 526–532.
-
Adams JG, Mc Alindon T, Dimasi M, Carey J, Eustace S:
Contribution of meniscal extrusion and cartilage loss to joint
space narrowing in osteoarthritis. Clin Radiol 1999, 54:
502-506
-
Kenny C. Radial displacement of the medial meniscus and Fairbank's signs.
Clin Orthop Relat Res. 1997 Jun;(339):163-73
-
Fairbank TJ. Knee joint changes after meniscectomy. J Bone
Joint Surg [Br] 1948;30:664-70
-
Magee T. MR findings of meniscal extrusion correlated with
arthroscopy. J Magn Reson Imaging 2008 Aug; 28(2):466-70
-
Zanetti M, Pfirrmann CW, Schmid MR, Romero J, Seifert B,
Hodler J. Patients with suspected meniscal tears: prevalence
of abnormalities seen on MRI of100 symptomatic and 100
contralateral asymptomatic knees. AJR Am J Roentgenology 2003
Sept; 181(3) 635-41
-
Stoller D.W,Li A.E, Anderson LJ, Cannon WD. The Knee. In:
David W Stoller ed. Magnetic Resonance Imaging In Orthopaedics
And Sports Medicine. 3 rd ed.
-
Baltimore: Lipincolt Williams&Wilkins, 2007. 305-731
|