|
Abstract:
Aseptic
nonunions in distal
tibia are particularly challenging due to the short distal
segment and fragile nature of the local soft-tissue envelope,
particularly after type-Ⅱand
type-Ⅲtibia open fractures. Although many
internal-fixation options have been described for the treatment
of distal tibia nonunions after open fractures, these were
firstly preferred to manage with external fixators. We have
attempted to compare a subset of distal tibia nonunions after
tibia open fractures treated by Locking Compression Plates or
Unilateral External Fixators. From February 2007 to February
2010, we retrospectively reviewed 37 patients (30 men and 7
women) with aseptic nonunions in distal tibia treated by Locking
Compression Plates (n=15) and Unilateral External Fixators(n=22).
Iliac crest autogenous bone grafting was performed in all
patients during the internal or external fixation. The outcome
measures included the rates of union, time to union, malunion,
lasting nonunion, infection and scores of AOFAS. Although the
LCP group had a longer time to union, it got a higher union
rate, lower complications and better foot and ankle functions.
These differences excepting the scores of AOFAS were showed
statistically significant by SAS V8.1 Software (P=0.0107<0.05).
Thus, based on our limited study, LCP can be performed as the
excellent inter-fixator in distal tibia aseptic nonunions for
higher union rates and lower complications. Future larger number
of samples and prospective randomized trials are required to
analysis the advantages and disadvantages of this inter-fixator
in the treatment for these challenging nonunions.
J.Orthopaedics 2010;7(4)e11
Keywords:
Aseptic Nonunion; Distal Tibia; Locking Compression plate;
Unilateral External Fixator; Iliac Crest Autogenous Bone
Grafting
Introduction:
The
incidence of nonunions for tibia is higher than other long bone
fractures. Nonunions for type-Ⅱand
type-Ⅲ open tibia fractures was reported
as 14% by Edwards and Jaworski1. Presenting factors
that have been reported to contribute to nonunions include
fracture displacement, bone loss, associated soft-tissue
injuries and infection.
The nonunion rates for distal tibia fractures were reported as
17%2. Nonunions in distal
tibia are particularly challenging due to the short distal
segment and fragile nature of the local soft-tissue envelope,
particularly after prior surgery. Before the introduction of the
inter-fixation for distal tibia open fractues, these nonunions
were preferred to manage with external fixation. This technique
gained widespread acceptance because of the ease appliance and
minimal obstruction to soft tissue. However, several studies
have demonstrated this preferable management with high rates of
pin loosening, malunion and lasting nonunion3,4,5.
Although Locking Compression Plates with minimal invasion and
stable internal fixation have been widely used in clinic for
long bone fractures and nonunions, few paper reported their
efficacy for distal tibia nonunions. We made a small sample
study to compare the treatment of Locking Compression Plate with
Unilateral External Fixator for distal tibia nonunions in our
orthopedic center from February 2007 to February 2010.
Materials
and Methods:
We
retrospectively reviewed 37patients with distal tibia aseptic
nonunions treated in our orthopedic center over a 3-year period.
Nonunion has been defined by the United States Food and Drug
Administration as a fracture that occurred a minimum of nine
months previously and has not shown radiographic signs of
progression toward healing for three consecutive months6.
Diagnosis for nonunion was made based on clinical examination
that included local tenderness or false motion, and plain
radiographs in all patients. The infection nonunions and bone
defect more than 2cm were not included in this series. There
were 30 men and 7 women, with an average age of 43.02years
(range19-74years). All initial fractures were open. These were
classified according to Gustilo and Anderson as type
Ⅰ, type
Ⅱ, type
ⅢA, type
ⅢB and
typeⅢC .The
nonunion time was 9 to 27.5 months, with a mean time of 18.07
months. 4 patients had hypertrophic, and 33 patients had
atrophic nonunions according to the criteria of Weber and Cech7
. 15 nonunions were treated with Locking Compression
Plates and the others were treated with Unilateral External
Fixators. These two groups were eventually matched in terms of
age, nonunion time, nonunion types, open fracture types,
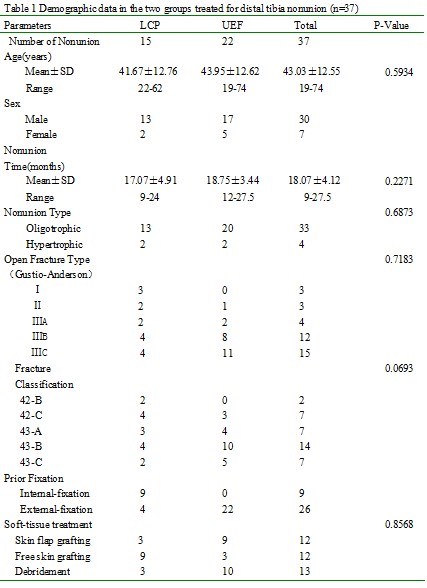
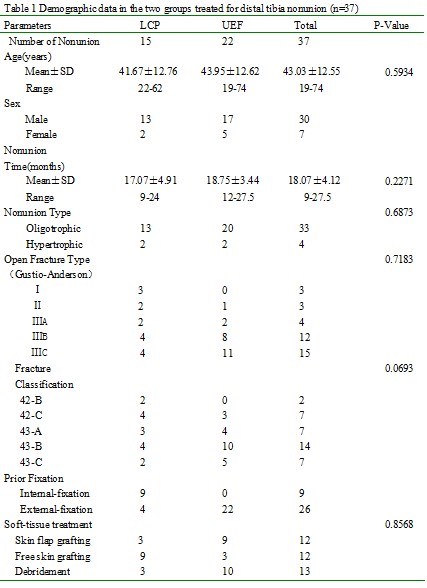
fracture classifications and soft-tissue treatments. (Details
in Table 1) .
External fixators were removed 2weeks before and internal
fixations were removed by small incision during the nonunion
operation in the LCP group. Iliac crest autogenous bone grafting
was performed in two groups during the fixation.
Postoperatively, patients were allowed to move the ankles with
no weight bearing. All patients remained non-weight bearing for
the first 4 to 6 weeks. Partial weight bearing in two groups
then started, provided that radiographs showed some evidence of
callus formation. Full weight bearing was allowed when adequate
bridging callus was visible on radiographs. Clinic and
radiographic examinations were scheduled regularly at 4 weeks,
and 3, 6, 9and 12 months after surgery till to bony union. Union
was defined as bridging callus crossing three of four cortices
on orthogonal radiographs with no pain on palpation over the
fracture site or when weight bearing. Time to bony union
、union
rates、complications
and sores of AOFAS were recorded.
Statistical analysis was performed by SAS V8.1 Software. The
normality test, T test or Wilcoxon Two-Sample test were used
where appropriate. A P value of less than 0.05(0.1 for
normality) was considered statistically significant. We made
statistical analysis of the two sample distributions in terms of
age、nonunion
types、nonunion
time、open
fracture types and fracture classifications. No statistical
significant differences were found in the constitution of the
two groups (p>0.05 Table1).
Results :
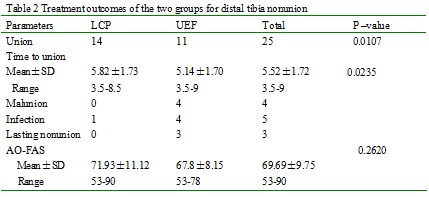
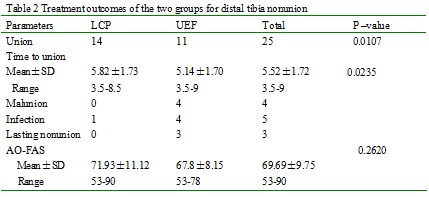
Average
time of follow-up was 10months (range 6-32 months).There were
significant differences in the treatment outcomes of union rates
、time
to union and complications including malunion、infection and lasting nonunion in
two groups. The LCP group had a higher union rate and lower
complications (p=0.0107<0.05) but a longer time to bony union(P=0.0235<0.05).
Though the mean scores of AOFAS in LCP group were better than
that in UEF group, there was no statistically significance
between the two groups (p =0.2620>0.05). (Table2)
Discussion :
Many
factors have been associated with nonunions. Most are related to
the initial injury. There is a direct correlation between the
nature of the injury and the likelihood of nonunions. The
prevalence of distal tibia nonunions increases with the severity
of open fractures. The endosteal and periosteal blood supply is
often extensively destroyed when the open fracture occurs in the
distal one-third of the tibia, which are regarded as the most
important to the healing of a tibia fracture8.
Nonunions are classified according to their radiographic
appearance as hypertrophic, oligotrophic, or atrophic as defined
by LaVelle6. Hypertrophic nonunions have abundant
callus. This indicates an adequate blood supply but a lack of
sufficient mechanical stability for completion of
fracture-healing. Oligotrophic nonunions have little callus but
still have an adequate blood supply. These nonunions are
typically due to inadequate reduction with little or no contact
between the fracture surfaces. Atrophic nonunions have no or
little callus and have resorption of the bone. Most distal tibia
nonunions after open fractures are inclined to be atrophic
nonunions due to deficient biologic processes with sever soft
tissue injuries.
Failure
to inadequately mobilize the fractures are also known to
increase the prevalence of nonunion and delay the time to union9.Successful
management of a nonunion often depends on appropriate reduction
and realignment of the fracture, bone grafting, and
stabilization. Three main methods of fixation are used for the
distal tibia nonunions: intra-medullary nailing, plate fixation
or external fixation. The literatures supporting the successful
using of each method have been published. External fixation was
considered for definitive fixation of type-II and type-III open
fractures or for patients with compromised soft tissue10.
Experimental and clinical studies have shown unilateral external
fixators some advantages, which provides free wound access and
allows stabilization of bone fragments at a distance from the
lesion. However, there is a significant risk of complications
from pin tract infection, pin loosening, malunion and lasting
nonunion. Locked intramedullary nailing also has been used in
this type of reconstruction. This may be technically difficult
when the intramedullary canal was closed in a atrophic nonunion.
It is also difficult to obtain adequate segment in the distal
fragment with the interlocking screws due to its small size and
osteopenia 11. Use of compression plates for the
treatment of closed tibia nonunions has been advocated by Muller
and Thomas12,13. Success rates with compression
plates alone have been reported to be high in the treatment of
hypertrophic nonunions, and supplementary bone-grafting was
suggested for atrophic nonunions.
Since
the introduction of the LCP in 2001, various papers have dealt
with clinical results obtained with this osteosynthesis system.
In Martyn Snow’s14 study, the LCP was more stable
than the DCP. Many researches have reported the successful
treatment of distal tibia fracture using LCP with MIPPO
technology. In 2004, Ring D15 reported the good
results of LCP for the treatment of the humerus osteoporotic
nonunons.
All
above support the possibility of using LCP for distal tibia
nonunions. We made a comparative study between LCP and UEF with
iliac crest autogenous bone grafting for distal tibia nonunions
and we found some statistical significance in terms of union
rates, time to union and complications between two groups. There
has been some controversy concerning the role of internal
fixation following previous external fixation. Because of the
risk of infection, we also do not recommend insertion of plates
regardless of the condition of the soft tissue. After removal of
external fixation with no infection and good soft tissue
covering, LCP can be performed with a low risk. The limitation
of this study is that this is a comparative study with
relatively small number of study groups. A large number of
samples and prospective randomized trials are required for
further confirming the advantages of LCP in the treatment of
distal tibia nonunion.
Conclusion:
We
recommend LCP with iliac crest autogenous bone grafting for the
high union rates and lower complications for distal tibia
nonunions in which there was no any infection.
Reference:
-
Velazco A, Whitesides TE Jr, Fleming LL. Open fractures of the
tibia treated with the Lottes nail. Journal of Bone and Joint
Surgery- American Volume. 1983;65:879-85.
-
Ruedi TP, Allgower M. The operative treatment of intra-articular
fractures of the lower end of the tibia. Clinical Orthopaedics
and Related Research. 1979;138:105–110.
-
Edwards CC, Simmons SC, Browner BD, Weigel MC. Severe open
tibia fractures: results treating 202 injuries with external
fixation. Clinical Orthopaedics and Related Research.
1988;230:98–115.
-
Gershuni DH, Halma G. The AO external skeletal fixator in the
treatment of severe tibial fractures. Journal of Orthopaedic
Trauma. 1983;23:986–990.
-
Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM,
Swiontkowski MF. Treatment of type II, IIIA and IIIB open
fractures of the tibial shaft: a prospective comparison of
unreamed interlocking intramedullary nails and half-pin
external fixators. Journal of Orthopaedic Trauma. 1998;12:1–7.
-
LaVelle DG. Delayed union and nonunion of fractures. In:
Canale TS editor. Campbell’s operative orthopaedics. 9th ed.
St. Louis: Mosby;1998:2579-629.
-
Weber BG, Cech O. Pseudoarthrosis: Pathology,
Biomechanics,Therapy, Results. Berne, Switzerland; Hans Huber
Medical Publisher,1976.
-
Macnab I. Blood supply of the tibia [abstract].In:
Proceedings and Reports of Councils and
Associations. Journal of Bone and Joint Surgery- British
Volume. 1957;39:799.
-
Connolly JF. Common avoidable problems in nonunions. Clinical
Orthopaedics and Related Research. 1985;194:226-35.
-
Green SA, Garland DE, Moore TJ, Barad SJ. External fixation
for the uninfected angulated nonunion of the tibia. Clinical
Orthopaedics and Related Research. 1984; 190:204-11.
-
Patzakis MJ, Wilkens J, Wiss DA. Infection
following intramedullary nailing of long bones: diagnosis and
management. Clinical Orthopaedics and Related Research.
1986;212: 182–191.
-
Muller ME. Treatment of nonunions by compression. Clinical
Orthopaedics and Related Research. 1965;43:83-92.
-
Muller ME, Thomas RJ. Treatment of non-union in fractures of
long bones. Clinical Orthopaedics and Related Research.
1979;138:141-53.
-
Martyn S, Graham T,Phillip GT. A
Mechanical Comparison of the Locking Compression Plate (LCP)
and the Low Contact-Dynamic Compression Plate (DCP) in an
Osteoporotic Bone Model. Journal of Orthopaedic Trauma.
2008;22:121-125.
-
Ring D, Kloen P, Kadzielski J, Helfet D, Jupiter JB. Locking
Compression Plates for Osteoporotic Nonunions of the
Diaphyseal Humerus. Clinical Orthopaedics and Related Research
2004:425:50–54.
|