|
Abstract:
Introduction:
With unstable thoraco-lumbar vertebral fractures primary
stabilization with internal fixator is the operative method of
first choice. With osteoporosis with older patients anchoring is
unsafe and vertebrae may lose height secondarily. We want to
analyze retrospectively the behavior of such unstable
osteoporotic fractures.
Material and Methods:
In 2007 and 2008 61 patients older than 60 years with an average
age of 73 ± 8 years (60-88 years) with unstable thoraco-lumbar
vertebral fractures were treated with a percutaneous internal
fixator. Preoperatively, postoperatively and after six weeks of
functional treatment without a brace the kyphosis angle was
determined in a lateral radiography and compared with
Student-t-Test. In 7 cases cement-augmented screws were used.
Results:
Kyphosis angle preoperative was 13,9 ± 9,4° and postoperative
8,1 ± 6,7°. Thus a reduction of height of 5,8 ± 5,9° (p < 0,001)
was achieved by the operation. Within the first six weeks
postoperative, however, loss of height of 7,7 ± 7,4° (p < 0,001)
occurred, caused by cutting out of screws through the vertebra,
as the screw-rod connections remained constant in all cases
without significant changes. With the operations with
cement-augmented screws there was no loss of height.
Unstable vertebral fractures with patients over 60 years cannot
be held by the fixator alone. Loss of reduction occurred from
the cutting-out of screws in osteoporotic bone. Therefore,
either in one or in two operations, stabilization of ventral
column must be performed, or in addition cement augmentation of
pedicle screws.
J.Orthopaedics 2010;7(4)e1
Keywords:
osteoporotic fractures; thoracolumbar spine; Sextant;
minimally-invasive
Introduction:
Vertebral fractures are frequent with older patients.
Osteoporosis plays an important part with the outset of these
fractures. By the 55th year a significant increase of
fracture-incidence can be observed (1), herewith a slight trauma
can be the cause for a painful fracture of vertebra, in some
cases spontaneous fractures occur without trauma. According to
the classification of Magerl (2) different procedures of
stabilization can be applied. Whereas compression fractures
Magerl A1 and A2 can safely be treated with kyphoplasty to
prevent an increasing kyphosis, to reduce vertebra and to
relieve pains (3), fractures involving the back column according
to Magerl A3, as well as unstable Magerl B- and C-fractures, are
an indication for dorsal instrumentation (2). To stabilize in an
emergency situation, open or minimally invasive percutaneous
systems may be applied. At the moment, there exist several
percutaneous systems for dorsal instrumentation (4,5). Minimal
invasive technique allows a correct and safe placement of
pedicle screws without disadvantage compared to the open method
(6). Great advantages of percutaneous application are short
incisions and lesser trauma to surrounding tissues. The result
is less blood loss and protection of back muscles (7,8).
Patients can be faster mobilized and hospital stay shortened
(9,10). By a shortened operation time, a risk reduction
especially with old patients succeeds (11). To avoid mechanical
complications and a cut-out with old patients, pedicle screws
may be augmented with cement (12).
We use the CD Horizon Sextant IITM
with cannulated polyaxial screws and the CD Horizon LongitudeTM with cannulated
non-polyaxial screws of Medtronic.
The aim of our study was to
find out if percutaneous procedures with patients over 60 years
are prone to reach a reduction and if sufficient stability
during the healing process is achieved. Further it was to be
examined whether polyaxial screw-rod connections have sufficient
stability.
Materials
and Methods:
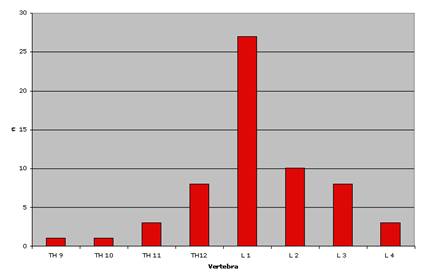
In 2007 and 2008 we operated altogether 61 (m:f = 23:38) (Tab.
1) patients over 60 years old with unstable monosegmental
fractures of thoraco-lumbar transition and lumbar spine (Fig. 1)
on a percutaneous internal fixator. After a fall besides
conventional X-ray analysis in all cases a CT or MRI was
required. 58 times there were Magerl A3- and in 3 cases
C1-fractures. 29 patients received the CD Horizon Sextant IITM
(Fig. 2) and 32 patients the CD Horizon LongitudeTM.
Median age was 73 ± 9 years (60-88 years) and did not differ
significantly within both groups (p = 0,25).Because of
considerable osteoporosis with radiologic rarification of
trabecles primarily cement-augmented screws were used in 7
cases. PMMA-cement was introduced in the vertebral body after a
kyphoplasty of screw site. Median age of patients with cemented
screws was 77 ± 7 years (71-88 years).
We examined the patients in a short follow-up interval of six
weeks postoperative and determined kyphosis angle as described
by Kuklo et al. (13) and compared with postoperative kyphosis
angle with Student-t-test. In addition, the screw-screw angle of
internal fixator was measured and compared by Student-t-test
with connected probes. Error probability was determined at 0,05.
After 6 weeks with 35 patients, stabilization of ventral column
was performed. In the Sextant group, the ventral column was
stabilized in 18 cases (14 x Kyphoplasty, 4 x Obelisk), in the
Longitude group 17 patients achieved stabilization of ventral
column (14 x Kyphoplasty, 1 autologous tricortical iliac crest
graft and MACS II, 2 x Obelisk). Pains were defined according to
Visual analogous scale pre- and postoperatively and
incision-suture time was evaluated. Intraoperative blood loss
was estimated. Data analysis was done retrospectively.
Fig. 1
Localization of fracture
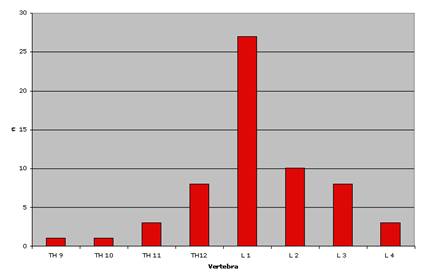
Fig.2
Radiographs of a case of a Th 12 fracture Magerl Classification
A3 preoperative (A), postoperative (CD Horizonâ
Sextant IIÔ
B) an
6 weeks postoperative (C) and after ventral stabilization with a
Obelisk (D)
  
A
B
C

D
Results :
The time
between incision and suture was 58
± 38
minutes in the Sextant group, 47
± 18
minutes in the Longitude group, and 52
± 29
minutes in both groups combined. No significant difference was
found between the two groups (p = 0.065). The hospitalization
duration was 10
± 5
days and the intraoperative blood loss 10-20 ml in both groups.
The
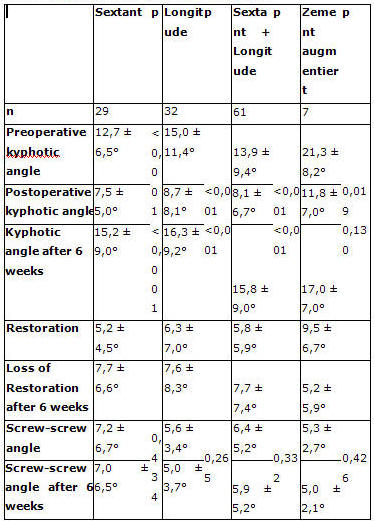
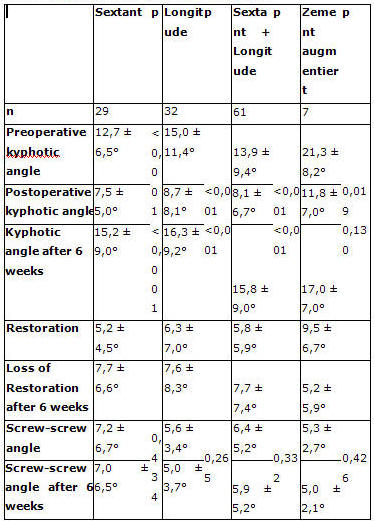
preoperative kyphotic angle (Table 2) was 12.7
± 6.5°
in the Sextant group, 15.0
± 11.4°
in the Longitude group, and 13.9
± 9.4°
in all 61 patients. No significant difference was observed
between the two groups (p = 0.17). In
the Sextant group a restoration of 5.2
±
4.5° was achieved, resulting in a kyphotic angle of 7.5
±
5.0° (p < 0.001).
In the Longitude group the kyphotic angle was reduced by 6.3
±
7.0° to 8.7
±
8.1°
postoperatively (p < 0.001), with no significant difference
between the two groups (p = 0.338).
Both groups
together yielded a restoration in the kyphotic angle from 5.8
± 5.9°
to 8.1
± 6.7°
postoperatively (p < 0.001).
At 6 weeks the
Sextant group showed a loss in reduction of 7.7
± 6.6°,
resulting in a kyphotic angle of 15.2
± 9.0 °
(p < 0.001). At the same time the Longitude group revealed a
loss of 7.6
± 8.3°,
resulting in a kyphotic angle of 16.3
± 9.2 °
(p < 0.001). No significant difference was observed between the
two groups (p = 0.353). The screw-rod-screw constructs remained
unchanged in all groups, without significant variances.
The VAS pain
scores were reduced significantly from a mean value of 6
preoperatively to 2 postoperatively (p < 0.001). In the group of
patients with cement-augmented screws (n = 7, males:females =
2:5), significant reduction was achieved (p < 0.001): the
preoperative kyphotic angle of 21.3
± 8.2°
was reduced by 9.5
± 6.7
to 11.8
± 7°
postoperatively. In this group no significant losses in the
restored height (p = 0.130) with secondary increase in the
kyphotic angle (p = 0,426) were observed (table 2).
No
neurological disorders occurred. In one case we removed a
postoperative hematoma, in another case a late infection led to
early removal of the internal fixation.
Three cases of
secondary screw cut-out were observed with migration of the
screw tip into the intervertebral disc, requiring revision of
the internal fixation including anterior stabilization. One
apoplexy occurred in a female patient during hospitalization,
independent of the surgical intervention. Hospital mortality
amounted to 0%.
Table 1
Clinical data of patients treated
|
|
Longitude |
Sextant |
Longitude and Sextant |
|
n |
32 |
29 |
61 |
|
Age |
73 ± 8 (60 - 88) |
72 ± 9 (60-88) |
73 ± 9 (60 - 88) |
|
Magerl Classification |
31x A3 , 1x C1 |
27x A3, 2x C1 |
58x A3, 3x C1 |
|
Ventral procedur |
14x kyphoplasty 1x MACS II,
2x Obelisk |
14x kyphoplasty, 4x Obelisk |
28x kyphoplasty, 1x MACS II,
6x Obelisk |
|
Complications |
1 Late infection and early removal
1 Revision of internal fixation |
1 Removal of postoperative hematoma |
1 Late infection and early removal
1 Revision of internal fixation
1 Removal of postoperativ hematoma |
|
Cement augmentation |
6 |
1 |
7 |
|
Hospitalization duration |
10 ± 4 Tage |
11 ± 6 Tage |
10 ± 5 Tage |
Table 2
Kyphotic angle and screw-screw angle
Discussion :
In order to prevent recurring kyphosis and neurological damage
unstable vertebral fractures are indication for dorsal
stabilization. Dorsal instrumentation with internal fixator here
is established first treatment. By this measure a quick and safe
mobilization of older patients and reduction of pains can be
achieved. We postponed an immediate stabilization of ventral
column to minimize preoperative mortality and morbidity and thus
diminish operation risk.
Alternatively with older patients a kyphoplasty can be used as a
minimally invasive procedure. In our patients base we not
initially do kyphoplasty. With all fractures damage of posterior
column existed, we therefore wanted to avoid dorsal and herewith
spinal cement leakage which could cause neurologic damage.
Mueller et al (14) showed in their study with 36 patients with
unstable burst fractures of thoraco-lumbar spine a decompression
of the spinal canal of approximately 10% by ligamentotaxis. An
additional decompression was not performed when neurologic
symptoms were not present. Operative technique was carried
through in ventral sag with non-polyaxial screws under
distraction.
With our data we could show that with a percutaneous fixator
even with limited distraction potential of systems alone by
ventral sag an expansion of the vertebra and therewith
reconstruction of alignment is possible. This reduction,
however, with patients over 60 years cannot be upheld alone by
the internal fixator. Within only 6 weeks, a secondary kyphosis
can occur. A longer post-examination interval was deliberately
not chosen, as a significant loss of reduction already after
this short time occurred and one could not rely on a spontaneous
reconstruction of the secondarily sintered vertebra.
As the screw-rod connection in our investigations remained
without change, secondary kyphosis must be caused by a cutting
out of screws through the vertebral body. McLain et al (15)
could prove a similar loss of reduction of about 10° comparable
to our data during healing phase of unstable thoraco-lumbar
fractures in their five year follow up with their short-range
instrumentation with 6 of 11 patients. An immediate ventral
stabilization also with long-range instrumentation led with all
patients in their study to a satisfactory clinical result, a
secondary kyphosis was prevented, a loosening of internal
fixator was not observed. Post-operative pain after ventral
stabilization also was significantly less.
In 2009 Palmisani et al (16) compared different percutaneous
fixator models with 51 patients with 64 fractures and were able
to find significant loss of reduction of 3,9° after 14 months
only with patients who had been treated with CD Horizon
LongitudeTM with polyaxial screws. Ventral procedures
were not applied. In this collective, patient age however was
with 45 years distinctly younger than with our patients.
Observation time was longer than in our examinations. Logroscino
et al (17) used a long dorsal instrumentation with multimorbid
old patients by inserting screws in 2 vertebra each above and
below the fractured vertebra. In 9 examined cases in a one year
follow-up no signs of loosening or fatigue of material were
noticed. Therefore they considered this construction as more
stable than monosegmental procedure with this patient
collective. Because of small case numbers, however, further
investigation with a bigger collective is demanded.
Ataka et al (18) were able to prove a loss of reduction of 4,1°
in their investigations in a 25 months follow-up on 14 patients
with a median age of 73 years. With unstable osteoporotic
fractures, they used an internal fixator with open approach.
Loss of reduction was less marked than in our study, but patient
number in their study was small, thus no valid statement can be
pronounced.
Numerous studies as to resistance of pedicle screws in
osteoporotic bone have already been published. Thus Soshi et al
(19) already in 1991 were able to prove a significant decreased
resistance of screws in osteoporotic bone in a cadaver study.
Mean age of participants with 71 years was comparable to our
collective. In the study, they could prove - depending on the
degree of osteoporosis - a 50-70% diminished strength of screws
in bone. Additionally, they showed that cement augmentation led
to a significant improvement of screw firmness with little and
median osteoporosis (Jikei Grade I-II), with a severe
osteoporosis (Jikei Grade III) no significant improvement of
strength could be verified. Yet in the study, there was always
chosen the pull-out strength along long axis of screw. Cutting
out of screws with fixator in place however means a pull and
shear movement within the vertebra. Hence, these results cannot
be completely compared to our results. Biological aspects like
bone growth in screw-threads, sclerosis of bone etc. are not
taken into consideration in a cadaver study. We could only prove
with a very small collective of 7 patients that by cement
augmentation of pedicle screws an improved stability in bone of
the fixator can be achieved. For valid evidence, though, bigger
case numbers are needed.
The different techniques of cement augmentation were examined by
Becker et al in 2008 (12) in an experimental cadaver study. Mean
patient age was 79,8 years (72-89 years) and was therewith
comparable to our collective. In the study the augmentation
techniques of vertebroplasty, kyphoplasty and augmentation by
cannulated screws were compared. Like us they used a PMMA-bone
cement. They could prove a significant nearly double as high
firmness in osteoporotic bone by cement augmentation with
cannulated screws and with vertebroplasty-augmented screws. But
they didn’t find superior firmness of screws with
kyphoplasty-augmented screws. In our cases we did not either use
kyphoplasty for cement augmentation, therefore we were also able
with our small case number to prove a significantly increased
strength of screws. After first bad experiences we abandoned
cementing via perforated screws, as a percutaneous application
was difficult, only possible with expensive additional modules
of single-use. Frequently there were problems with cement
extrusion in the thread of rod connections.
Halvorson et al (20) could also show in a cadaver study that
there is a linear correlation between pull-out strength and bone
density with pedicle screws. They didn’t mention patients’ age.
In addition they found that predrilling of holes of pedicle
screws caused a significant worsening of screw-anchoring in
osteoporotic vertebra. In this study, pull-out strength was also
chosen along screw long-axis. For this reason, these results are
not completely comparable to our results, but they show a
possible factor which might have caused instability of
construction. In our case screw-holes were predrilled with a
tap, lately corticalis is only cut with 2-3 screw threads.
Thereby we hope to achieve increased density of spongiosa around
the screws.
In our retrospective study, measuring of the bone density was
not possible for no valid statement concerning bone density from
MRI-pictures can be made. A quantification of bone quality could
therefore not be done in our study. Following demographic
investigations, we had to suppose a diminished bone quality by
osteoporosis in our patient collective.
To sum up, this means that treatment of unstable vertebral
fractures with osteoporotic bone quality with percutaneous
fixator systems Sextant IITM and LongitudeTM
allows a reconstruction of fractured vertebra, that this
reduction cannot be upheld by the fixator alone. This is caused
by cutting-out of screws through the vertebral body. Cement
augmentation of pedicle screws and an early stabilization of
ventral column may be corrective measures.
Reference:
-
Singer BR, McLauchlan GJ, Robinson CM, Christie J (1998)
Epidemiology of fractures in 15000 adults: The influence of
age and gender. J Bone Joint Surg Br 80:243-248
-
Magerl F, Aebi M, Gertzbein D, Harms J, Nazarian S (1994) A
comprehensive classification of thoracic and lumbar injuries.
Eur Spine J 3:184-201
-
Wardlaw D, Cummings SR, Meirhaeghe JV, Bastian L, Tillman JB,
Ranstam J, Eastell R, Shabe P, Talmadge K, Boonen S (2009)
Efficacy and safety of balloon kyphoplasty compared with
non-surgical care for vertebral compression fracture (FREE): A
randomised controlled trial. Lancet 373:1016-1024
-
Mathews HH, Long BH (1995) Endoscopy assisted percutaneous
anterior interbody fusion with subcutaneous, suprafaszial
internal fixation: Evolution of technique and surgical
considerations. Orthopedics 3:353-366
-
Lowery GL, Kulkarni SS (2000) Posterior percutaneous spine
instrumentation. Eur Spine J 9:126-130
-
Ringel F, Stoffel M, Stüer C, Totzek S, Meyer B (2006)
Minimally invasive transmucular pedicle screw fixation of the
thoracic and lumbar spine.
Neurosurgery 59:ONS361-367
-
Grass R, Biewener A, Dickopf A (2006) Perkutane dorsale versus
offene Instrumentation bei Frakturen des thorakolumbalen
Übergangs- Eine vergleichende prospektive Untersuchung.
Unfallchirurg 109:297-305
-
Rampersaud YR, Annand N, Dekutoski MB (2006) Use of minimally
invasive surgical technique in the management of thoracolumbar
trauma. Spine 31 (Suppl 11):S96-102
-
Dickermann RD, Reynolds AS, Tackett J, Winters K, Alvarado C
(2008) Percutaneous pedicle screws significantly decrease
muscle damage and operative time: surgical technique makes a
difference! Eur Spine J 17:1398
-
Park Y, Ha JW (2007) Comparison of One-Level Posterior Lumbar
Interbody Fusion Performed With a Minimally Invasive Approach
or a Traditional Open Approach.
Spine 32:537-543
-
Schmidt OI, Strasser S, Kaufmann V, Strasser E, Gahr RH (2007)
Role of early minimal-invasive Spine fixation in acute
thoracic and lumbar spine trauma.
IJO 41:374-380
-
Becker S, Chavanne A, Spitaler R, Kropik K, Aigner N, Ogon M,
Redl H (2008) Assessment of different screw augmentation
techniques and screw designs in osteoporotic spines. Eur Spine
J 17:1462-1469
-
Kuklo TR, Polly DW Jr, Owens BD, Zeidman SM, Chang AS, Klemme
WR (2001) Measurement of the thoracic and lumbar fracture
kyphosis. Spine 26(1):62-66
-
Mueller LA, Mueller LP, Schmidt R, Forst R, Rudig L (2006) The
phenomenon and efficiency of ligamentotaxis after dorsal
stabilization of thorakolumbar burst fractures. Arch Orthop
Trauma Surg 126:364-368
-
McLain RF, Burkus JK, Benson DR (2001) Segmental
instrumentation for thoracic and thoracolumbar fractures:
prospective analysis of construct survival anf five-year
follow-up. Spine J 1:310-323
-
Palmesani M, Gasbarrini A, Barbanti Brodano G, De Iure F,
Cappuccio M, Boriani L, Amendola L, Boriani S (2009) Minimally
invasive percutaneous fixation in the treatment of thoracic
and lumbar spine fractures. Eur Spine J 18 (Suppl 1):S71-74
-
Logroscino CA, Proietti L, Tamburrelli FC (2009) Minimally
invasive spine stabilisation with long implants. Eur Spine J
18 (Suppl 1):S75-81
-
Ataka H, Tanno T, Yamazaki M (2009) Posterior instrumented
fusion without neuronal decompression for incomplete
neurological deficits following vertebral collapse in the
osteoporotic thoracolumbar spine. Eur Spine J 18:69-76
-
Soshi S, Shiba R, Kondo H, Murota K (1991) An Experimental
Study on a Transpedicular Screw Fixation in Relation to
Osteoporosis of the Lumbar Spine. Spine 16:1335-1341
-
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS; Cook SD
(1994) Effects of Bone Mineral Density on Pedicle Screw
Fixation.
Spine 19:2415-2420
|