|
Abstract:
Percutaneous vertebroplasty in the treatment of symptomatic
vertebral compression fractures has become a popular treatment
modality. The main purpose of the procedure is pain relief.
Recent studies however, have cast doubt on its efficacy. An
additional benefit of the procedure is possibly a partial
restoration of the height of the collapsed vertebral body with
potential improvement in the sagittal alignment and biomechanics
of the spine.
Digital
radiographs of 70 thoracolumbar osteoporotic compression
fractures in 57 patients were reviewed retrospectively before
and after vertebroplasty for changes in the vertebral height,
wedge angle, kyphosis angle, thoracolumbar and lumbar sagittal
angles.
Increases
in anterior and middle heights post-vertebroplasty were
statistically significant, along with improvements in the wedge
angle and thoracolumbar sagittal alignment.
This study
shows that percutaneous vertebroplasty effectively increases
vertebral body heights resulting in improvements in the wedge
angles. These improvements are achieved solely by placing
patient in the prone position during the procedure. In addition,
there was improvement in the thoracolumbar sagittal alignment.
This finding is previously unreported and although the
significance of this improvement is unclear, it may potentially
result in improved biomechanics of the spine which may in turn
result in reduced risk of adjacent level vertebral fractures.
J.Orthopaedics 2010;7(3)e7
Keywords:
Vertebroplasty; vertebral body height; osteoporotic compression
fractures; sagittal alignment
Introduction:
The
prevalence of osteoporosis worldwide is increasing due to a
combination of improved healthcare and advances in medical
science resulting in increased life expectancy1.
Among the many complications of osteoporosis, vertebral
compression fractures (VCF) have also become more common. There
is often a tendency to overlook the morbidities associated with
osteoporotic VCF due to the traditionally “conservative”
management of such conditions. Many VCF are asymptomatic and are
only diagnosed incidentally but those that are symptomatic are
often associated with significant morbidity. In addition, loss
of anterior height results in wedge deformity of the affected
level which is postulated to result in abnormal spinal
biomechanics through altered sagittal alignment.
Percutaneous vertebroplasty was described by Gilbert2
in 1987 in the treatment of aggressive hemangiomas of the
vertebral body. Subsequently, this technique was extended for
use in the management of painful VCF. As such, the main
indication of vertebroplasty in the treatment of VCF is that of
intractable pain despite a trial of conservative management via
analgesia, bed rest, gentle physiotherapy and other adjuncts
e.g. acupuncture.
Percutaneous vertebroplasty involves the injection of
polymethylmethacrylate (PMMA) into the affected vertebral body,
often under local anaesthesia or under sedation. Partial to
total relief of pain in 80 – 90% of patients is reported over
the next 72 hours3,4. These results, though
impressive, do not address the problem of loss of height
resulting from the compression fracture. Loss of height and
wedging of the affected vertebral body results in altered
biomechanics of the spine and have been associated with
increased risk of developing adjacent level compression
fractures5. Kyphoplasty was hence developed in the
hope of achieving the same excellent results as vertebroplasty
with the added advantage of restoring the loss of vertebral body
height6. The major drawback of this technique
however, is its significantly greater cost as compared to that
of vertebroplasty.
Several
authors have observed mobility in vertebral compression
fractures and have reported increases in vertebral height
following vertebroplasty using postural reduction7-9.
This study
was undertaken to investigate the immediate radiological effects
of vertebroplasty with respect to the improvement in vertebral
height, angles and sagittal alignment following percutaneous
vertebroplasty.
Materials
and Methods:
Vertebroplasty for 70 osteoporotic compression fractures in 57
consecutive patients (47 females and 10 males) were carried out
between the periods of Jan 2005 to Dec 2006. Age of patients
ranged from 57 to 96 years with an average of 78 years. The main
indication for the procedure was pain not improved despite
conservative treatment, together with radiographic evidence of
either an acute compression fracture or pseudoarthrosis.
Duration of symptoms (ranging from 1 week to 10 months) was not
considered an important consideration in the decision for or
against surgery.
All
patients underwent magnetic resonance imaging (MRI) of the spine
prior to vertebroplasty to ensure accurate identification of the
involved level especially in cases where more than a single
level of osteoporotic compression fracture existed.
Vertebroplasty was performed on acute fractures only, as
evidenced by MRI changes of increased signal intensity of the
vertebral body on T2 and short tau inversion recovery (STIR)
sequences.
All
pre-operative radiographs were taken in the erect position and
were performed within 2 weeks of vertebroplasty while all
post-operative radiographs were also taken in the erect position
and done within 3 days of the procedure. Only osteoporotic
compression fractures occurring in the thoracolumbar region of
T10 to L3 were included in this study. Any compression fractures
occurring as a result of other pathological conditions besides
osteoporosis (e.g. tumors) were excluded. Compression fractures
occurring as a result of blood dyscrasias were also excluded
based on routine screening blood investigations which include a
complete blood count, erythrocyte sedimentation rate and
C-reactive protein.
Digital
radiographs for these cases were reviewed by 2 independent
investigators pre and post vertebroplasty. All radiographs and
measurements were made using the Centricity (version 2.1, 2004
GE Medical Systems) digital radiography software.
Vertebroplasty technique
All cases
were done under local anaesthesia with sedation provided by an
anaesthetist. The patient was positioned in the prone position
on a radiolucent table (Jackson table, Orthopaedics Systems,
Inc) with pillows positioned under the patient to ensure comfort
during the procedure.
Under
guidance using an image intensifier, two 11 Gauge Spineplex
needles (Stryker Corp., Kalamazoo, Michigan) were inserted via a
bilateral transpedicular approach and advanced till the tip was
approximately between the anterior and middle thirds of the
vertebral body. Up to 10mls of radio-opaque contrast was
injected and any signs of leakage checked with the image
intensifier. If any leak was detected, the needle was
repositioned and again checked for the presence of leakage. In
the absence of leakage of contrast, PMMA loaded in 1ml syringes
was injected into alternate needles while filling was checked
regularly under image intensification. Between 2 to 7 mls of
PMMA was used in each vertebral body depending on the degree of
collapse, amount of filling and size of vertebral body.
Injection of PMMA was stopped when either filling was observed
to reach the posterior fourth of the vertebral body or if
significant leakage was observed. The patients were kept in the
prone position for 20 minutes since commencement of mixing of
cement, after which they were allowed to turn supine. The
patients were instructed to rest in bed on the day of the
procedure and allowed to ambulate on the first post operative
day. The patients were allowed to return home on the first
post-operative day.
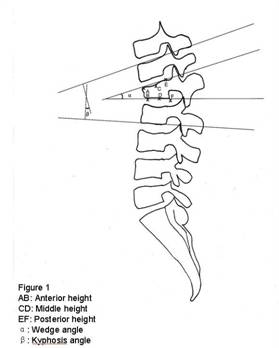
Measurement (Figure 1)
The lateral
radiographs of all patients were analyzed using the Centricity
(version 2.1, 2004 GE Medical Systems) digital radiography
software. The anterior, central and posterior heights were
measured using a magnified image to the nearest 0.1mm. The Cobb
angles, wedge angles, and sagittal alignment of the
thoracolumbar and lumbar regions (defined by convention as T10
to L2 and L1 to S1 respectively) were also measured to the
nearest 0.1 degrees.
Figure
1: This shows the method of measurement carried out for
determination of the wedge α and Cobb β angles on the lateral
radiograph. The measurement of anterior height is taken from
points AB, middle height from points CD and posterior height
from points EF.
Analysis
Analysis
of the data was carried out using the paired Students t-test
with the help of a statistician. Statistical significance was
taken as p value of less than 0.05.
Results :
Of the
patients analyzed, 48 had single level VCF, 6 had double level
VCF, 2 had triple level VCF and only one had 4 level VCF.
The most
commonly affected level is the T12 vertebrae with 23 cases.
Twenty cases involved the L1 vertebrae, 11 cases involved the L3
vertebrae, 9 cases involved the L2 vertebrae, 4 cases involved
the T11 vertebrae and only 3 cases involved the T10 vertebrae.
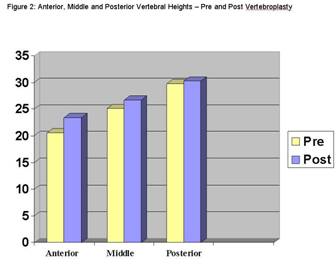
There were
statistically significant increases in anterior (p<0.001) and
middle heights (p<0.001). Of the 70 vertebral bodies which
underwent vertebroplasty, 48 had increases in anterior heights
and 43 had increases in middle heights. The average increase in
anterior height was 2.9mm (range -5mm to +16.7mm, SD of 4.8mm)
while the average increase in middle height was 1.6mm (range
-1.9mm to +14.5mm, SD of 3.6mm). (Figure 2).
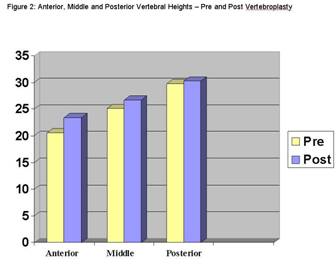
Figure 2:This
shows the pre treatment and post treatment vertebral heights
clearly demonstrating increases in post treatment vertebral
heights most markedly in the anterior and middle columns.
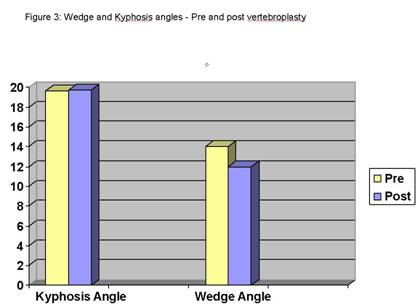
Statistically significant improvements in the wedge angles and
thoracolumbar saggital alignment were also measured. Wedge
angles improved by an average of 4.0° (range 0.2 to 10.4°, SD of
6.4°) while thoracolumbar saggital alignment improved by an
average of 2° (range of 0.2 to 9°, SD of 6.5°). (Figure 3) Of
the 70 vertebral bodies which underwent vertebroplasty, 43
showed improvement in wedge angles while 41 showed improvement
in sagittal angles.
The
kyphosis angle increased by 0.4° (range -16.5° to +18.6°,
SD of 6.3°) but this was not statistically significant
(P<0.881).
Posterior
heights generally increased but improvements were not
statistically significant. The average increase in posterior
height was 0.5mm (p=0.16). The change in lumbar sagittal
alignment showed a trend towards improvement by an average of
2.3°, but this was not statistically significant (p=0.74).
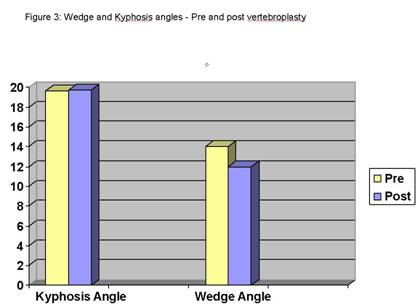
Figure 3:
This shows the pre treatment and post treatment vertebral wedge
and kyphosis angles demonstrating a statistically
non-significant increase in kyphosis angle, but a significant
improvement in the wedge angle.
Discussion :
Percutaneous vertebroplasty is a well described procedure that
has gained widespread acceptance. Its main application is for
safe, rapid and effective relief of debilitating pain associated
with acute wedge compression fractures of the vertebral body10,11.
More recent studies have studied the effects of vertebroplasty
on vertebral heights and many have found statistically
significant increases in vertebral heights post vertebroplasty7,12,13.
These improvements in vertebral heights were achieved using
postural reduction with the patient placed in prone position
during the procedure.
The
efficacy of vertebroplasty, however, has recently been disputed
by 2 randomized trials performed by independent investigators14,15.
Their findings that vertebroplasty yielded no better results
than sham procedures have cast doubt on the credence of the
procedure.
Our study
showed statistically significant improvements in the anterior
and middle vertebral heights. In addition, statistically
significant improvements in the wedge angles and thoracolumbar
sagittal alignment were also noted. These improvements were
likely due to performance of the procedure in the prone position
with pillows placed under the chest and hips to effect a gentle
hyper-extension of the spine. As the fracture was still
relatively recent, the prone position resulted in a partial
restoration of the vertebral height. Patients were also kept in
the hyper-extended position till the polymethyl-methacrylate
cement (PMMA) fully hardened after the procedure. In addition,
ambulation was delayed till the first post-operative day to
reduce the chances of loss of height immediately post procedure.
The rationale for this is based on the fact that the strength of
polymethylmethacrylate continues to increase for up to 4 to 5
days, after which its strength reaches a plateau16.
Keeping the patient in bed for that amount of time, however,
would be impractical and counter productive as patients could
encounter problems associated with protracted bed rest.
The results
of our study compare favorably with other studies done by other
investigators which also conclusively showed significant
increases in vertebral height post vertebroplasty7-9.
Teng et al7 showed significant increases in anterior,
middle, posterior heights (increment of 16.7%, 14% and 7%
respectively) in addition to kyphosis and wedge angles
(restorations of 4.3° and 7.4° respectively) of treated
vertebral bodies. Hitawashi et al8 also showed
significant increases in anterior, middle and posterior heights
(2.5mm, 2.7mm and 1.4mm respectively). However, the study
population in Hitawashi’s paper included compression fractures
that resulted from neoplastic diseases and osteoporosis. Chin et
al9 studied the efficacy of postural reduction prior
to vertebroplasty in 3 groups of patients categorized into
duration of onset of symptoms prior to intervention (less than 4
weeks, 4-8 weeks and more than 8 weeks). He presented his data
in the form of a compression ratio of the anterior height
divided by the posterior height. In all 3 groups, statistically
significant increases in compression ratio post vertebroplasty
were noted but more interestingly, the greater increases in
compression ratio were observed in more acute compression
fractures. The same observation was noted for the wedge and
kyphosis angles.
Our study
also analyzed the sagittal alignment of the spine pre and post
vertebroplasty. These are predefined by convention as L1 to S1
for the lumbar sagittal alignment and T10 to L2 for the
thoracolumbar alignment. Our study showed that the thoracolumbar
alignment showed significant improvement while lumbar alignment
did not. The reason for this observation is unclear. Our
postulation is that the lumbar motion segments are capable of
greater movements, and as such may “dampen” changes in wedge
angles of the treated vertebral segments. On the other hand,
thoracolumbar segments being less mobile, are not able to
compensate for any changes in wedge angles of the treated
vertebral bodies so readily.
Pradhan et
al17 analyzed the sagittal angle of spinal segments
pre and post kyphoplasty and found that improvement of the
angular deformity diminished as he measured the Cobb angle off
increasing numbers of spanning vertebrae from the VCF. He also
found that the length of spine over which sagittal alignment was
improved also increased with number of treated levels. In our
study, 7 patients had vertebroplasty done concurrently on 2
levels while only one had vertebroplasty done on 3 levels. A
sub-analysis done on these patients revealed a trend towards
improvement in the sagittal alignment of both the thoracolumbar
and the lumbar alignments. However due to the small sample size,
further studies using larger sample sizes are required to verify
these findings.
To the best
of our knowledge, no other studies have analyzed the effects of
vertebroplasty on the overall sagittal alignment of the spine.
In a biomechanical study, Kayanja et al18 showed that
the anterior wall of the upper adjacent vertebra of a VCF
experienced higher strain. This suggests that the resultant
kyphotic deformity from a VCF could predispose the adjacent
vertebral bodies to compression fractures. As such, our findings
are especially important as the improvement in wedge angles and
sagittal alignment could theoretically result in improved
biomechanics of the spine, hence reducing the incidence of
adjacent level VCF. If this is true, vertebroplasty should then
be adopted as the standard of treatment of VCF in all patients
deemed suitable to undergo the procedure. Further studies are
needed to confirm this postulation.
Conclusions:
Vertebroplasty has long been established as a safe and
efficacious means of pain relief from osteoporotic compression
fractures. 2 recent studies have cast serious doubt on the
efficacy of the procedure yielding results no better than sham
procedures, in terms of pain relief. The potential benefits of
vertebroplasty, however go beyond just pain relief. Significant
improvements in anterior and middle heights, wedge and kyphosis
angles are also observed. These improvements occur simply by
placing the patient in a prone position with pillows positioned
under the chest and hips. This maneuver not only enhances the
comfort of the patient but also causes hyper-extension and
hence, reduction of the fractured vertebra.
In addition
to improvements in the wedge angle of each treated vertebra,
some improvement of the sagittal alignment was also observed in
the thoracolumbar region. This improvement in the thoracolumbar
sagittal alignment may theoretically reduce the incidence of new
compression fractures occurring in the same patient. Further
studies are required to establish if this is indeed true.
Reference:
-
E M C
Lau.
Osteoporosis: Implications in Asia.
Ann Acad
Med Singapore
January 2002, Vol. 31 No.1
-
Galibert
P, Deramond H. Note préliminaire sur le traitement des
angiomes vertébraux par vertébroplastie acrylique percutanée.
Neurochirurgie 1987; 33: 166–7.
-
Deramond
H, Depriester C, Galibert P, Le Gars D: Percutaneous
vertebroplasty with polymethylmethacrylate: Technique,
indications and results. Raiol Clin North Am 36:533-546, 1998
-
Amar AP,
Larsen DW, Esnaashari N, Albuquerque FC, Lavine SD, Teitelbaum
GP: Percutaneous transpedicular polymethylmethacrylate
vertebroplasty for the treatment of spinal compression
fractures. Neurosurgery 49:1105-1114, 2001
-
Heaney
RP. The natural history of vertebral osteoporosis: Is low bone
mass an epiphenomenon? Bone 1992; 13 (suppl 2): 23–6.
-
Lieberman
IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and
efficacy of "kyphoplasty" in the treatment of painful
osteoporotic vertebral compression fractures. Spine. 2001 Jul
15;26(14):1631-8
-
Teng MMH,
Wei CJ, Wei LC, Luo CB, Lirng JF, Chang FC, Liu CL, Chang CY.
Kyphosis
Correction and Height Restoration Effects of Percutaneous
Vertebroplasty. AJNR Am J Neuroradiol 24:1893–1900,
October 2003
-
Hiwatashi
A, Moritani T, Numaguchi Y, Westesson PL. Increase in
vertebral body. AJNR Am J Neuroradiol. 2003 Feb;24(2):185-9.
-
Chin DK,
Kim YS, Cho YE, Shin JJ. Efficacy of postural reduction in
osteoporotic vertebral compression fractures followed by
percutaneous vertebroplasty. Neurosurgery. 2006
Apr;58(4):695-700; discussion 695-700.
-
Amar AP,
Larsen DW, Esnaashari N, Albuquerque FC, Lavine SD, Teitelbaum
GP: Percutaneous transpedicular polymethylmethacrylate
vertebroplasty for the treatment of spinal compression
fractures. Neurosurgery 49:1105–1114, 2001.
-
Jensen
ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE:
Percutaneous polymethylmethacrylate vertebroplasty in the
treatment of osteoplastic vertebral body compression
fractures: Technical aspects. AJNR Am J Neuroradiol
18:1897–1904, 1997.
-
Hiwatashi,
A, Moritani, T, et. al., Increase in vertebral body height
after vertebroplasty, AJNR Am J Neuroradiol 23:185-189,
February 2003
-
Hiwatashi
A, Sidhu R, Lee RK, deGuzman RR, Piekut DT, Westesson PL.
Kyphoplasty versus vertebroplasty to increase vertebral body
height: a cadaveric study. Radiology. 2005 Dec;237(3):1115-9.
-
Buchbinder, Rachelle, et al. "A Randomized Trial of
Vertebroplasty for Painful Osteoporotic Vertebral Fractures."
The New England Journal of Medicine.August 6, 2009, Volume
361:557-568, Number 6
-
Kallmes,
David F., et al. "A Randomized Trial of Vertebroplasty for
Osteoporotic Spinal Fractures." The New England Journal of
Medicine.August 6, 2009, Volume 361:569-579, Number 6
-
SS Haas,
GM Brauer and G Dickson. A characterization of
polymethylmethacrylate bone cement. J Bone Joint Surg Am.
1975;57:380-391.
-
Pradhan
BB, Bae HW, Kropf MA, Patel VV, Delamarter RB. Kyphoplasty
reduction of osteoporotic vertebral compression fractures:
Correction of local kyphosis versus overall sagittal
alignment. Spine. 2006;31:435-41.
-
Kayanja MM, Ferrara LA, Lieberman IH (2004) Distribution of
anterior cortical shear strain after a thoracic wedge
compression fracture. Spine J 4(1):76–87
|