|
Abstract:
Introduction:
unicompartmental knee replacement (UKR) is a popular alternative
to total knee replacement (TKR) in medial compartment disease.
Revision to TKR is well described as a late endpoint.
Our objective is to investigate early surgical management
of persistent pain following UKR, identify common themes and
effectiveness of re-interventions.
Methods:
381 UKRs implanted over 5 years included, and patients requiring
re-operation reviewed retrospectively.
Findings:
27 re-interventions performed on 17 patients at a mean 16.8
months (95% CI 9.5 to 24.1), with symptom onset post-operatively
at 9 months (95% CI 4-14). There were 10 arthroscopies, 10
revisions to TKR, 4 manipulations under anaesthesia (MUA), 2
bearing exchanges, and 1 tibial-plateau fracture fixation. MUA
improved stiffness 2 of 3 patients. Arthroscopy was successful
in 2 patients with loose cement-bodies, not providing a
diagnosis in 8, of whom 7 required subsequent revision. Overall
there were 10 revisions: 9 were performed for persistent pain
and 9 reported symptom improvement. Intra-operative findings
included aseptic loosening (n=4), synovitis (n=2), increased
posterior slope of the tibial cut (n=1), dislocated bearing
(n=1), and no cause of failure (n=2). There were no deep
infections.
Conclusions:
Our unit’s early re-intervention rate is 4.5% (95% CI 2.4 to
6.5), with a revision rate of 2.6% (95% CI 1.0 to 4.2) after a
mean (±SD) follow-up of 40 (±16) months. Arthroscopy is a poor
diagnostic and therapeutic option against persistent pain
following UKR. In contrast, the decision to revise, although
initially disappointing for both patient and surgeon, gave
symptom improvement in 90%.
J.Orthopaedics 2010;7(3)e5
Keywords:
Introduction:
The mobile bearing unicondylar knee replacement (UKR) was
developed in 1978, with the first Oxford partial knee
arthroplasty performed in 1982.1 Survival at ten
years is quoted at 98% (95% CI 93% to 100%) by the design group2
and 95% (95% CI 90.8% to 99.3%) quoted by an independent study.3
These excellent long term results have encouraged an increased
use of this implant for unicompartmental arthritis of the knee
in recent years.4
The Oxford group suggest one in three of all knees requiring
arthroplasty are suitable for a UKR,5 despite this
only approximately 8% of all knee arthroplasties are
unicompartmental replacements.4 This may be because
there is concern following UKR of persistent or new onset
post-operative pain. The pain could indicate an incorrect
initial choice of implant, disease progression to unresurfaced
compartments, aseptic loosening or infection.4
Further management of this group of patients presents a clinical
dilemma, especially if laboratory and radiological
investigations do not highlight a potential cause for their
symptoms. Conservative measures are usually recommended to
patients, with advice that the symptoms are likely to settle
with time or that the symptoms are not amenable to surgical
intervention. This reflects the established management of
similar pain following total knee replacement (TKR).6
Despite these reassurances there are a small number of
patients who consider their symptoms debilitating enough to
warrant further surgery.
The Royal Orthopaedic Hospital (Birmingham) is a specialised
Orthopaedic tertiary referral centre in the United Kingdom
dealing with a large throughput of arthroplasty patients, and
having on-site dedicated knee arthroplasty surgeons as well as
orthopaedic nurses and physiotherapists. The objectives of this
study are to establish early re-operation rates following UKR
and assess the results of subsequent operative intervention in
patients with debilitation pain following primary UKR.
Materials
and Methods:
All Phase 3 Oxford UKRs (Biomet, Bridgend, UK) implanted at our
institution between November 2002 and December 2007 were
included in the study. 40 patients underwent bilateral surgery.
Surgery was performed under the supervision of seven consultant
arthroplasty surgeons as described in the manual of surgical
technique.7 Patients who required any subsequent
surgery on the ipsilateral knee were highlighted retrospectively
using our proprietary database, and their medical notes
individually reviewed.
Results :
383 UKRs were performed on 343 patients over this five year
period, with a mean (±SD) follow-up of 40.1 months (±16 months).
Two patients were excluded as they underwent simultaneous ACL
reconstruction leaving a cohort of 381 UKRs.
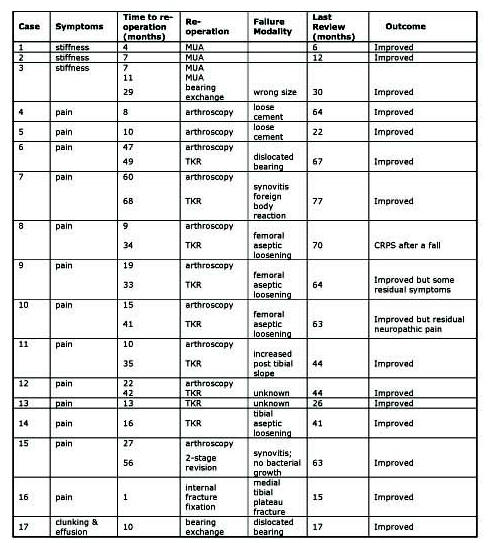
There were 27 re-operations performed in 17 patients [see table
1], equivalent to a re-intervention rate of 4.5% (95% CI 2.4 to
6.5). The mean time to the first re-operation was 16.8
months (95% CI 9.5 to 24.1) from the primary procedure.
Procedures undertaken were: 10 revisions to total knee
replacements (1 performed in two stages), 10 arthroscopies, 4
manipulations under anaesthetic (MUA), 2 exchange of mobile
bearings and 1 open reduction internal fixation of a tibial
plateau fracture.
Manipulation under anaesthetic
Three patients with ongoing limited range of movement were
manipulated. Satisfactory range of movement was achieved for
two patients. Despite two manipulations the final patient did
not improve until the mobile bearing was exchanged for a smaller
component. This resulted in a satisfactory outcome.
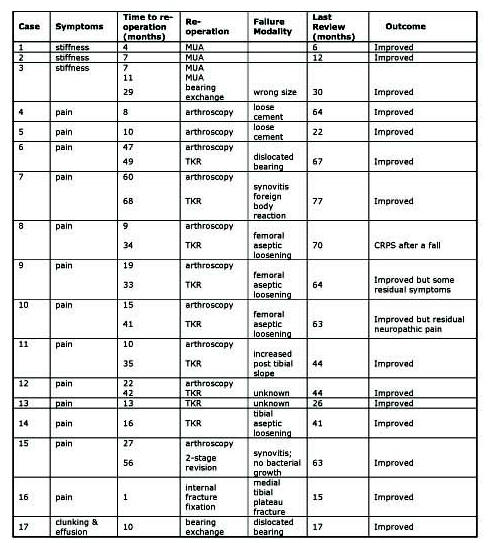
Table 1:
Summary of patients requiring re-intervention
Arthroscopies
Ten patients were managed with arthroscopic procedures, but only
two (20%) had significant resolution of their symptoms. In both
these cases loose cement fragments were seen in post-operative
radiographs and arthroscopic removal settled their symptoms.
Arthroscopic assessment of the remaining eight patients revealed
no gross loosening of the implants when probed and no gross
disease progression. One patient was noted to have lateral
partial thickness fissuring in the lateral compartment, while
four patients had evidence of early patello-femoral wear. All
eight were subsequently revised to total knee replacements, with
symptom improvement in seven. Mean interval between arthroscopy
and revision was 17.1 months (95% CI 10.1 to 24.1).
Revision
to total knee replacement
In total ten UKRs were revised to total knee replacements, eight
as previously discussed were following initial arthroscopic
surgery, and two following radiographic suspicion of aseptic
loosening. Mean time from primary UKR to revision was
38.2 months (95% CI 28.1 to 48.3). Aseptic loosening of
the components was demonstrated intraoperatively in four
patients (3 in the femoral component and 1 in the tibial
component). In those UKRs with stable implants, intraoperative
findings included: synovitis with histology consistent with a
prominent foreign body reaction (n=2), and increased posterior
slope of the tibial cut (n=1). No clear cause was identified in
two patients.
Nine of the ten revisions were single-stage procedures. The
only two-stage revision was initially planned as a one stage
revision but converted after intra-operative findings of
widespread haemosiderin deposits. Subsequent microbiological
and histological investigations excluded infection. A primary
prosthesis was implanted in eight cases (7 AGCs Biomet, Bridgend
UK & 1 Kinemax Stryker Howmedica ), and a revision
implant with 10mm medial augments was required in two patients
for associated bone loss (Maxim Biomet, Warsaw, IN). There were
no revisions for infection.
Amongst the ten patients revised for ongoing pain nine had a
significant improved in symptoms, with complete resolution of
symptoms in seven. One patient had non-specific ongoing
symptoms whilst another complained non-dermatomal pain. Both
considered these symptoms acceptable. The final patient with a
poor outcome had an encouraging improvement in symptoms
initially, but after a fall within eight weeks of his revision
developed symptoms consistent with complex regional pain
syndrome.
The early re-operation rate following Oxford unicompartmental
knee replacement in our unit is 4.5% (95% CI 2.4 to 6.5),
with a revision rate of 2.6% (95% CI 1.0 to 4.2) after a mean (±SD)
follow-up of 40.1 (±16) months.
Discussion :
The ideal indication for unicompartmental knee replacement is
“anteromedial arthritis”.8 Clinically this equates
to an intact anterior cruciate ligament, varus deformity that is
correctable at 20° flexion, functionally normal medial
collateral ligament and full thickness cartilage in the lateral
compartment. Chondral ulcers on the medial aspect of the
lateral femoral condyle and patellofemoral arthritis are not
considered contraindications by the Oxford group.9
The Oxford group state that using the above criteria, 1 in 3
knees suitable for arthroplasty are appropriate for their
implant.5 The current phase III Oxford implant was
introduced in 1998 and is implanted using minimally invasive
techniques. In the Oxford knee this is associated with half the
recovery time of the full arthrotomy, and one-third the recovery
time of a total knee arthroplasty.10
Despite the encouraging results with the Oxford unicompartmental
knee replacement (UKR) only 8% of all primary knee arthroplasty
are unicompartmental, of which 72% are the Oxford phase III
implant.4 There are a combination of design,
philosophical and clinically-related reasons that some surgeons
limit their own indications for the implantation of a
unicompartmental knee replacement. Technically, unicompartmental
arthroplasty is more challenging than a total arthroplasty as
exact soft tissue balancing is required.11 The
addition of a mobile bearing to the Oxford design, with the
potential for dislocation, reduces the margin for error
further. Studies have shown that technical errors are the main
cause of early failure, long term studies have shown that if
survival is good at seven years then long term results are
likely to be good.10 This pattern of failure is
unique to congruent mobile bearing designs as wear rates are
low, which appears to have resulted in improved long term
results in comparison to other designs.2
The potential problem of persistent postoperative pain, with its
subsequent management challenges, has also raised concerns.
Failure to fully resolve all symptoms following a TKR is also
well recognised and once infection, aseptic loosening and gross
malalignment are excluded it is usually managed conservatively.
This course of action is realistically harder to follow in any
form of partial replacement, as the potential always exists for
further surgery to the unresurfaced components. However,
conservative measures are still usually recommended to
recipients of a UKR as they are to their TKR counterparts, with
advice that the symptoms are likely to settle with time or that
the symptoms are not amenable to surgical intervention.
Despite these reassurances there are a small number of patients
who consider their symptoms debilitating enough to warrant
further surgery. Clinically this group is often difficult to
manage appropriately.
The source of the persistent debilitating symptoms is not always
clear despite clinical examination, serial laboratory and
radiological investigations. In our specialist unit the
preferred primary re-operation chosen for persistent pain was
knee arthroscopy. Symptom improvement was only achieved in 2
out of 10 patients, both of whom had a clear pre-arthroscopy
diagnosis of loose cement fragments. In the remaining patients
symptoms did not improve significantly enough to prevent
revision to a TKR. Arthroscopic assessment further failed to
identify loose prostheses that were apparent at the time of
revision. Our findings would suggest that the role of
arthroscopy is limited in the management of a painful UKR as it
is a poor diagnostic and therapeutic modality.
The decision to revise to a total knee replacement is never
straightforward, for the patient it involves further major
surgery with no guarantee of symptom resolution and for the
surgeon it confirms failure of the original UKR. This difficult
decision is demonstrated in the mean 17-month interval between
the initial arthroscopy and subsequent revision. Despite these
misgivings our results are encouraging, with nine (90%) of
patients revised to TKR achieving clinically significant symptom
improvement, of which seven (70%) are pain free. Aseptic
loosening was the most consistent intra-operative finding
identified in four patients. The bone loss associated with
loosening was minimal, and only two cases required a revision
implant. Our findings would suggest that although the decision
to revise is initially disappointing there is a marked
improvement in symptoms.
Pandit5 reviewed 688 consecutive Oxford knee
replacements from the Oxford group: there were eight (1.2%)
revisions within 2.5 years of the index procedure and seven
other re-operations identified over an unspecified time period.
Indications for revision were infection in four cases, two
dislocated bearings and two for unexplained pain. Despite
revision surgery, pain persisted in one of these patients.
Re-operation was required for stiffness in four cases, pain
resulted in arthroscopy in two patients and one patient
underwent debridement for a superficial infection. It is not
clear from their data if the patients that were formally revised
to a total knee replacement underwent other procedures prior to
revision. Extrapolating their data, the presumed “best-case”
scenario for early re-operation is fifteen cases (2.2%) with a
revision rate of 1.2%.
Svärd’s3
series of 103 Oxford replacements identified three revisions
(2.9%) and one re-operation (0.9%) within two years of the index
procedure. The indications for revision were pain and clinical
suspicion of infection respectively. The re-operation was for a
suspected loose body, this was not located but symptoms
improved. No mention was made in the paper with respect to
complications of stiffness and the requirement for manipulation
under anaesthetic. Again it is not clear from their data if the
patients that were formally revised to a total knee replacement
underwent other procedures prior to revision. Extrapolating
their data the presumed “best-case” scenario for early
re-operation is four cases (3.8%) with a revision rate of 2.9%.
Reviewing the outcome of 381 Oxford knee replacements in
our institution, seventeen (4.5%) patients required
re-operations for persistent symptoms. In ten (2.6%)
patients a decision was been made to revise the primary implant
to a total knee replacement.
Our figures are higher than the extrapolated “best-case”
scenario data published from the design centre in Oxford5
(2.2% and 1.2%) and broadly comparable with the independent
series published by Svärd3 (3.8% and 2.9%).
Conclusions:
4.5% (95% CI 2.4% to 6.5%) of patients required a re-operation
for ongoing symptoms following an Oxford UKR. Our revision rate
is 2.6% (95% CI 1.0% to 4.2%), which is comparable to current
published data. Management of debilitating pain following
unicondylar knee surgery can be difficult. Arthroscopy is a
poor diagnostic and therapeutic modality for this clinical
problem, and only recommended if a correctible problem is
identified clearly prior (e.g. a loose body). Our results
suggest that if appropriate conservative measures have failed,
persistent pain is managed most reliably with revision to a
total knee replacement.
Reference:
-
Goodfellow J, O’Connor J.
The mechanics of the knee and prosthesis design. J Bone
Joint Surg (Br), 1978; 60-B:358-369
-
Murray D, Goodfellow J, O’Connor J.
The Oxford medial unicompartmental arthroplasty – a ten year
survival study. J Bone Joint Surg (Br), 1998; 80-B
(6):983-989
-
Svärd U, Price A.
Oxford medial unicompartmental knee arthroplasty. A survival
analysis of an independent series. J Bone Joint Surg (Br),
2001; 83:191-194
-
National Joint Registry for England and Wales 5th
annual Report 2008
-
Pandit H, Jenkins C, Barker K, Dodd C, Murray D.
The Oxford medial unicompartmental knee replacement using a
minimally-invasive approach. J Bone Joint Surg (Br), 2006;
88-B:54-60
-
Elsom DW, Brenkel IJ.
A Conservative approach is feasible in unexplained pain after
knee replacement. J Bone Joint Surg (Br), 2007; 89-B:1042-1045
-
Oxford™ Unicompartmental Knee: Manual of the Surgical
Technique, Biomet UK Ltd (UK)
-
White S, Ludkowski P, Goodfellow J.
Anteromedial osteoarthritis of the knee. J Bone Joint Surg
(Br), 1991; 73-B:582-586
-
D. J. Beard, H. Pandit, H. S. Gill, D. Hollinghurst, C. A. F.
Dodd, D. W. Murray.
The influence of the presence and severity of pre-existing
patellofemoral degenerative changes on the outcome of the
Oxford medial unicompartmental knee replacement. J Bone
Joint Surg Br, Dec 2007; 89-B: 1597 - 1601.
-
Price A, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW.
Rapid Recovery after Oxford unicompartmental arthroplasty
through a short incision. J Arthroplasty, 2001; 16:970-976
-
Robertsson O, Knutson K, Lewold S, Lidgren L.
The routine of surgical management reduces failure after
unicompartmental knee arthroplasty. J Bone Joint Surg Br,
2001, 83(1):45-4
|