|
Abstract:
Introduction: Distal radius fractures are among the most common
fractures of the upper extremity. In this study we compared the
functional outcome of treatment of distal radius fractures with
two different modalities, K-wire fixation with cast versus Ligamentotaxis.
Materials
and methods: Prospective study of Sixty five cases (40 males and
25 females) of intraarticular fractures of distal radius (Frykman
types 3 to 8) treated by percutaneus K wire-cast or external
fixator. Out of which 46 patients (25 male and 21 female)
underwent K wire-cast and 19 patients (15 male and 4 female)
underwent Ligamentotaxis with AO external fixator with
supplementing pinning. Patients were evaluated clinically and
functionally using Gartland and Werley Scoring system.
Results:
Mean age was 46.89 ± 14.75 years (range, 19 – 78 years) in K
wire-cast group and 42.84 ± 15.60 years (range, 23 – 79 years)
in Ligamentotaxis group. For the K wire-cast group the average
Gartland and Werley score was 85.45 ± 8.14 (range, 60-100
points) and average grip strength as measured by hand
dynamometer was mean 86.41 ± 8.73 % (range 60-100 %) of the
normal hand. Average Gartland and Werley score for the
Ligamentotaxis group was 83.03 ± 9.73 (range 50 – 97.5 points)
with average grip strength of 83.16± 9.01 % (range 65-95 %).
With an exception of reflex sympathetic dystrophy, which is an
important predictor of poor outcome, most complications were
minor and did not affect the end-result significantly.
Discussion:
There was no significant difference in results of K wire-cast
and Ligamentotaxis, though the complication rates (pin tract
infection) were slightly higher in external fixator group. Thus
both methods work well for selected distal end radius fractures
with acceptable clinical, functional results and low
complication rates.
J.Orthopaedics 2010;7(3)e3
Keywords:
distal end radius fracture; K wire and cast; ligamentotaxis;
Frykman classification; Gartland and Werley score
Introduction:
More than
195 years have passed since Colles described a fracture of the
distal end radius (DER).1
DER fractures are among the most common fractures of the upper
extremity. Comminuted fractures of the DER are caused by
high-energy trauma in young patients and by low-energy trauma in
the elderly, and present as shear and impacted fractures of the
articular surface of the distal radius with displacement of the
fragments.2-9
Management
of comminuted DER fractures continues to be a therapeutic
problem and challenge for the orthopedic surgeon. Impacted
intra-articular fractures have generated interest because of the
failure to reduce these fractures to within 2 mm of articular
congruity, has been shown to lead to symptomatic post-traumatic
arthritis.10 In a retrospective study of intra-articular
fractures of the distal radius in young adults, Knirk and
Jupiter11 found that if the fracture healed with
greater than 2mm of residual articular incongruity, 100% of
these patients had radiographic evidence of arthritis and
two-thirds were symptomatic. The fact that these articulations
are not weight-bearing does not exclude them becoming a major
source of disability if the articular anatomy is not restored.
Lafontaine et at12 studied 112 consecutive DER
fractures treated conservatively and suggested five factors that
could relate to instability following fracture reduction:
Initial dorsal angulation > 20 degrees, Dorsal metaphyseal
comminution, Intra-articular disruption, Associated ulnar
fracture, and Patients over 60 years of age with sever
osteoporosis.
Altissimi
et al13 further observed in a clinical review of 100
distal end radius fractures , that the severity of initial
radial shortening was the most reliable indicator of
instability. DePalma et al14 advocated that every
attempt be made to restore normal anatomy. He suggested that a
poor result was inevitable if "a
residual dorsal tilt of the radius > 30 degrees
and loss of the inward tilt of the
articular surface
of the radius exceeding 3mm" was
found. Bio mechanical cadaveric studies support
this clinical observation.15 It has been shown that
shortening of the distal radius by small amounts (2.5mm) and/or
the residual dorsal tilt results in a significant increase in
the axial load transmitted to the ulnar shaft.16,17
Also the dorsal tilt produces DRUJ incongruency and tightens the
interosseous membrane, causing limitation of forearm rotation.18
Thus, this increased ulnar load leads to degenerative arthritis
and pain on the ulnar side of the wrist.19
There are
various methods of reducing and maintaining the reduction of the
fracture published in the literature, which include the K-wire
and cast, percutaneus pinning, Plaster of Paris cast, open
reduction with internal fixation and external fixator or
distractor using the principles of ligamentotaxis. Percutaneus
pins to provide additional stability is minimally invasive and
has shown to give good results for extra-articular or simple
articular fractures.20 This however may not be strong
enough to prevent collapse. The need for application of cast may
lead to so called fracture disease and there are chances of pins
getting infected inside the cast.21
In
Ligamentotaxis the traction applied by the external fixator
produces tension in the intact ligaments and soft tissue
surrounding the bone which not only acts as a counter traction
but also aligns the displaced bone fragments. This
tissue tension is maintained over a period of time by external
fixator. This modality of treatment has been shown to be
effective in the surgical management of unstable, intra-articular
fractures of the distal radius but has also been linked with an
unacceptably high rate of complications in some series with most
important being collapse of the fracture.22,23 This
collapse may be secondary to stress relaxation of the soft
tissues over a period of time.24 To counter this
complication adjunct fixation with K wires is advocated. In
vitro cadaveric studies have concluded this method to give
stability similar to volar plating25 while clinical
studies have reported favorable outcomes.26,27
Both the
above mentioned techniques have been studied separately and no
comparative study is available. In this study we aim to compare
the functional outcome and complications associated with
treatment of DER with these two modalities.
Materials
and Methods:
Prospective
study of Sixty five cases of various fractures of the distal
radius was treated by percutaneus K wire-cast and external
fixator from July 2008 to April 2009. Frykman classification
system for distal end radius fractures was used in this study.28
Subjects with age >18 years, Frykman class type 3 to 8 and only
isolated injuries were included while volarly displaced
fractures, fractures with intra-articular comminution were
excluded
The series
includes 65 patients 40 males and 25 females. Out of which 46
patients (25 male and 21 female) underwent K wire-cast and 19
patients (15 male and 4 female) underwent Ligamentotaxis with AO
external fixator, with or without supplementing pinning. There
were 28 Left (20 for K wire-cast and 8 for Ligamentotaxis) and
37 right wrists (26 for K wire-cast and 11 for Ligamentotaxis).
The youngest was 19 while the oldest patient in this series was
79 years of age. The aims of treatment are to restore anatomy
(radial length and angles, articular surface congruity, DRUJ)
and to regain function. Key articular fragments are identified:
dorsoulnar, palmar-ulnar, hyperextended palmar fragment, radial
styloid, and impacted articular fragments. The three column
concept helps in developing an operative strategy for reduction
and stable fixation of the respective articular fragments. The
intermediate column is the key to the radiocarpal joint surface.
Surgical procedure:
Ligamentotaxis:
A
tourniquet was used at the discretion of the surgeon. The
external fixation group underwent closed reduction with the
placement of two pins in the base of the second metacarpal and
two in the distal third of the radius in a percutaneus or open
surgical manner. After application of the fixator if acceptable
alignment had been achieved, percutaneus K-wires were placed to
hold the reduction. The hand and forearm are placed in a bulky
soft dressing. No cast or splint is needed. The fingers are left
free for a full range of motion.
Percutaneus
pinning and cast: We used two or three Kirschner wires placed
across the fracture site, generally from the radial styloid,
directed proximally and from the dorsoulnar side of the distal
radial fragment directed proximally. Above elbow cast in
supination was applied in these patients
In
Ligamentotaxis group Passive and active range of motion
exercises were commenced the day of operation and on the 1st
post-operative day, the patient began training in activities of
daily living. Twice a day swabbing of the pin sites with
hydrogen peroxide was done for the first week.
10th day after the surgery, sutures are removed and pin site
care is continued. The fixation device is left in place for
an average 6 weeks (range 4 to 8 weeks) until both clinical and
radiographic evidence of healing is seen, depending upon the
surgeon's evaluation of the post-operative radiographs. At this
point, the external fixator is removed under sedation, and a
volar removable thermoplastic splint is given for 2 weeks. This
splint is removed regularly throughout the day for exercise.
Eight to ten weeks postoperatively, strengthening is begun and
ultimately, work and sports, hardening exercises are added.
For K-wire
cast group, Postoperative arm elevation is advised to alleviate
swelling. Careful watch for distal neurovascular compromise and
tightening of plaster is observed. Follow up is advised after 1
week for examination of cast. If cast is loosened then
reapplication of cast was done. At post op 3 weeks above elbow
cast is converted into below elbow cast. The cast is continued
for an average 6 weeks (range 4 to 8 weeks) until both clinical
and radiographic evidence of healing is seen, depending upon the
surgeon's evaluation of the post-operative radiographs. At this
time the K-wires were removed at an average 4 weeks (range 4 to
6 weeks). After cast removal gentle wrist Range of motion
exercises started. 8 to 10 weeks postoperatively, strengthening
is begun and ultimately, work and sports, hardening exercises
are added.
Follow up protocol:
All patients were called for follow up visits at 3 weeks, 6
weeks, 3 months, 6 months, 9 months and one year. The data was
quantified with the system of Gartland and
Werley29
in
which
clinical and
radiographic data are used.
The quality of recovery was determined by
range of motion, grip strength, peri and post-operative
complications, patient satisfaction and radiographic evaluation
by the modified Gartland and Werley's Wrist Grading System in
which equal emphasis is placed for a maximum possible findings —
each with 50 points for a maximum possible score of 100 points.
Antero-posterior and Lateral radiographs of the injured wrist
were used for various measurements. The radiographs made at the
time of the latest follow-up were evaluated for joint congruity.
Osteoarthritis of the radiocarpal and the distal radio-ulnar
joint was graded according to the criteria of Knirk and Jupiter3
at the latest follow- up evaluation with Grade 0- No
osteoarthritis; Grade I- Slight narrowing of the joint space;
Grade II- Marked narrowing of the joint space with osteophytes
formation; Grade III- Full thickness loss of articular
cartilage with formation of cysts and osteophytes.
Observations and
Results:
For the K wire-cast group the mean age was 46.89 ± 14.75 years
(range, 19 – 78 years), with 21 females and 25 males (Table 1).
The patients were followed up for an average of 11.85 ± 3.69
months (range, 6– 18 months).The average time required for
union of fracture in our series was 7.47 ± 0.99 weeks
(range,6.2 - 11.4weeks), Post operative average flexion 67.07 ±
9.64 degrees (range 50-80 degrees), average extension 73.15 ±
12.13 degrees (range 40-90 degrees), average Radial deviation
20.43 ± 3.63 degrees (range 15-25 degrees), average Ulnar
deviation 29.57 ± 4.45 degrees (range 20-35 degrees), average
pronation 73.48 ± 10.64 degrees (range 50-90 degrees), average
Supination 76.63 ± 9.07 degrees (range 50-90 degrees), average
grip strength as measured by hand dynamometer was 86.41 ± 8.73 %
(range 60-100 %), average Gartland and Werley score was mean
85.45 ± 8.14 (range, 60-100 points).
|
Variable |
K
wire-cast |
Ligamentotaxis |
|
Age years– mean (range) |
46.89
( 19 – 78) |
42.84
( 23 – 79) |
|
Male:
Female |
25 :
21 |
15: 4 |
|
Frykman Class
IV:V:VI:VII:VIII |
1:22:3:14:6 |
0:0:1:4:14 |
|
Follow up time |
11.85 |
11.21 |
|
Union
time |
7.47 |
7.17 |
|
Gartland and Werley score |
85.45
points |
83.03
points |
|
Results- Excellent:Good:Fair:Poor |
15:23:7:1 |
2:13:3:1 |
Table 1:
Demographical details of the entire sample population
For the
Ligamentotaxis group the mean age was 42.84 ± 15.60 years
(range, 23 – 79 years), with 4 females and 15 males. The
patients were followed up for an average of 11.21 ± 3.98
months (range, 6– 17 months).The average time required for
union of fracture in our series was 7.17 ± 0.69 weeks (range,
6.5 – 7.6 weeks),. Post operative average flexion 63.95 ± 8.91
degrees (range 40-75 degrees), average extension 69.47 ± 11.17
degrees (range 40-85 degrees), average radial deviation 18.16 ±
3.42 degrees (range 15-25 degrees), average ulnar deviation
27.11 ± 4.81 degrees (range 15-35 degrees), average pronation
70.00 ± 9.57 degrees (range 50-90 degrees), average supination
74.74 ± 10.07 degrees (range 50-90 degrees), average grip
strength as measured by hand dynamometer 83.16± 9.01 % (range
65-95 %),average Gartland and Werley score was mean 83.03 ± 9.73
(range 50 – 97.5 points). There was no significant difference in
postoperative flexion (p value 0.229), extension (p value
0.224), ulnar deviation (p value 0.052), Pronation (p value
0.159) and supination (p value 0.270) between two groups. The P
value 0.022 for postoperative radial deviation between two
groups was significant however there was no difference in the
functional scoring (Table 2). Figure 1 and 2 show two patients
of this series treated with either technique.
|
Variables |
GROUP |
N |
Mean |
SD |
‘p’
value |
|
Age
(years) |
K-wire and cast |
46 |
46.89 |
14.744 |
.326
|
|
|
Ligamentotaxis |
19 |
42.84 |
15.600 |
|
Follow up duration (months)
|
K-wire and cast |
46 |
11.85 |
3.688 |
.538 |
|
Ligamentotaxis |
19 |
11.21 |
3.980 |
|
Union
time (weeks)
|
K-wire and cast |
46 |
7.463 |
.9956 |
.244
|
|
Ligamentotaxis |
19 |
7.168 |
.6896 |
|
Postoperative Flexion (degrees)
|
K-wire and cast |
46 |
67.07 |
9.64 |
.229 |
|
Ligamentotaxis |
19 |
63.95 |
8.91 |
|
Postoperative Extension (degrees)
Flexion |
K-wire and cast |
46 |
73.15 |
12.127 |
.244
|
|
Ligamentotaxis |
19 |
69.47 |
11.171 |
|
Postoperative Radial deviation (degrees)
|
K-wire and cast |
46 |
20.43 |
3.625 |
.022 |
|
Ligamentotaxis |
19 |
18.16 |
3.420 |
|
Postoperative Ulnar deviation (degrees)
|
K-wire and cast |
46 |
29.57 |
4.450 |
.052
|
|
Ligamentotaxis |
19 |
27.11 |
4.806 |
|
Postoperative Pronation (degrees) |
K-wire and cast |
46 |
73.48 |
10.639 |
.159 |
|
Ligamentotaxis |
19 |
70.00 |
9.571 |
|
Postoperative Supination (degrees)
Su |
K-wire and cast |
46 |
76.63 |
9.072 |
.270 |
|
Ligamentotaxis |
19 |
74.74 |
10.071 |
|
Grip
strength
(% of
normal side)
|
K-wire and cast |
46 |
86.41 |
8.732 |
.123
|
|
Ligamentotaxis |
19 |
83.16 |
9.013 |
|
Scoring points |
K-wire and cast |
46 |
85.45 |
8.141 |
.242 |
|
Ligamentotaxis |
19 |
83.03 |
9.739 |
Table 2:
Statistical comparison of various clinical variables using
unpaired t test.
Figure
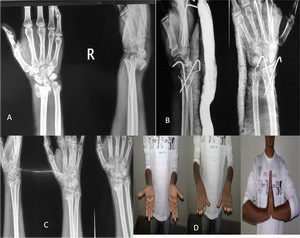
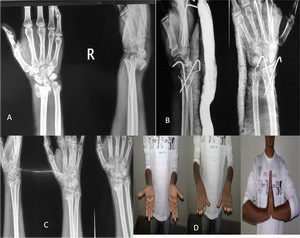
1: Twenty two year male having frykman’s class VI distal
fracture treated with K wire and casting with good functional
outcome at one year follow up
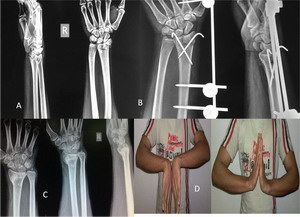
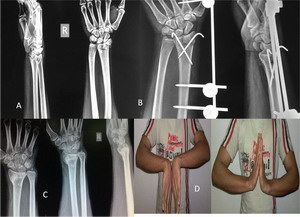
Figure
2: Twenty seven year old male having Frykman class
VIII fracture treated with external fixator having excellent
functional outcome at one year follow up
Fifteen of
the 46 patients (32.6 %) treated with an K wire-cast and 2 out
of 19 patients (10.5 %) treated with external fixator
supplemented with percutaneus pinning were rated having
excellent results according to the modified Gartland and Werley
scoring system. Rest is as seen in table I
There was 1
poor result out of 46 (2.2 %) in K wire cast group in 78 year
old lady with severe osteoporosis and pin tract infection at one
year follow up. One poor result out of 19 (5.3 %) in
Ligamentotaxis group - Reflex Sympathetic Dystrophy was noted
in one case in 67 year old male and was treated conservatively.
The average grip strength exceeded 80% in comparison with that
of the contralateral, unaffected hand, with a range of 60 to
100%.
Complications:
There were 4 pin tract infections in K wire cast group and 7 pin
tract infection in Ligamentotaxis group; which resolved with
local wound care and oral antibiotic therapy. No loss of
reduction was observed. No pin breakage, iatrogenic fractures,
persistent neuropathy was observed. Patient satisfaction was
consistently high, although a variable degree of morning
stiffness in the wrist was experienced in older patients. All of
these patients returned to their former activities of daily
living with no significant limitations, and no secondary
operations have been required. With an exception of reflex
sympathetic dystrophy, which is an important predictor of poor
outcome, most complications were minor and did not affect the
end-result significantly.
Discussion :
Distal end
radius fractures are one of the most common and most challenging
fractures. Closed reduction with K wire fixation and cast is one
of the most frequently used minimally invasive methods while
Ligamentotaxis offers advantage of neutralization of the axial
load achieving indirect reduction . We studied both these
methods with respect to their outcomes and complications.
The two
main operative procedures for an unstable distal end radius
fractures are closed reduction and internal fixation and open
reduction and internal fixation (ORIF). Strohm et al30
showed that K wire cast is more superior than cast only, in
treatment of distal end radius fractures. Among the closed
methods external fixation allows controlled distraction and more
accurate positioning than pins and cast, however there were more
complication associated with external fixation than K wire cast.
Kaempfie31 et al discovered that an increase in the
duration and amount of distraction of distal radial fractures
treated by external fixation adversely affected the final range
of motion of the wrist, function, grip strength and the level of
pain. In our series the Ligamentotaxis group had significantly
less radial deviation (p <.05) than compared with the K wire
group. Also the range of ulnar deviation approached statistical
significance (p – 0.052). The other factors like the union time
and range of flexion extension and pronation - supination were
similar in both the groups. We successfully restored radial
length, angulation and articular congruity in most cases. The
average residual dorsal angulation was 10 degree. Failure to
correct this deformity fully confirms the conclusion by Bartosh
and Saldana32 that ligamentotaxis alone is unreliable
in reestablishing radiopalmar tilt and so recommend using
percutaneus K wires along with ligamentotaxis. All of these
patients returned to their former activities of daily living
with no significant limitations, and no secondary operations
have been required to date. Our results are comparable with
review done by Handall et al33 in which two trials
comparing a bridging (of the wrist) external fixator versus pins
and plaster found no significant differences in function or
deformity. Thus, K wire-cast and external fixation supplemented
by percutaneus pinning both were found to be a safe and
reliable method for treatment of comminuted distal radial
fractures and the decision generally lies with the surgeon to
choose the appropriate treatment modality for individual
patients. Even though some motion is lost, 75% recovery of
mobility and grip strength can be anticipated. The complication
rates were quite low in our series with pin tract infection most
common. Careful assessment of the fracture pattern, patient
selection, meticulous surgical technique, appropriate choice of
fixation device and pins, recognition the need for augmentation
with limited internal fixation and aggressive post- operative
rehabilitation provide foundation for successful management of
these fractures while minimizing complications.
Our study
has few shortcomings. The small sample size and unequal patient
distribution in the two groups are the main issues; however we
believe that the study offers useful insights for management of
distal end radius fractures.
Reference:
-
The
classic. On the fracture of the carpal extremity of the
radius. Abraham Colles, Edinburgh Med. Surg. J., 1814. Clin
Orthop Relat Res. 1972 Mar-Apr;83:3-5.
-
Cooney
WP, Berger RA. Treatment of complex fractures of the distal
radius. Combined use of internal and external fixation and
arthroscopic reduction. Hand Clin. 1993 Nov;9(4):603-12.
-
Knirk JL,
Jupiter JB. Intra-articular fractures of the distal end of the
radius in young adults. J Bone Joint Surg Am. 1986
Jun;68(5):647-59.
-
Lozano-Calderon SA, Doornberg J, Ring D (2006) Fractures of
the dorsal articular margin of the distal part of the radius
with dorsal radiocarpal subluxation. J Bone Joint Surg Am
88:1486–1493.
-
Mehta JA,
Bain GI, Heptinstall RJ. Anatomical reduction of intra-articular
fractures of the distal radius. An arthroscopically-assisted
approach. J Bone Joint Surg Br. 2000 Jan;82(1):79-86.
-
Melone CP
Jr. Distal radius fractures: patterns of articular
fragmentation. Orthop Clin North Am. 1993 Apr;24(2):239-53.
-
Ring D,
Prommersberger K, Jupiter JB. Combined dorsal and volar plate
fixation of complex fractures of the distal part of the
radius. J Bone Joint Surg Am. 2004 Aug;86-A(8):1646-52.
-
Rogachefsky
RA, Lipson SR, Applegate B, Ouellette EA, Savenor AM,
McAuliffe JA. Treatment of severely comminuted intra-articular
fractures of the distal end of the radius by open reduction
and combined internal and external fixation. J Bone Joint Surg
Am. 2001 Apr;83-A(4):509-19.
-
Ruch DS,
Weiland AJ, Wolfe SW, Geissler WB, Cohen MS, Jupiter JB.
Current concepts in the treatment of distal radial fractures.
Instr Course Lect. 2004;53:389-401.
-
Haus BM,
Jupiter JB. Intra-articular fractures of the distal end of the
radius in young adults: reexamined as evidence-based and
outcomes medicine. J Bone Joint Surg Am. 2009
Dec;91(12):2984-91.
-
Knirk JL,
Jupiter JB. Intra-articular fractures of the distal end of the
radius in young adults. J Bone Joint Surg Am. 1986
Jun;68(5):647-59.
-
Lafontaine M, Hardy D, Delince P. Stability assessment of
distal radius fractures. Injury. 1989 Jul;20(4):208-10.
-
Altissimi
M, Mancini GB, Azzarà A, Ciaffoloni E. Early and late
displacement of fractures of the distal radius. The prediction
of instability. Int Orthop. 1994 Apr;18(2):61-5.
-
DePALMA
AF. Comminuted fractures of the distal end of the radius
treated by ulnar pinning. J Bone Joint Surg Am. 1952
Jul;24-A-3:651-62.
-
Short WH,
Palmer AK, Werner FW, Murphy DJ. A biomechanical study of
distal radial fractures. J Hand Surg Am. 1987
Jul;12(4):529-34.
-
Peltier
LF. Fractures of the distal end of the radius. An historical
account. Clin Orthop Relat Res. 1984 Jul-Aug;(187):18-22.
-
Simic PM,
Weiland AJ. Fractures of the distal aspect of the radius:
changes in treatment over the past two decades. Instr Course
Lect. 2003;52:185-95.
-
Kihara H,
Palmer AK, Werner FW, Short WH, Fortino MD. The effect of
dorsally angulated distal radius fractures on distal
radioulnar joint congruency and forearm rotation. J Hand Surg
Am. 1996 Jan;21(1):40-7.
-
Bushnell
BD, Bynum DK. Malunion of the distal radius. J Am Acad Orthop
Surg. 2007 Jan;15(1):27-40.
-
Allain J,
le Guilloux P, Le Mouël S, Goutallier D. Trans-styloid
fixation of fractures of the distal radius. A prospective
randomized comparison between 6- and 1-week postoperative
immobilization in 60 fractures. Acta Orthop Scand. 1999
Apr;70(2):119-23.
-
Weber SC,
Szabo RM. Severely comminuted distal radial fracture as an
unsolved problem: complications associated with external
fixation and pins and plastertechniques. J Hand Surg Am. 1986
Mar;11(2):157-65.
-
Cooney WP
3rd, Dobyns JH, Linscheid RL. Complications of Colles'
fractures. J Bone Joint Surg Am. 1980;62(4):613-9.
-
Jupiter
JB, Fernandez DL. Complications following distal radial
fractures. Instr Course Lect. 2002;51:203-19.
-
Sun JS,
Chang CH, Wu CC, Hou SM, Hang YS: Extra-articular deformity in
distal radius fractures treated by external fixation. Can J
Surg 2001;44:289-294
-
Dunning
CE, Lindsay CS, Bicknell RT, Patterson SD, Johnson JA, King GJ.
Supplemental pinning improves the stability of external
fixation in distal radius fractures during simulated finger
and forearm motion. J Hand Surg Am. 1999 Sep;24(5):992-1000.
-
Geissler
WB, Fernandes D. Percutaneous and limited open reduction of
intra-articular distal radial fractures. Hand Surg. 2000
Dec;5(2):85-92.
-
Seitz WH
Jr, Froimson AI, Leb R, Shapiro JD. Augmented external
fixation of unstable distal radius fractures. J Hand Surg Am.
1991 Nov;16(6):1010-6.
-
Bradway
JK, Amadio PC, Cooney WP. Open reduction and internal fixation
ofdisplaced, comminuted intra-articular fractures of the
distal end of the radius. J Bone Joint Surg Am. 1989
Jul;71(6):839-47.
-
Gartland
JJ Jr, Werley YCW. Evaluation of healed Colles' fractures. J
Bone Joint Surg Am. 1951 Oct;33-A(4):895-907.
-
Strohm
PC, Müller CA, Boll T, Pfister U. Two procedures for Kirschner
wire osteosynthesis of distal radial fractures. A randomized
trial. J Bone Joint Surg Am. 2004 Dec;86-A(12):2621-8.
-
Kaempffe
FA, Wheeler DR, Peimer CA, Hvisdak KS, Ceravolo J, Senall J.
Severe fractures of the distal radius: effect of amount and
duration of external fixator distraction on outcome. J Hand
Surg Am. 1993 Jan;18(1):33-41.
-
Bartosh
RA, Saldana MJ. Intraarticular fractures of the distal radius:
a cadaveric study to determine if ligamentotaxis restores
radiopalmar tilt. J Hand Surg Am. 1990 Jan;15(1):18-21.
-
Handoll
HH, Madhok R. Surgical interventions for treating distal
radial fractures in adults. Cochrane Database Syst Rev.
2003;(3):CD003209.
|