|
Abstract:
Surgical
treatment of Osgood-Schlatter disease is rarely indicated, as
most patients become asymptomatic after skeletal maturity and
fusion of the proximal tibial apophysis. Some patients with
separated mobile ossicles have persistent pain with kneeling and
direct pressure over the tibial tubercle. We describe the
results of simple excision of the mobile ossicles in 22 patients
with a mean age of 18 years after skeletal maturity. All but one
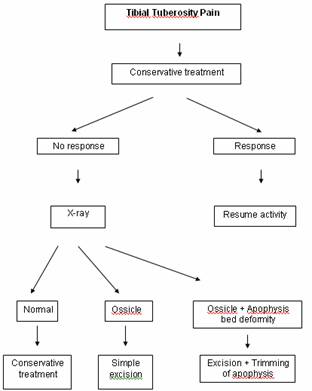
were satisfied with the results of the surgery. An algorithm for
treatment and surgical technique is presented.
J.Orthopaedics 2010;7(3)e12
Keywords:
Knee pain;
Osgood-Schlatter disease; Tibial apophysis
Introduction:
Osgood-Schlatter
disease (OSD) is a well known condition, characterized by pain
over the tibial tubercle with subsequent tubercle prominence.
The disease starts in the second decade of life and usually
resolves spontaneously without sequelae by the time of skeletal
maturity. Boys in the early second decade of life are
predominantly affected. Less than one-quarter of patients
develop pain over the tibial tubercles [1]. Initially, the
tibial tubercle is painful following physical activity and
gradually becomes prominent and constantly painful. Radiological
examination demonstrates a round regular ossification over the
tubercle. Treatment is symptomatic and includes modification of
physical activity, ice, non steroidal anti inflammatory drugs,
braces and pads. In the majority of the cases, symptoms resolve
after physeal closure without the need for specific treatment
and rarely do patients require surgical intervention. There are
few reports in the literature about surgical treatment of OSD,
usually due to the development of a painful ossicles in patients
who did not respond to conservative treatment [2, 3]. We report
our experience in OSD patients who were refractory to
conservative treatment modalities, with clinically evident
mobile ossicles and radiological confirmation of the
presence of a free osseous fragment.
Materials
and Methods:
Between
January 2000 and May 2006, we treated surgically 23 knees in 22
patients with painful bursitis over the tibial tubercle (Table
1). Of these, 21 were males and one was a female. Patients had a
documented history of OSD with recurrent pain for an average
period of 22 months prior to surgery. Average age at surgery was
18 years, and the average follow up period was 38 month. All
were treated in the acute phase by a conservative protocol that
included three weeks of complete activity restriction, a course
of topical and oral NSAID, and infra-patellar braces. Inclusion
criteria were: age over 16 years, painful bursitis over the
tibial tubercle after failure of initial conservative treatment
of 3 months, radiological evidence of osseous fragment anterior
to the tibial tubercle, and closure of growth plates.
Operative technique
Eighteen patients were operated under local anesthesia with
Esracain 1% and Adrenalin 1:10.000, and four were under general
anesthesia. A small longitudinal skin incision over the tibia
tubercle was performed with exposure of the patellar tendon at
the site of insertion to the tubercle. A longitudinal, as
sparing as possible, fiber-splitting incision of the patellar
tendon followed by subperiosteal undermining at either side of
the osseous fragment was completed .The plain of cleavage
between the bony bed and the mobile fragment was isolated by
sharp dissection. Final removal of the osseous fragment from its
bony bed was completed by delivery with a blunt instrument. Soft
dressing was applied for the first few days. Patients were
encouraged to resume daily activity immediately after surgery.
Results :
Surgical treatment is rarely indicated for OSD due to excellent
pain relief after conservative treatment. Most patients become
asymptomatic after naturally occurring fusion of the proximal
tibial apophysis. Several studies showed that patients who did
not respond to conservative treatment had a mobile osseous
fragment which caused pain during direct pressure on the
tubercle and upon kneeling [3-6].
Only
rarely do some patients remain symptomatic. Approximately 10% of
osseous fragments fail to unite with the tibia tubercle, and
patients with this condition experience anterior knee pain even
with mild activity but especially with kneeling [2,3,7].
Typically, their symptoms relate to the persistence of the
separate mobile osseous fragment. These patients are the core of
our study.
There
is no consensus about definitive treatment of residual OSD.
Trail [1] compared two groups of patients with symptomatic OSD
over a 4-5 year follow-up period. One group was treated by
tibial sequestrectomy and one group was treated conservatively.
Sequestrectomy did not offer significant benefit over
conservative treatment and a significant complication rate was
reported. Ferciot and Thompson described excision of the
ossicles without excision of the tibia tubercle prominence
[8,9]. Flowers and Bhadreshwar reported results of a modified
Ferciot procedure in 35 patients [3].They achieved pain relief
in 95% of patients and reduction of the prominence in 85% with
minimal complications. Orava et al [5] summarized their
experience with 70 operations on 67 patients with late
unresolved OSD. Mean age of their patients was 19.6 years.
Excision was performed in 62 cases. The reported outcome was
excellent or good in 56 cases, moderate in 9, poor in 3 and
unknown in 2 patients. Binazzi et al [4] described surgical
treatment of 15 patients with OSD. There was one fair and no
poor result. The authors concluded that removal of all loose
intratendinous ossicles associated with prominent tibial
tubercles is the procedure of choice, both from the functional
and cosmetic points of view. Mital et al [2] reviewed a cohort
of 118 patients with OSD. Fourteen patients (fifteen knees) had
a distinct and separate ossicle at the proximal aspect of the
tibial tubercle. Resection of the ossicles brought relief of
symptoms. The authors concluded that unresolved OSD patients
suffered from avulsion of the proximal cartilaginous part of the
tibia tubercle and should be treated by surgical excision.
We
describe the results of treatment in 22 young adult patients
with known OSD treated by simple excision of mobile ossicles.
All our patients suffered from pain with kneeling and direct
pressure over the ossicles. All patients were mature or at the
end of skeletal maturity according to their physis appearance.
Sixteen patients had a clinically mobile ossicle and all but one
showed clear separation of the ossicles from the tibial tubercle
(Fig. 1). Based on our experience, we have devised a treatment
algorithm (Fig. 2). We believe that the key factors for
successful surgical treatment are clear visualization of
separation on lateral knee x-ray view and a clinical mobility
positive test (firm grasping of the prominent part of the
tubercle and its sliding movement). Our results are uniformly
good; the only one failure related to mistaken inclusion
criteria where the lateral x-ray did not show clear ossicle
separation.
Discussion :
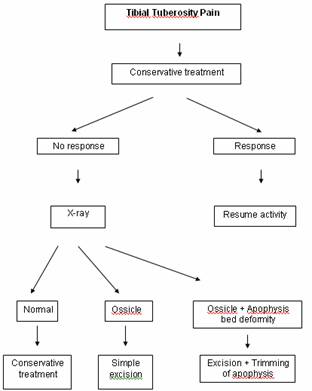
Figure 1:
Appearance
of free ossicle and spiky deformity of the underlying apophysis

Figure 2:Treatment
algorithm
Reference:
-
Trail
IA (1988) Tibial sequestrectomy in the management of Osgood-Schlatter
disease. J Pediatr Orthop 8:554-557
-
Mital
MA, Matza RA, Cohen J (1980) The so-called unresolved Osgood-Schlatter
lesion: a concept based on fifteen surgically treated lesions.
J Bone Joint Surg Am 62:732-739
-
Flowers
MJ, Bhadreshwar DR (1995) Tibial tuberosity excision for
symptomatic Osgood-Schlatter disease. J Pediatr Orthop
15:292-297
-
Binazzi
R, Felli L, Vaccari V, Borelli P (1993) Surgical treatment of
unresolved Osgood-Schlatter lesion. Clin Orthop Relat Res
289:202-204
-
Orava
S, Malinen L, Karpakka J, Kvist M, Leppilahti J, Rantanen J,
Kujala UM (2000) Results of surgical treatment of unresolved
Osgood–Schlatter lesion. Ann Chir Gynaecol 89:298-302
-
Robertsen K, Kristensen O, Sommer J (1996) Pseudoarthrosis
between a patellar tendon ossicle and the tibial tuberosity in
Osgood-Schlatter's disease. Scan J Med Sci Sports 6:57-59
-
Lynch
MC, Walsh HP (1991) Tibia recurvatum as a complication of
Osgood-Schlatter's disease: a report of two cases. J Pediatr
Orthop 11:543-544
-
Ferciot
CF (1995) Surgical management of anterior tibial epiphysis.
Clin Orthop 5:204-206
-
Thompson JEM (1956) Operative treatment of osteochondritis of
the tibial tubercle. J Bone Joint Surg Am 38:142-148
|