|
Abstract:
The time at which patients should drive following total hip
replacement (THR) is dependant upon recovery and the advice they
are given. The Driver Vehicle and Licensing Agency (DVLA) do not
publish recommendations following THR and insurance companies
usually rely on medical instruction.
Brake reaction times for patients undergoing THR were measured
before and four, six and eight weeks after surgery using a
vehicle driving simulator. Patients were prospectively
recruited. Ethical approval was granted. Participants included
eleven males and nine females, mean age 69 years. Side of
surgery, frequency of driving and type of car (automatic or
manual) were documented. Patients with postoperative
complications were excluded. No adverse events occurred during
the study.
Statistical analysis using Friedman’s test demonstrated a
statistically significant difference (P=0.015) in reaction times
across the four time periods. Wilcoxon test demonstrated a
highly significant difference between initial and six week mean
results (P=0.003), and between four and six week results
(P=0.001). No significant difference was found between six and
eight weeks.
Our data suggests reaction times improve until week six and
significantly between week four to six. Patients making an
uncomplicated recovery should be considered safe to drive by
week six.
J.Orthopaedics 2010;7(2)e6
Keywords:
Total hip replacement, total hip arthroplasty, hip, reaction
times.
Introduction:
The point at which patients can return to driving following
total hip arthroplasty (THA) is a common question. The answer is
not so simple1. In order to drive a car, the patient
must be able to physically transfer into the vehicle, obtain a
comfortable driving position and have full command of the
operative controls. Failure to do so could be catastrophic on
the road. Patient factors such as postoperative pain, mobility
and the desire to avoid dislocation must all be taken in account
when advising a return to driving2. These multiple
factors are difficult variables to measure. Arguably, the most
important driving command, with reference to the lower limb, is
the ability to perform an emergency stop and brake. This can be
measured in the form of a driver reaction time. The driver
reaction time, or emergency braking stop, is comprised of the
neurological reaction time, the time taken for the driver to
recognise the danger and decide to apply the brake, the transfer
time as the foot is moved from accelerator to brake and the
brake time as the brake is depressed from zero until the point
at which the brakes are fully applied3. According to
the Highway Code, the national average is 0.7 seconds4.
There is also a legal standpoint to consider. Many insurance
companies will look to the surgeon to provide advice as to when
a patient may return to driving, as naturally this is dependant
on the type and extent of the surgical procedure. The surgeon
may decide to refer to a national agency for guidance, such as
the Driver and Vehicle Licensing Agency (DVLA) in the United
Kingdom (UK). The DVLA offer guidance to doctors on over one
hundred and forty different medical and surgical conditions, but
not specifically following total hip arthroplasty. The most
recent guide published in February 20095 states that
licence holders wishing to drive after surgery (generic,
without specific reference to THA), should establish with
their doctor when it is safe to do so and should check their
insurance policy. In the absence of firm guidance from the DVLA,
the surgeon could review the literature for the answer, though
predictably this is also a little grey. Few studies have tackled
this question and those that have, reported different
conclusions. In a study from the Oxford Orthopaedic Engineering
Centre, Macdonald and Owen6 concluded from
their study of twenty-five patients, that most were safe to
return to driving from week eight. In a sponsored American study
of ninety patients, Ganz and Levin7 concluded
that patients manage to achieve their preoperative reaction time
at weeks four to six, and improve thereafter.
At our own institution, we allow patients making a satisfactory
recovery to return to driving at six weeks. This is based
loosely around choosing the mid-point of the studies above and
as our follow-up clinics occur at week six. We recognised this
practise needed to be evidenced based, and performed our own
study based around driving reaction times following THA. Our
aims were to evaluate if our current practise was safe, and in a
similar fashion to previous studies, determine at which point
there is a significant improvement in postoperative reaction
times.
Materials
and Methods:
We were fortunate to be granted access to a driving simulator
(Media in Progress, Srl, 00165, Roma, Italy) at a regional
mobility centre. The driving simulator is used on a daily basis
in the assessment of fitness to drive. A single driving
consultant whom is familiar with the equipment and processes
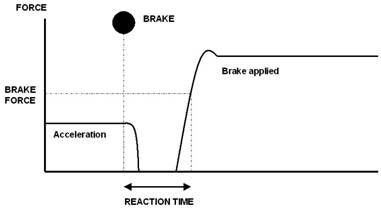
involved, was recruited to perform our testing. Subjects were
asked to accelerate to a constant speed of thirty miles per hour
(mph) and perform an emergency braking stop when signalled to do
so by a random red light, located on top of the apparatus
(figure 1).
Figure 1. Driving vehicle simulator

In order for their attempt to be registered a successful,
subjects had to achieve a minimum brake pressure of one hundred
and fifty Newton metres (Nm). Subjects were permitted two
unrecorded practise attempts to familiarise themselves with the
process, followed by three recorded attempts. Unsuccessful
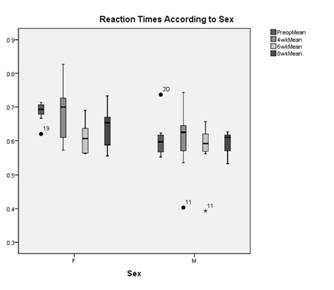
attempts were recorded as such. The total reaction time,
including neurological time, transfer time and the time taken
between applying the brake and achieving 150 Nm, the brake time
was recorded as one measurement in seconds (figure 2). Patients
were assessed pre-operatively and at four, six and eight weeks
post-operatively.
Figure 2. Driving reaction time
Patients were recruited on a voluntary basis prospectively. All
patients undergoing primary total hip arthroplasty using a
stemmed prosthesis were eligible. Patients undergoing total hip
resurfacing or a revision procedure were not eligible. Patients
were recruited at random, from either of our institutions two
pre- assessment clinics. Upon receiving a hospital letter
stating the date of pre-assessment, an information leaflet
regarding the research was also included. After formal
pre-assessment had finished, patients were asked if they wished
to volunteer for the study by a pre-assessment nurse, who had
been fully briefed regarding the study eligibility criteria and
design requirements. Patients requiring further information were
given the telephone number of an investigating doctor to
contact. All patients entering the study were fully consented
regarding the potential risks and free to withdraw at any point.
Recruited patients were provided with appointments for pre and
post-operative assessment at the mobility centre. No incentives
were offered for recruitment and patients received their surgery
according to their place on the waiting list. The operative
surgeon was not informed of individual patient recruitment into
the study in an attempt to avoid bias. Exclusion criteria
mid-study included any patient that experienced a serious
post-operative complication, as participation may compromise
recovery and jeopardise the validity of the results. Ethical
approval for the study was obtained.
Results :
In total 20 patients were recruited comprising of 9 females and
11 males with a mean age of 69 years (range 53-78). The primary
diagnosis in all cases was osteoarthritis. Of the patients, 5
had a left sided procedure and the remaining 15 a right-sided
procedure. With regards to driving practises, 12 patients drove
an automatic vehicle and the remainder a manual. The majority of
patients, 14, drove more than six times per week, 5 two to four
times per week and 1 patient only drove once to twice per week.
No complications were experienced during testing. Of the 20
patients, 15 completed the full remit of testing preoperatively
and at four, six and eight weeks. Five patients completed
testing preoperatively, at four weeks and six weeks, but did not
attend for final testing at eight weeks. All patients tested
managed to record three successful reaction times at their
respective time periods. Not once did any patient record an
unsuccessful attempt.
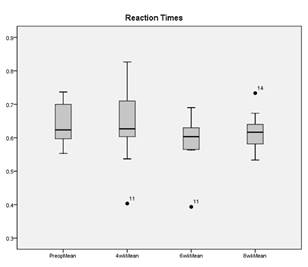
The statistical analysis was overseen by our institutions onsite
statistician using SPSS software (version 16, SPSS Inc, Chicago,
Illinois, USA). The three-recorded reaction times from each
patient for each time period, were tabulated in order to
calculate the overall mean reaction time (table I).
Table I: Mean reaction times for each time period.
|
Mean Reaction Times |
|
|
N |
Minimum |
Maximum |
Mean |
Std. Deviation |
|
PreopMean |
20 |
.55 |
.74 |
.6427 |
.06361 |
|
@4wkMean |
20 |
.40 |
.83 |
.6307 |
.09203 |
|
@6wkMean |
20 |
.39 |
.69 |
.5867 |
.06740 |
|
@8wkMean |
15 |
.53 |
.73 |
.6144 |
.05159 |
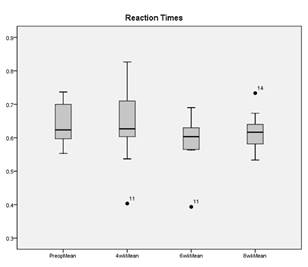
Given that our data set was small and therefore not normally
distributed, non-parametric testing was used. Friedman’s test
demonstrated a significant difference of 0.015 across all
four-time periods, but did not reveal at which interval.
Wilcoxon signed rank tests were used to analyse the intervals
and found a highly significant difference between the
pre-operative and 6 week time period (P=0.003) and between weeks
4 and 6 (table 2).
Table 2. Analysis of reaction times across time periods
|
Wilcoxon Signed Ranks Test |
| |
PreopMean
- @4wkMean |
PreopMean - @6wkMean |
PreopMean
- @8wkMean |
@4wkMean - @6wkMean |
@4wkMean - @8wkMean |
@6wkMean - @8wkMean |
|
P= |
.550 |
.003 |
.125 |
.001 |
.061 |
.245 |
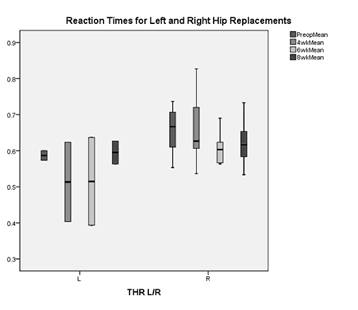
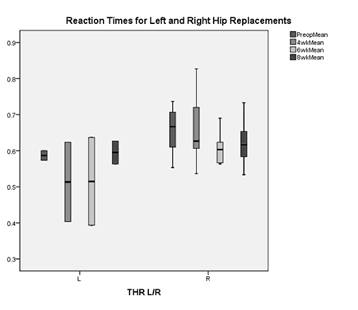
Figure 3. Reaction times according to sex
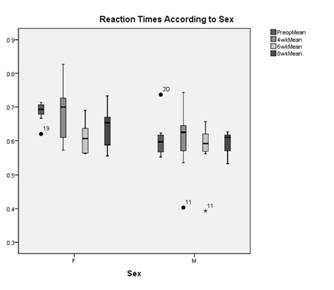
Figure 4. Reaction times for left and right hip replacements
Discussion :
With reference to our study aims, we feel our results
demonstrate that reaction times do improve with time, and
significantly improve by week six. We were particularly
encouraged to find such a highly significant improvement between
the preoperative and six weeks time period and across the four
to six week interval. Review of individual mean scores for each
patient at week seix revealed no score above the 0.7 second
average reaction time in the Highway Code, suggesting that all
patients in our study would have had satisfactory reaction times
to return to driving at that stage. This does however raise the
question of why we did not find statistically significant
results at eight weeks, though the mean score was 0.61 seconds.
We believe this is due to the smaller sample size of only
fifteen patients that completed testing at week eight. Analysis
of individual patient scores reveals an anomaly, “Patient 14”,
whom despite obtaining a six-week score of 0.65, then went onto
register an eight week score of 0.73 seconds (figure 5). This
score in itself was a mean of all three attempts, two of which
had been particularly encouraging at 0.57 and 0.64 seconds, but
was completely skewed by an extremely slow final attempt of 0.99
seconds.
Figure 5. Mean reaction times and “Patient 14”
The small sample size of only twenty patients is a without
question a limitation to this study. Our local region is mainly
rural, serving a population of 531,600 people8 across
1,376 square miles9. In order to attend for testing,
patients living away from the hospital in remote areas needed to
travel a considerable distance at their own cost, which was a
major barrier. As the study was not funded, we could not offer
to pay for travel expenses. The small sample size has had an
impact not only on our eight-week results, but also the
comparison between right and left hips. One would expect those
patients undergoing a right-sided procedure to have a longer
reaction time, as most people brake using the right foot. With
only five left sided procedures in our cohort, we did indeed
notice this trend, but the data was not statistically
significant. However, given that the majority of our data is
based on right-sided results, it could be argued that it is
representative of a worst-case scenario.
From the literature there are few comparable studies. In the
paper by MacDonald and Owen6, twenty-two
patients were assessed, nine left THA’s, twelve rights and one
bilateral procedure, in addition to fifteen normal subjects.
Conceptually the study was similar in the use of a driving
simulator, but with a younger cohort of patients (mean age 58
years) and lower braking force threshold of 100 Nm (compared to
150 Nm). They too found a statistically significant improvement
with time across all periods, but did not examine the time
intervals. Their recommendation of week eight was based heavily
around the 0.7 second average reaction time in the
Highway Code. In the paper by Sandy Ganz et al7,
a sponsored American study comprising ninety patients,
fifty-five of which were tested at one year. Patients were
tested pre-operatively, at 1 week, 4-6 weeks, 26 weeks and at 52
weeks. A statistically significant result was found between the
pre-operative mean, and each time interval. At six weeks the
mean driving reaction time was found to be 0.06 seconds faster
than the pre-op score, comparable to the 0.056 second
improvement in our study. Interestingly, Ganz found a
significant improvement between week six and one year as one may
expect, but not between twenty-six weeks and one year,
suggesting reaction times are better than pre-op by week six and
continue to improve up until a defined point in postoperative
recovery and return to normal function.
Conclusions:
Brake reaction times following primary uncomplicated total hip
arthroplasty improve with time. Our data would suggest this
occurs by week six. Therefore with such patient’s in mind, it
would be reasonable to permit driving from six weeks onwards.
This is supported by one other major study. We recommend
surgeons should fully assess that the patient is making a
satisfactory recovery and document their advice. Patients in the
UK should be made aware of the DVLA’s guidance (5) on driving
following surgery; “that it is the responsibility of the driver
to ensure that he/she is in control of the vehicle” and check
with their insurance provider first.
Reference :
-
Cooper JM.
Clinical decision making: doctor, when can I drive?
Am J Orthop. 2007 Feb;36(2):78-80.
-
Peak EL, Parvizi J, Ciminiello M, Purtill JJ, Sharkey PF,
Hozack WJ, Rothman RH. The role of patient restrictions in
reducing the prevalence of early dislocation following total
hip arthroplasty. A randomized, prospective study.
J Bone Joint Surg Am. 2005 Feb;87(2):247-53.
-
Spalding TJ, Kiss J, Kyberd P, Turner-Smith A, Simpson AH.
Driver reaction times after total knee replacement.
J Bone Joint Surg Br, Sep 1994; 76-B: 754 -
756.
-
Department of Transport. The Highway Code. London: HMSO, 1978.
-
Department of Transport. At a glance Guide to the current
Medical Standards of Fitness to Drive. Driver Medical Group,
DVLA, Swansea, February 2009.
-
MacDonald W, Owen JW. The effect of total hip replacement on
driving reactions. J Bone Joint Surg
Br. 1988 Mar;70(2):202-5.
-
Ganz SB, Levin AZ, Peterson MG, Ranawat CS. Improvement in
driving reaction time after total hip arthroplasty.
Clin Orthop Relat Res. 2003
Aug;(413):192-200.
-
UK England & Wales Scotland and Northern Ireland 2007. Office
for National Statistics,
http://www.ons.gov.uk .
Accssed 28th August 2009.
-
UK Standard Area Measurements 2007. Office for National
Statistics,
http://www.ons.gov.uk .
Accssed 28th August 2009.
|