|
Abstract:
While pelvic pain in the peripartum period is commonplace,
little is known regarding its relation to symphyseal widening.
The purpose of this study was to evaluate physiologic change in
the widening of the symphysis pubis postpartum, and determine
its relationship to suprapubic pain. Sixty-four women who were
within 48-hours post vaginal delivery were randomly selected. On
postpartum day one or two, participants used a quantitative
scale to assess pubic and back pain. Chart reviews were
conducted to obtain patient, newborn, and labor characteristics.
Ultrasonography was used to measure symphyseal widening.
Outcomes were suprapubic pain correlated to symphyseal widening,
and these two related to other patient, newborn, and labor
characteristics. The results showed that 88% of the women
perceived mild to moderate pubic pain, while 98% had mild to
moderate back pain. Ultrasonagraphy determined that 41 women had
widening greater than 10mm, but mean symphyseal width did not
correlate with back pain (p=0.83), or pubic pain (p=0.87). Pubic
pain increased with increasing patient age (p=0.02). Back pain
increased with precipitous labor, but did not reach significance
(p=0.06). No correlation was found between postpartum pain and
symphyseal widening, suggesting that there are other mechanisms
of peripartum suprapubic pain that must be considered.
J.Orthopaedics 2010;7(1)e8
Keywords:
Pubis symphysis; symphyseal widening; diastasis; postpartum pain
Introduction:
The symphysis pubis is a nonsynovial amphiarthrodial joint that
forms the anterior arch of the pelvis. It is, however, one of
the three pelvic joints that are affected during the peripartum
period due to hormonal influence and mechanical stressors.
The normal physiologic width of the symphysis pubis ranges from
4-6 mm.[1] Relaxation of the symphyseal ligaments during the
peripartum period is a well-described phenomenon, beginning in
the 10th week of gestation and reaching a maximum at or near
term. The average widening during pregnancy ranges from 6 mm to
8 mm, with return to baseline between 4 to 12 weeks
postpartum.[2, 3] It has been hypothesized that relaxin, an
insulin-like hormone, influences cartilage swelling and pelvic
ligament laxity, and thus symphyseal widening; however, most
studies to date have found no association.[4] Post-mortem
studies found that mechanical stressors during labor cause focal
and edematous changes in the ligaments in all women with vaginal
deliveries of a neonate over 2300 grams.[5] Sustained
symphyseal widening greater than 10 mm is considered to be
pathologic, as observations have shown it be associated with
significantly increased maternal morbidity and disability
postpartum.[6]
The incidence of pubic symphysis diastasis is estimated to be 1
in 521 to 1 in 30,000 vaginal deliveries.[7-9] Factors that are
presumed to affect widening include precipitous labor or rapid
descent of the presenting part of the fetus. Other factors, such
as maternal age, parity, pelvimetry or fetal weight have not
been shown to correlate with symphyseal diastasis.[10]
While pelvic pain in the peripartum period is commonplace,
little is known regarding the relationship between symphyseal
widening and the development of this pain. We conducted a pilot
study to evaluate physiologic changes in the widening of the
symphysis pubis postpartum utilizing ultrasonagraphy, and
correlated these findings with patients’ symptoms defined as
suprapubic pain, unrelated to other causes (e.g. uterine
cramps).
Materials
and Methods:
The design of the study involved prospective analysis of
postpartum women in a single urban hospital between October 2006
and May 2007. Patients who were within 48-hours post vaginal
delivery were randomly selected and asked to participate in the
study. Written and Institutional Review Board (IRB) approved
consent was obtained from all subjects who met inclusion
criteria and agreed to use of their personal data for research
purposes.
Subjects
Sixty-five women were asked to participate in the
study. Cesarean sections were excluded for this preliminary
study. Sixty-four women (mean age 28.5 years, age range 17-43)
completed the study.
Pain Evaluation
During the patient's initial enrollment on postpartum day
one or two, participants completed a questionnaire using a
quantitative scale to assess pubic and back pain postpartum. The
pain scale quantified pain on a scale from zero to 10, with mild
pain in the 0-3 range, moderate pain in the 4-7 range, and
severe pain in the 8-10 range. A concurrent chart review was
also conducted on all patients to obtain data on patient and
newborn characteristics, as well as on labor. Data obtained from
the questionnaire and chart review were used to evaluate pubic
and back pain in relation to: symphyseal widening and mobility,
parity, length of gestation, age of patient, length of stage two
of labor, mode of delivery, neonate birth weight and height,
degree of perineal tears, blood loss, and type of the female
pelvis (clinically assessed as gynecoid, anthropoid, android, or
pletipoid). In this study, precipitous labor was defined as
labor less than one hour.
Ultrasound Imaging
Abdominal ultrasonography was used to measure symphyseal
widening in supine position with the knees and hips extended,
and the knees and hips flexed (Figure 1) on postpartum day one
or two. Images were evaluated by a trained ultrasonographer who
took two separate measurements of symphyseal widening at the
superior aspect of the bony arch in both positions (Figure 2).
The averages of the two measurements in each position were used
for statistical analysis. Measurements of symphyseal mobility
were calculated by subtracting the difference of the average
extended value from the average flexed value.
Figure 1: Ultrasonography was used to measure symphyseal
width in supine position with the knees and hips extended, and
the knees and hips flexed.
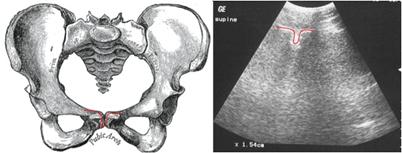
Figure 2:
Ultrasound images (right) were evaluated by a trained
ultrasonographer who took two separate measurements of
symphyseal widening at the superior aspect of the bony arch, as
represented in the schematic drawing of pelvic anatomy (left).
Statistical Analysis
Spearman’s correlation coefficient was used to assess the
association between symphyseal width and pubic and back pain, as
well as all three of these and newborn height and weight. In
addition, Spearman’s correlation coefficients were used to
assess the associations between pubic and back pain and maternal
characteristics, such as age, and labor characteristics,
including parity, estimated blood loss, and degree of perineal
tears. Differences in pubic and back pain across ethnicity were
assessed using one-way analysis of variance (one-way ANOVA)
tests with Bonferroni-adjusted multiple comparisons. Student’s
t-tests were used for two-way comparisons of pain and symphyseal
widening across newborn gender, induction, and rupture of
membranes.
Results :
There were a total of 64 women, with a mean age of 28.5 years,
and age range from 17 to 43 years. The majority of the patients
were Hispanic (31/64). The women had a mean height of 63 inches,
and a mean weight of 159 pounds. Pregnancy status was para 1 in
26 patients, para 2 in 21 patients, para 3 in 12 patients, and
para 4 in 5 patients. The mean parity for the women studied was
1.95. All patients underwent normal spontaneous vaginal
deliveries (NSVD), with a mean estimated blood loss during labor
of 308 milliliters. Sixteen women had induction with oxytocin.
Thirty-two women had artificial rupture of membranes, whereas 30
had spontaneous rupture of membranes. The mean length of stage
two of labor was 43 minutes. Fifty of the women gave birth in
the Semi-Fowler position, three in the lateral, one in
knee-chest, and 10 in lithotomy. Thirty-nine women sustained a
tear, consisting of 11 vaginal or labial, 13 first-degree
perineal, and 15 second-degree perineal. Thirty-one of the
newborn babies were female, and 33 were male. The mean weight
for the newborns was 3182 grams, and the mean height was 43 cm.
Table 1 summarizes the clinical characteristics of these
patients.
The mean symphyseal widening measured was 12 mm, and the mean
change in symphyseal mobility was 5 mm. Sixty-four percent
(41/64) of patients had widening greater than 10 mm. Only one
patient was found to have symphyseal widening greater than 25
mm. This patient, a 29-year old para 5 female who otherwise had
average clinical characteristics, underwent NSVD and perceived
moderate pubic pain and severe back pain. She was the only
subject in our study who perceived severe back pain.
Eighty-eight percent of the women (56/64) perceived mild to
moderate pubic pain, while 98 percent (63/64) had mild to
moderate back pain. Severe pain was a more common complaint
among women with pubic pain (8/64) versus those with back pain
alone (1/64). The mean symphyseal widening did not correlate to
either lower back pain (p=0.83), or pubic pain (p=0.87). Pubic
pain increased with increasing patient age (p=0.02). There was
no significant difference in either pubic or lower back pain
between race groups.
There was no correlation between parity and pain. There was also
no significant relationship between symphyseal widening and
parity. Position and rupture of membranes did not significantly
affect the change in symphyseal widening or increased severity
of pain. Back pain increased with precipitous labor, but did not
reach significance (p=0.06), and pubic pain did not (p=0.72)
either. The size and weight of the newborn was not found to
correlate to either the change in symphyseal width or increased
severity of pain. Two of the deliveries were complicated by
shoulder dystocia, but this was too few to assess for
statistical significance. The measurements of the symphyseal
widening of the two women with this complication were 14 mm and
20 mm.
|
Patient and Newborn Characteristics |
Results |
|
Mean age of Mother (range) |
28.5 years (17-43) |
|
Mean Height of Mother (n=34) |
63 in |
|
Mean Weight of Mother (n=36) |
159 lbs |
|
Race Distribution |
20 Black/31 Hispanic/2 White/11 Other |
|
Mean Length of Gestation |
274.4 days |
|
Mean Parity |
1.95 |
|
Mean symphyseal Width |
12 mm |
|
Mean change in symphyseal width (mobility) |
5 mm |
|
Newborn Gender |
31 Female/33 Male |
|
Mean Newborn Weight |
3182 g |
|
Mean Newborn Height |
43 cm |
|
Mean Length of Stage II of Labor |
43 min |
|
Mean Blood Loss |
308 ml |
Table 1:
Summary of the demographic
and clinical characteristics of subjects.
|
Perceived Pain |
Results |
|
Location |
Mild (%) |
Moderate (%) |
Severe (%) |
|
Pubic symphysis only |
44 (69%) |
12 (19%) |
8 (12%) |
|
Pubic symphysis and back |
9 (14%) |
11 (17%) |
1 (2%) |
|
Back only |
47 (73%) |
16 (25%) |
1 (2%) |
Table 2:
Location of perceived pain is shown according to quantitative
rating by subjects during encounters.
Discussion :
In this study we found the majority of postpartum women to have
experienced a “pathologic” symphyseal separation. We found no
correlation, however, between perceived postpartum pain and
symphyseal widening. In pregnancy, pelvic ligament relaxation
and increased joint mobility is observed.[11] Peripartum pubic
and lower back pain is experienced in approximately 50 percent
of women during pregnancy, and there is some evidence that pain
is associated with symphyseal widening during pregnancy.[12-15]
However, the correlation
between antepartum symphyseal widening and pain is debatable, as
Bjorklund et al (2000) found that while widening was strongly
associated with pain, there was no evidence that the degree of
symphyseal widening determined the severity of pubic pain in
pregnancy or postpartum. This finding suggests that there are
other mechanisms of peripartum pain that must be considered.[12]
The literature suggests that symphyseal widening during
pregnancy is due to both hormonal influence and mechanical
stressors. It is possible that postpartum pain is a continuum of
antepartum pain and mediated by these same factors; however, the
variability of postpartum pain in location and severity suggests
that there may be two distinct etiologies. The etiology of mild
to moderate postpartum pain that ceases within days after
delivery may be explained by the relaxation of the symphysis
pubis during delivery. This physiologic widening is consistent
with our study finding of 88 percent of women who perceived mild
to moderate pubic pain (Table 2). A retrospective study that
examined women with symptomatic symphyseal separation found that
55 percent of women described pubic pain as their only symptom,
and only two women did not suffer from pain in this area.[16] A
meta-analysis of case reports found that the predominating
symptom of separation of the symphysis pubis is a constant, dull
pain located directly over the symphysis.[9]
According to Larsen et al (1999), approximately four percent of
women experience severe pain localized to the pubis and low back
for several months postpartum.[17] Though not all of these
women sustained a symphyseal diastasis, the etiology of this
more intense and prolonged pain is believed to be due to pelvic
ring instability at both the pubic symphysis, and if severe
enough, also at the sacroiliac joints.[11] Studies have reported
that symphyseal diastasis exceeding 40 mm disrupts the
sacroiliac ligaments.[18, 19] This suggests that patients who
experience mild to moderate postpartum pain suffer from
physiologic pelvic dysfunction, while those with severe pain
likely suffer symphyseal diastasis due to biomechanical
disruption of the muscles and ligaments within the pelvic ring
during delivery.[11, 20, 21] In this study, we
define symphyseal diastasis as disruption of the pelvic ring
with more than 25 mm of symphysis pubis separation.[22]
Due to similarity in presentation and symptoms, and a lack of
objective measures of ligament relaxation or pelvic instability,
there is confusion in both the terminology and criteria used to
describe and diagnose symphysis pubis dysfunction, symphysis
pubis diastasis, and peripartum back and pubic pain.[11, 20, 23]
As a result,
the diagnosis is often
based on the patient’s information about
severity and location of
pain.
In this study, we considered pubic and lower back pain as
separate entities with similar etiologies along a spectrum of
pelvic ligament laxity. Though we did not find any significant
difference in the frequency or severity of pubic pain versus
back pain in the postpartum period, it is hypothesized that
pubic pain would not only be a more common complaint, but also
less pronounced than back pain due to the more extreme etiology
of the latter.
The literature is inconclusive on the relationship between a
precipitous second stage of labor and postpartum pain.[24]
While some have found no correlation, a series of case
reports suggest that rupture of the symphysis pubis in
spontaneous labor is due to marked rapidity of labor.[9] In our
study we found a trend of low back pain increasing with
precipitous labor, though it was not statistically significant.
A plausible explanation for this observation is that the
ligaments may undergo plastic rather than elastic deformation,
which may contribute to a higher rate of dysfunction or
diastasis, not only at the symphysis pubis, but also at the
sacroiliac joint.
The literature is inconsistent with regards to peripartum pain
and age of the mother. Some authors found that younger women
were more likely to have pain postpartum, while others reported
no effect.[14] Our findings suggest that pain increased with
maternal age. One author with similar findings suggested that
this result may be related to the women in their population
having a higher age at their first pregnancy.[25]
Another similar observation was reported for back pain
experienced during pregnancy, but the author was unable to
separate the effects of age on pain from those of parity.[26]
We found that parity was not
correlated to back pain or pelvic pain, but did not examine
whether there were any confounding effects caused by maternal
age. Wu et al suggest that the real pattern of association
between pain is a “U” shape – there is high risk for very young
women whose bodies are not yet ready for pregnancy, then risk
decreases until women get much older, or undergo more
pregnancies.[23] The literature is not conclusive as to whether
postpartum pain increases with the number of pregnancies;
however, it has been shown that pain in the back and pubis after
previous pregnancies increases the risk for peripartum pain in
subsequent pregnancies.[27] It is likely that pain
may be due to the aging process and ligamentous laxity
associated with increasing age, rather than parity.[28]
It has been suggested that postpartum pain may occur as a result
of traumatic delivery, such as in shoulder dystocia.[11]
There is some evidence that shoulder dystocia is associated with
symphyseal separation. In the only case of its type to be
reported, shoulder dystocia was resolved through spontaneous
separation of the pubis symphysis.[29] Other reports have found
separation of the pubis symphysis following the McRobert’s
maneuver.[30, 31] In our study, we had two patients with
complications of shoulder dystocia during delivery, both of
which had widening greater than 1 cm. A larger sample size would
enable us to consider the relationship between the McRobert’s
maneuver, symphyseal widening, and related pain.
Ultrasound is a consistent, cost-effective and harmless means of
measurement. Although discrepancies exist regarding ultrasound
technology for measurement of symphyseal widening, we considered
the upper margin of the symphysis pubis joint with the patient
supine as the true symphyseal width. The measurements in this
study are consistent with other authors who have found
ultrasonography to be a reliable and reproducible method to
measure symphyseal width.[27].
The limitation of this study is its small sample size. A post
hoc power analysis was performed. This showed that if we
increased the number of patients 50-fold (3,064) we would
increase our power to 80 percent. In addition, the relationship
between parity and pain in relation to maternal age may be
further elucidated by gaining a greater sample of women.
Pain is subjective and patient-to-patient variations may have a
psychological component as well as a physical component which
was not measured.
Future directions of this study include consideration of
antepartum pain to determine whether postpartum pain is residual
antepartum pain or due to dysfunction and rupture of ligaments.
Postpartum pubic pain and back pain are similar in etiology, yet
unique in frequency, location, and severity. The diagnosis is
most commonly made based on clinical presentation, although the
literature on ultrasonography to aid in the diagnosis continues
to grow.
In conclusion, we believe that although a diagnosis of
symphyseal dysfunction or diastasis does not change the
management during labor, a better understanding of the etiology
of postpartum pain will help in the management of patients with
this condition as well as potentially aid patients who sustain
this condition with subsequent pregnancies.
Reference :
-
Wurdinger, S., et al., MRI of the pelvic ring joints
postpartum: normal and pathological findings. J Magn Reson
Imaging, 2002. 15(3): p. 324-9.
-
Heyman, J., Lundquist A., The symphysis pubis in pregnancy
and parturition. Acta Obstet Gynecol Scand, 1932. 12: p.
35.
-
Alicioglu, B., et al., Symphysis pubis distance in adults:
a retrospective computed tomography study. Surg Radiol
Anat, 2008. 30(2): p. 153-7.
-
Dietrichs, E. and O. Kogstad, "Pelvic girdle
relaxation"--suggested new nomenclature. Scand J Rheumatol
Suppl, 1991. 88: p. 3.
-
Scriven, M.W., D.A. Jones, and L. McKnight, The importance
of pubic pain following childbirth: a clinical and
ultrasonographic study of diastasis of the pubic symphysis.
J R Soc Med, 1995. 88(1): p. 28-30.
-
Lindsey, R.W., et al., Separation of the symphysis pubis in
association with childbearing. A case report. J Bone Joint
Surg Am, 1988. 70(2): p. 289-92.
-
Heckman, J.D. and R. Sassard, Musculoskeletal
considerations in pregnancy. J Bone Joint Surg Am, 1994.
76(11): p. 1720-30.
-
Luger, E.J., R. Arbel, and S. Dekel, Traumatic separation
of the symphysis pubis during pregnancy: a case report. J
Trauma, 1995. 38(2): p. 255-6.
-
Reis RA, B.J., Arens RA et al., Traumatic separation of the
symphysis pubis during spontaneous labor: With a clinical and
X-ray study of the normal symphysis pubis during pregnancy and
the puerperium. . Surg Gynecol Obstet, 1932. 55: p. 18.
-
Snow, R.E. and A.G. Neubert, Peripartum pubic symphysis
separation: a case series and review of the literature.
Obstet Gynecol Surv, 1997. 52(7): p. 438-43.
-
Leadbetter, R.E., D. Mawer, and S.W. Lindow, Symphysis
pubis dysfunction: a review of the literature. J Matern
Fetal Neonatal Med, 2004. 16(6): p. 349-54.
-
Bjorklund, K., et al., Symphyseal distention in relation to
serum relaxin levels and pelvic pain in pregnancy. Acta
Obstet Gynecol Scand, 2000. 79(4): p. 269-75.
-
Fast, A., et al., Low-back pain in pregnancy. Spine (Phila
Pa 1976), 1987. 12(4): p. 368-71.
-
Ostgaard, H.C. and G.B. Andersson, Postpartum low-back
pain. Spine (Phila Pa 1976), 1992. 17(1): p. 53-5.
-
Ostgaard, H.C., G.B. Andersson, and K. Karlsson, Prevalence
of back pain in pregnancy. Spine (Phila Pa 1976), 1991.
16(5): p. 549-52.
-
Owens, K., A. Pearson, and G. Mason, Symphysis pubis
dysfunction--a cause of significant obstetric morbidity.
Eur J Obstet Gynecol Reprod Biol, 2002. 105(2): p. 143-6.
-
Larsen, E.C., et al., Symptom-giving pelvic girdle
relaxation in pregnancy. I: Prevalence and risk factors.
Acta Obstet Gynecol Scand, 1999. 78(2): p. 105-10.
-
Callahan, J.T., Separation of the symphysis pubis. Am J
Obstet Gynecol, 1953. 66(2): p. 281-93.
-
Hagen, R., Pelvic girdle relaxation from an orthopaedic
point of view. Acta Orthop Scand, 1974. 45(4): p. 550-63.
-
Hansen, A., et al., Postpartum pelvic pain--the "pelvic
joint syndrome": a follow-up study with special reference to
diagnostic methods. Acta Obstet Gynecol Scand, 2005.
84(2): p. 170-6.
-
Owens K., P.A., Mason G., Pubic Symphysis Separation.
Fetal and Maternal Medicine Review, 2002. 13: p. 13.
-
Kellman, J.F., Browner B.D., ed. In Skeletal Trauma.
Fractures, Dislocations, and Ligamentous Injuries.
Fractures of the Pelvic Ring, ed. J.J.B. Browner B.D., Levine
A, Trafton PG. Vol. 1. 1992, W.B. Saunders: Philidelphia. pp.
859-863.
-
Wu, W.H., et al., Pregnancy-related pelvic girdle pain
(PPP), I: Terminology, clinical presentation, and prevalence.
Eur Spine J, 2004. 13(7): p. 575-89.
-
Breen, T.W., et al., Factors associated with back pain
after childbirth. Anesthesiology, 1994. 81(1): p. 29-34.
-
Mens, J.M., et al., Understanding peripartum pelvic pain.
Implications of a patient survey. Spine (Phila Pa 1976),
1996. 21(11): p. 1363-9; discussion 1369-70.
-
Mantle, M.J., R.M. Greenwood, and H.L. Currey, Backache in
pregnancy. Rheumatol Rehabil, 1977. 16(2): p. 95-101.
-
Bjorklund, K., M.L. Nordstrom, and S. Bergstrom,
Sonographic assessment of symphyseal joint distention during
pregnancy and post partum with special reference to pelvic
pain. Acta Obstet Gynecol Scand, 1999. 78(2): p. 125-30.
-
Conn, M., ed. Handbook of Models for Human Aging. A
Model for Understanding the Pathomechanics of Osteoarthritis
in Aging, ed. M.A. Andriacchi TP. 2006, Elsevier: Amsterdam.
pp. 351-366.
-
Niederhauser, A., et al., Resolution of infant shoulder
dystocia with maternal spontaneous symphyseal separation: a
case report. J Reprod Med, 2008. 53(1): p. 62-4.
-
Culligan, P., S. Hill, and M. Heit, Rupture of the
symphysis pubis during vaginal delivery followed by two
subsequent uneventful pregnancies. Obstet Gynecol, 2002.
100(5 Pt 2): p. 1114-7.
-
Heath, T. and R.B. Gherman, Symphyseal separation,
sacroiliac joint dislocation and transient lateral femoral
cutaneous neuropathy associated with McRoberts' maneuver. A
case report. J Reprod Med, 1999. 44(10): p. 902-4.
|