|
Abstract:
Background
The radiographic assessment of hip placement followed closed
reduction is limited when plaster-of-Paris casts are used. The
aim of this study was to systematically determine if closed hip
reductions treated by fiberglass spica casts are more amenable
to evaluation by plain x-ray.
Methods
The study group consisted of 21 children (age 1.5-5 months)
treated for congenital dislocation of the hip (total, 23 hips)
at a single tertiary pediatric medical center from 2006 to 2008.
Hips were immobilized in a full spica cast made of semi-rigid
and rigid fiberglass, applied by at least two experienced
surgeons. Hip position was verified under fluoroscopy while the
child was still under general anesthesia. Follow-up was
performed with plain pelvic radiography and computed tomography.
At 6 weeks, the cast was changed under general anesthesia and
the reduction verified fluoroscopically. Radiograph quality,
treatment outcome, and cast-related complications were compared
with findings in 21 children treated several years earlier
(before introduction of the fiberglass spica cast at our center)
by the same team for the same indications with the identical
protocol, but with a plaster-of-Paris spica cast.
Results
All bony landmarks of hip reduction in the study group were
easily identified on the x-rays at all time points. Computed
tomography was noncontributory. In one case, the reduced hip was
found to be dislocated under fluoroscopy immediately at the end
of the procedure, which allowed for instant re-reduction.
Retrospective evaluation of the matched cohort revealed that 2
redislocations were initially missed because of the poor quality
of the intraoperative fluoroscopy and x-ray films.
Conclusion
Using fiberglass spica casts after closed reduction in children
with developmental dislocation of the hip, clinicians can
properly evaluate hip placement on plain x-rays, both after
application (for immediate re-reduction, if necessary) and
during follow-up. Furthermore, children are spared unnecessary
ionizing radiation from computed tomography scanning.
J.Orthopaedics 2010;7(1)e6
Keywords:
Spica cast; Fiberglass; Hip reduction; CDH.
Introduction:
The plain radiographic assessment of concentric reduction in
developmental dislocations of the hip is based on several
well-established criteria.1,2 However, in children
treated with a plaster-of-Paris spica cast after closed
reduction of a dislocated hip, the plaster itself limits the
quality of the radiographs, making it difficult for the
clinician to identify the exact position of the femoral head.3-9
To overcome this problem, researchers have suggested cutting a
window in the plaster above the reduced hip9 or the
use of tomography,8 ultrasound,10 computed
tomography (CT),3-7 or magnetic resonance imaging.11-13
Most authors today recommend a plaster cast for hip
immobilization after closed reduction, and little attention has
been addressed to the value of synthetic spica casts in this
setting. Our preliminary experience suggested that when a
synthetic spica cast is used, a clear view of all established
landmarks can be achieved by plain radiography, and the correct
position of the hip can be correctly ascertained.
The aim of this prospective study was to systematically
determine if closed hip reductions treated by fiberglass spica
cast are amenable to evaluation by plain x-ray compared to the
commonly used plaster-of-Paris spica cast.
Patients
and Methods:
This prospective cohort study was conducted between
January 2006 and April 2008 and included 21 consecutive
children with congenital dislocation of the hip (2 bilaterally)
who were scheduled for closed hip reduction at our Pediatric
Orthopedic Unit after failed treatment with a Pavlik harness.
The study protocol was approved by the local medical ethics
committee, and the parents of all children provided written
informed consent.
The procedure consisted of adductor longus tenotomy (open or
percutaneous), hip arthrography, and reduction under
fluoroscopy. A printout of the position of the reduced hip, as
verified by arthrography, was made, and the hip's bony
relations were evaluated as follows: Shenton’s line; position of
the femoral head in the medial lower quadrant produced by the
juncture of Perkin's and Hilgenreiner's lines; and alignment of
the femoral neck axis with the triradiate cartilage. The
children were then immobilized in a full spica cast made of a
mixture of semi-rigid and rigid fiberglass. The cast was applied
by at least two surgeons: One held the child in position over a
spica table, and the other placed the cast. Careful attention
was addressed to mold the cast dorsal to the greater trochanters
in order to prevent redislocation, and also to the padding at
the cast edges.
At the end of the procedure, the child’s hip position was
verified under fluoroscopy while he/she was still under general
anesthesia. The radiographic criteria for hip reduction were
position of the ossified nucleus, if present, at the
inferomedial quadrant created by the intersection of the
Perkin’s and Hilgenreiner’s lines or alignment of the femoral
neck with the triradiate cartilage.
The children were followed in the first and second weeks after
reduction by plain pelvic radiograms and CT scans. All images
were assessed by a pediatric radiologist and 2 pediatric
orthopedic surgeons, and their findings were recorded. At 6
weeks after reduction, the patients underwent a spica cast
change under general anesthesia. During the procedure, the hips
were examined for stability. The reduction was verified on
clinical grounds and by fluoroscopy; arthrography was not
performed. The second cast was removed 6 weeks later at the
outpatient clinic; there was no need for general anesthesia.
End points for the study were quality of the radiographs after
cast placement and cast change, outcome of treatment, and
complications due directly to the spica casts.
The findings in the study group were compared to a group of 21
patients treated at our center by the same team and for the same
indications with the identical protocol, but with a
plaster-of-Paris spica cast. The control patients all presented
from January 2003 to January 2006, before the fiberglass cast
was introduced for use in our department. Their data for the
present study were collected from the medical files.
Results :
The study group included 17 female and 4 male patients aged 1.5
to 5 months (average 3.6 months). In 7, the hip dislocation was
on the right side, and in 12, on the left; the remaining 2
patients had bilateral dislocations (total, 23 hip
dislocations).
The designated bony landmarks of hip alignment (Shenton’s line,
position of the femoral head at the inferomedial quadrant
created by the juncture of Perkin's and Hilgenreiner’s lines,
and alignment of the femoral neck axis with the triradiate
cartilage) were all clearly identified on the radiograph after
cast placement and cast change, 6 weeks later (Fig.1).

Fig. 1:
Pelvic x-ray film 6 weeks after closed reduction of the left hip
in a fiberglass spica cast. Note the clear visualization of
landmarks: neck axis and head position in the lower medial
quadrant.
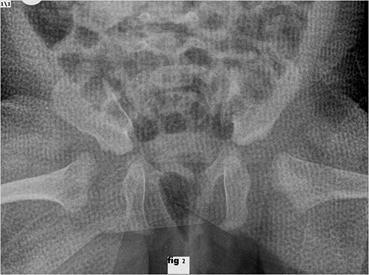
Twenty-two of the 23 hips were stable at all points of
evaluation. In one case, dislocation was demonstrated with the
help of fluoroscopy after completion of cast placement, which
made it possible to perform immediate re-reduction and recasting
while the patient was still under general anesthesia. (Fig.2)
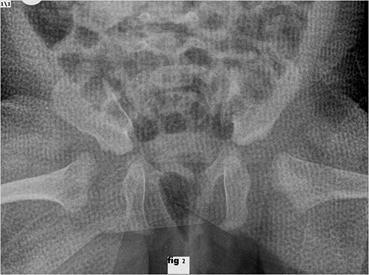
Fig. 2:
Pelvic x-ray after completion of cast placement. Right hip
dislocation can be clearly seen at the end of the attempted
closed reduction. Immediate re-reduction was performed, while
the patient was still under general anesthesia. Note the clear
visualization of the landmarks: neck axis pointing proximally to
the triradiate cartilage.
There were no recurrent dislocations during the follow-up
period.
Complications included an extensive skin rash along the encased
left limb and buttock, noted at cast change in one child and at
cast removal in another. The children were referred to a
dermatologist who diagnosed contact dermatitis and prescribed a
topical steroid cream. All casts remained aesthetically
acceptable, with no breaks and no odor at removal.
The plaster-of-Paris comparison group included 19 female and 2
male patients with a unilateral hip dislocation, 4 on the right
side and 17 on the left. The bony landmarks could not be clearly
seen on the plain x-ray films. Only on CT scan, performed in all
cases to confirm reduction stability, was a
redislocation detected in 2 patients. In both these patients, a
second attempt at conservative treatment failed, and they
underwent open hip reduction.
Discussion :
Our study shows that when hips are immobilized in a synthetic
spica cast after closed reduction, clear radiographs can be
obtained immediately upon completion of the procedure, while the
patient is still under general anesthesia, and during follow-up.
In all of our patients treated with the fiberglass spica cast,
all the radiological landmarks of hip reduction could be clearly
observed. CT scans did not contribute any further information,
and were found to be unnecessary in terms of identifying hip
location. Thanks to the transparency of the fiberglass spica
under fluoroscopy, the single case of closed reduction failure
was detected immediately, while the patient was still under
anesthesia. By contrast, in the comparison group treated by
plaster-of-Paris casts, the plain radiographs were unclear and
failed to show redislocation in 2 cases, which was detected only
on CT scan.
Most authors recommend the use of plaster-of-Paris spica casts
for their ease of application and of molding after closed hip
reduction.2 However, our results show that equally
good results can be achieved with synthetic casts when applied
by orthopedic surgeons well trained in their use. Furthermore,
eliminating the need for CT spares children unnecessary exposure
to radiation. Synthetic spica casts have additional advantages
over plaster-of-Paris casts: They are much lighter, making it
easier for parents to lift and carry their immobilized children,
and more amenable to daily hygienic care. The main
disadvantages of the synthetic spica casts are the need for
clinician training in their application and their higher cost.
Skin rash developed during treatment in 2 of our patients and
resolved upon removal of the cast. We do not know if the rash
was a reaction specifically to the synthetic material. Our
search of the literature yielded one report of a patient in whom
skin maceration caused by the synthetic cast was complicated by
skin infection and septicemia. However, as noted by the authors,
the hygienic care of this child was neglected.14
In conclusion, with the use of a synthetic spica cast after
closed reduction in the treatment of children with developmental
dislocation of the hip, clinicians can properly evaluate hip
placement by plain x-rays, both immediately after application of
the spica cast and during follow-up. When applied by an
experienced physician, the fiberglass cast yields an equally
good outcome to the plaster-of-Paris cast, and children are
spared the unnecessary ionizing radiation of CT. These findings
have important clinical implications given the additional
advantages of fiberglass spica casts in terms of lighter weight
and hygiene, which ease the burden of care.
Reference :
-
Herring JA, editor. Tachdjian’s
pediatric orthopedics. 3rd ed. Philadelphia: WB Saunders;
2002. p. 530-2.
-
Morrissy RT, Weinstein SL, editors.
Lovell and Winter’s pediatric orthopaedics. 6th
ed. Philadelphia: Lippincott Williams & Wilkins; 2006. p.
1011.
-
Toby EB, Koman LA, Bechtold RE,
Nicastro JN. Postoperative computed tomographic evaluation of
congenital hip dislocation. Journal of Pediatric
Orthopedics 1987; 7: 667-70.
-
Smith BG, Kasser JR, Hey LA,
Jaramillo D, Millis MB. Postreduction computed tomography in
developmental dislocation of the hip. Part I: analysis of
measurement reliability. Journal of Pediatric Orthopedics
1997; 17: 626-30.
-
Browning WH, Rosenkrantz H,
Tarquinio T. Computed tomography in congenital hip
dislocation. The role of acetabular anteversion. The
Journal of Bone and Joint Surgery. American volume 1982;
64: 27-31.
-
Mandel DM, Loder RT, Hensinger RN (1998)
The predictive value of
computed tomography in the treatment of developmental
dysplasia of the hip. Journal of Pediatric Orthopedics
1998; 18: 794-8.
-
Stanton RP, Capecci R. Computed
tomography for early evaluation of developmental dysplasia of
the hip. Journal of Pediatric Orthopedics 1992; 12:
727-30.
-
Samuelson KM, Nixon GW, Morrow RE.
Tomography for evaluation of congenital dislocation of the hip
while in a spica cast. The Journal of Bone and Joint
Surgery. American volume 1974; 56: 844-5.
-
Katz K, Yosipovitch Z (1994) Medial
approach open reduction without preliminary traction for
congenital dislocation of the hip. Journal of Pediatric
Orthopedics. British volume 1994; 3: 82-5.
-
van Douveren FQ, Pruijs HE, Sakkers
RJ, Nievelstein RA, Beek FJ. Ultrasound in the management of
the position of the femoral head during treatment in a spica
cast after reduction of hip dislocation in developmental
dysplasia of the hip. The Journal of Bone and Joint
Surgery. British volume 2003; 85: 117-20.
-
Mitchell PD, Chew NS, Goutos I,
Healy JC, Lee JC, Evans S, et al. The value of MRI
undertaken immediately after reduction of the hip as a
predictor of long-term acetabular dysplasia. The Journal of
Bone and Joint Surgery. British volume 2007; 89:
948-52.
-
Westhoff B, Wild A, Seller K,
Krauspe R. Magnetic resonance imaging after reduction for
congenital dislocation of the hip. Archives of Orthopaedic
and Trauma Surgery 2003; 123: 289-92.
-
Wirth T, Haake M, Hahn-Rinn R,
Walthers E. Magnetic resonance tomography in diagnosis and
therapy follow-up of patients with congenital hip dysplasia
and hip dislocation. Zeitschrift für Orthopädie und ihre
Grenzbegiete 1998; 136: 210-4.
-
Kremli M. Septic shock with skin
ulceration and infection after use of a synthetic hip spica
cast for treatment of congenital dislocation of the hip.
Annals of Saudi Medicine 2003; 23: 171-2.
|