|
Abstract:
A prospective,
multi-centre study was devised to investigate the correlation
between the clinical findings of patients presenting with
traumatic hip pain and the presence of occult hip fracture
diagnosed on MRI. 32 patients admitted with a suspected occult
hip fracture had both hips assessed for evidence of resting limb
deformity, point tenderness, hip pain on heel percussion,
pistoning and ability to straight leg raise (SLR). Plain
radiographs and MRI findings were also recorded in each case and
correlated with the findings. 23 out of 32 patients were unable
to SLR on the affected side and 21 of those had a fracture of
the pelvis or proximal femur on MRI. 9 patients could SLR of
which 6 had no fractures and 3 had a fracture of the pelvis or
proximal femur on MRI. The results show that the SLR test is 92%
sensitive and 75% specific for predicting the presence of a
fracture in either the proximal femur or pelvis and is therefore
recommended as a simple, reliable test to expedite the
investigation, diagnosis and further management of occult hip
fractures.
J.Orthopaedics 2009;6(4)e5
Keywords:
Occult hip fracture; straight leg raise; diagnosis hip fracture
Introduction:
Fractures of the femoral
neck are relatively common and usually present in the elderly
population. The risk of hip fracture doubles for each decade
beyond fifty years of age[1] and is an increasing problem as the
population becomes increasingly elderly[2]. The diagnosis is
usually made following clinical examination and the use of plain
film radiographs. Unfortunately minimally impacted or
undisplaced fractures may present with normal or equivocal
radiographs especially in the presence of osteoporosis and
advanced osteoarthritis[1,3,4,5,6].
There is little in the
literature about the clinical findings in patients with occult
hip fractures. What has been clearly established is that delayed
treatment of hip fractures results in increased morbidity,
mortality and hospital stay[7,8,9,10]. Zuckerman showed a
ten-fold increase in mortality when the operation was delayed
for more than 48 hours after admission[6].
The aim of our study was
to record the clinical and radiological findings of patients
admitted with a suspected neck of femur fracture and to
correlate any of the findings with the presence of a fracture on
MRI. If a test is shown to be predictive of hip fractures then
this can be used to expedite those patients with a suspected hip
fracture for further investigation.
Materials
and Methods:
A prospective,
multi-centre study was conducted looking at all patients
admitted with a suspected occult hip fracture that required
further investigation. Patients that were noncompliant with
examination or had gross degenerative changes of the hip on
plain radiographs were excluded. Each patient was assessed for
evidence of suspected occult hip fracture and the ability to
straight leg raise (SLR). All the patients admitted to the study
underwent an MRI scan and the results were correlated with the
clinical findings. The SLR test was found to be the most
reliable and reproducible test and therefore became the focus of
our study.
Results :
32 patients were
admitted to the study (10 male and 22 female, age range 58 – 101
years with a mean of 76 years). Of the 32 patients, 23 were
unable to straight leg raise on the affected side, 9 were able
to do so. Of the 23 patients unable to straight leg raise, 21
had a fracture of the proximal femur and or pelvis on MRI. Of
the group of 9 able to straight leg raise 6 had no fracture on
MRI and 3 had a fracture to the proximal femur or pelvis. All
patients could straight leg raise and had normal MRI of the
contra lateral hip.The fractures identified on the MRI scan
included: 6 Intertrochanteric, 5 Subcapital, 4 Basicervical, 4
Greater trochanteric, 3 Acetabular , 3 Pubic rami and 1 Sacral
fracture.
Under the conditions of this study the straight leg raise test
had a 92% sensitivity and 75% specificity for a fracture of the
proximal femur or pelvis.
|
Diagnosis on MRI |
Number |
|
Subcapital fracture |
5 |
|
Basicervical |
4 |
|
Intertrochanteric |
6 |
|
Greater trochanteric |
4 |
|
Pubic ramus fracture |
3 |
|
Acetabular |
3 |
|
Sacral fracture |
1 |
Discussion :
The straight leg raising test is an accurate and reproducible
test to identify those patients with occult hip fracture who
need further investigation. This could be due to the fact when
actively straight leg raising, the load on the head is estimated
to be the same as during the stance phase of the gait cycle
(three times body weight) as shown by Rydell[11].
It has been clearly shown in the literature that the mortality
and morbidity (thromboembolism, pressure sores, pneumonia) rates
for hip fractures rises quickly with increasing delay between
admission and eventual treatment[1,5]. Zuckerman showed a three
day delay doubled the mortality rate in the first year and noted
a ten fold increase in mortality when the operation was delayed
for more than forty eight hours following admission[6]. A
recent meta-anaylsis of published data found a 41% increase in
thirty day all case mortality and an increase of 32% at one year
in those whose surgery was delayed greater than 48 hours[10].
Early surgery has also been shown to decrease the length of
hospital stay and increase the chances of returning to
independent living[7].
Minimally impacted or undisplaced fractures may present with
normal or equivocal radiographs especially in the presence of
osteoporosis or advanced osteoarthritis[1,5,6]. In these cases
further imaging is required. MRI scanning is now the
investigation of choice[3,4,12] and has been shown to be 100%
sensitive and 100% specific for neck of femur fractures[2]. It
is non-invasive, requires no ionizing radiation and the coronal
images collected are easier to interpret than a CT scan’s axial
images. MRI can also detect subtle changes in bone marrow
associated with a fracture and delineate the anatomic
configuration of the fracture enabling appropriate surgical
planning[4,5,6,8,10,11,13]. Figures 1. & 2. show a neck of
femur fracture diagnosed on MRI scan after a normal plain
radiograph.

Figure 1: Plain AP pelvic radiograph in a patient with
left sided hip pain and inability to SLR.
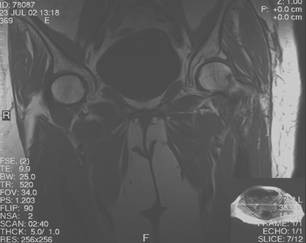
Figure 2: MRI scan of same patient showing a subcapital
fracture of the neck of the left femur.
Cost issues also need to be taken into account when considering
the management of patients with a painful hip. The average
hospital bed costs £350 per day, a bone scan £60, CT £100 and
MRI scan £250. Clearly early diagnosis, investigation and
treatment will both reduce the length of hospital stay therefore
reducing bed costs as well as improving outcome in terms of
mortality, morbidity and a return to independent
living[1,5,7,8,9,10].
The straight leg raising test is therefore recommended as a
simple, quick and reproducible test to help speed up the
diagnosis, investigation and further management of occult
fractures of the hip.
Reference :
-
Ingari JV, Smith DK, Aufdemort TB, Yaszcemski MJ. The anatomic
significance of MRI findings in hip fracture. Clin Orthop
1996; 332: 209-214.
-
Mlinek EJ, Clark KC, Walker CW. Limited magnetic resonance
imaging in the diagnosis of occult hip fractures. AJEM
1996;16(4): 390-392.
-
Chana R, Noorani A, Ashwood N, Chatterji U, Healy J, Baird P.
The Role of MRI in the diagnosis of proximal femoral fractures
in the elderly. Injury 2006; 37(2): 185-189.
-
Hossain M, Barwick C, Sinha AK, Andrew JG. Is Magnetic
resonance imaging (MRI) necessary to exclude occult hip
fracture? Injury 2007; 38(10): 1204-1208.
-
Pandey R, McNally E, Ali A, Bulstrode C. The role of MRI in
the diagnosis of occult hip fractures. Injury 1998;
29(1): 61-63.
-
Zuckerman JD, Skovron ML, Koval KJ et al. Postoperative
complications and mortality rates associated with operative
delay in older patients who have a fracture of the hip. J
Bone Joint Surg 1995; 77A: 1551-1556
-
Al-Ani AN, Samuelsson B, Tidermark J, Norling A, Ekstrom W,
Cederhol T, Hedstrom M. Early operation on patients with a
hip fracture improved the ability to return to independent
living. A prospective study of 850 patients. J Bone Joint
Surg (Am) 2008; 90(7): 1436-1442.
-
Hommel A, Ulander K, Bjorkelund KB, Norrman PO, Wingstrand H,
Thorngren KG. Influence of optimized treatment of people with
hip fracture on time to operation, length of hospital stay,
reoperations and mortality within 1 year. Injury 2008;
39(10): 1164-1174.
-
Novak V, Jotkowitz A, Etzion O, Porath A. Does delay in
surgery after hip fracture lead to worse outcomes? A
multicenter survey. Int J Qual Heath Care 2007; 19(3):
170-176.
-
Shiga T, Wajima Z, Ohe Y. Is operative delay associated with
increased mortality of hip fracture patients? Systematic
review, meta-analysis, and meta-regression. Can J Anaesth
2008; 55(3): 146-154.
-
Rydell N. Biomechanics of the hip joint. Clin Orthop 1973; 92:
6-15.
-
Frihagen F, Nordsletten L, Tariq R, Madsen JE. MRI diagnosis
of occult hip fracture. Acta Orthop 2005; 76(4):
524-530.
-
Rizzo PF, Gould ES, Lyden JP, Asnis SE. Diagnosis of occult
fractures about the hip. J Bone Joint Surg (Am) 1993;
75: 395-401
|