|
Abstract:
Isolated trochlear chondral fractures of the knee are extremely
uncommon, especially in the adolescent population. Little is
known about the specific mechanisms of injury, and symptoms can
often mimic other knee pathologies, making diagnosis difficult.
Because these injuries cannot be diagnosed radiographically and
patient symptoms typically mimic meniscal tears or other knee
pathology, it is possible that these lesions are more prevalent
than previously thought. The purpose of this report is to
describe a case of chondral fracture of the lateral trochlea of
the femur in an adolescent male, to elaborate on the surgical
technique employed, and to provide an analysis for the mechanism
responsible for this injury.
J.Orthopaedics 2009;6(4)e2
Keywords:
Chondral fracture; adolescent; lateral trochlea; knee
Introduction:
Chondral fractures of the trochlea of the knee are uncommon and
rarely reported in the literature. Little is known about the
specific mechanisms that cause these injuries, and symptoms can
often mimic those of other knee pathologies, making diagnosis
difficult. In contrast, both osteochondral fractures as well as
isolated chondral fractures of the weight-bearing portion of the
femoral condyle are more frequently reported in the literature,
and the associated mechanism of injury has been well described.1-9
Only two previous studies10, 11 in the literature
report on isolated chondral injury to the lateral trochlea, and
to our knowledge, there are no reports describing osteochondral
fractures of the trochlea. The report by Oohashi et al.11
suggested that chondral fractures of the trochlea may occur as a
result of shear force of the patella during rapid extension of
the weight-bearing knee from a flexed position; however, this
mechanism has not been verified.
The purpose of this report is to describe a case of chondral
fracture of the lateral trochlea of the femur in an adolescent
male, as well as to analyze the mechanism responsible for this
injury. Prior to writing this manuscript, the authors obtained
the written informed consent from the patient’s guardian
(patient is a minor) for print and electronic publication of the
case report.
Case Report:
A healthy-appearing 13-year-old male reported to the clinic with
a one-month history of carrying some boxes and subsequently
tripping, falling, and landing bluntly on the anterior aspect of
his left knee. The patient stated that he fully recovered from
the injury uneventfully and returned to soccer-related
activities. The patient noted that four days prior to the
initial clinic visit (approximately 3.5 weeks after resuming
soccer activities), he attempted a sharp cutting maneuver and
felt a pop in his knee with immediate pain, swelling, and
inability to bear weight. The patient had no history of
previous surgery on the left knee. The patient obtained an MRI
and reported to the clinic for evaluation.
On physical examination, the patient had a moderate effusion of
his left knee and was exquisitely tender to palpation in the
anterior aspect of his knee. The patient also had focal
tenderness both medially and laterally surrounding the patella,
and had significant patellar apprehension with lateral
mobilization. The patient had active flexion to 90 degrees but
lacked ten degrees of full extension. Passive range-of-motion
testing was limited due to extreme guarding from discomfort.
Testing of the anterior cruciate ligament (ACL), posterior
cruciate ligament (PCL), medial cruciate ligament (MCL), and
lateral cruciate ligament (LCL) were normal, and the patient had
no medial or lateral joint line tenderness. The patient had a
grade I-A Lachman. Pivot shift testing was inconclusive due
pain. Gait examination was also not possible as the patient
could only toe-touch with crutches. The MR images, taken prior
to the clinic visit, revealed what appeared to be a 20 mm
(diameter) cartilaginous loose body originating from the lateral
femoral condyle. The ACL, PCL, MCL, LCL, and both menisci
appeared intact.
Based on the clinical findings and imaging studies, it appeared
that the patient had a patellar dislocation with a cartilage
loose body. Given the patient’s age and desire to return to
athletics, it was recommended that the patient undergo surgical
repair with arthroscopy, mini-arthrotomy, and loose body
fixation using screws.
The patient was brought to surgery 3 days later. General
anesthesia and antibiotics were administered, and a tourniquet
was placed. Examination under anesthesia revealed a stable knee
with a moderate effusion and full range-of-motion. A diagnostic
arthroscopy was then performed utilizing standard superloateral,
inferolateral, and inferomedial portals. Upon entering the
joint, the effusion was evacuated and an intact 35 by 35 mm
osteochondral fragment in the superior pouch of the knee was
revealed (Figure 1). The patella, lateral and medial
femoral condyles, lateral and medial menisci, lateral and medial
tibial plateaus, ACL, and PCL were all normal. Because of the
size, depth, and location of the chondral lesion, we decided to
make a mini-arthrotomy as opposed to attempt an all-arthroscopic
repair.
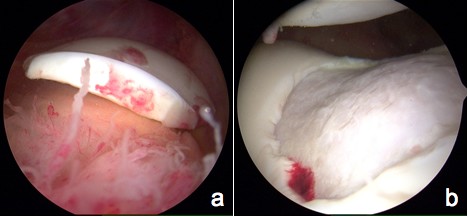
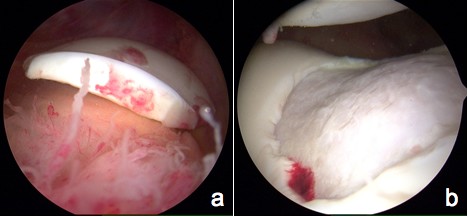
Figure 1a: Arthroscopic image portraying the isolated
chondral fragment
Figure 1b: Arthroscopic image portraying the defect on the
lateral trochlea
A 5 cm mini-arthrotomy incision was made over the anterolateral
patella and a lateral retinacular release was performed to allow
for adequate visualization and to prevent further episodes of
patellar dislocation. The capsule was opened and approximately
2 cm of the distal vastus lateralis was excised. The chondral
fragment was isolated, removed, and placed in moist saline on
the back table. The bed of the lesion, located in both the
convex and concave surface of the lateral trochlea, was curetted
down to the bleeding bone. As the chondral fragment was intact,
orientation and alignment of the fragment back into the defect
was readily achieved. After placement into the defect, the
fragment was secured using three Arthrex chondral darts, two
Arthrex 2.8 mm bioabsorbable screws, and one Arthrex 3.5 mm
cannulated metal screw. Excellent alignment and fixation were
achieved, and the tourniquet was released for a total tourniquet
time of just over 1 hour (Figure 2).
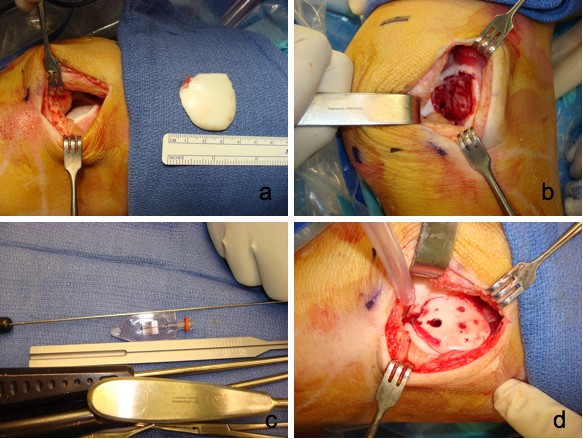
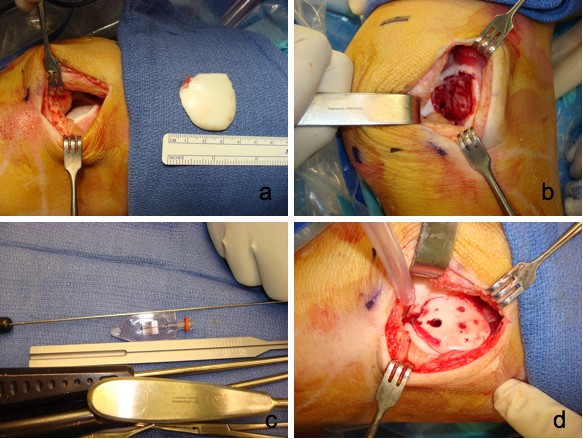
Figure 2a: Intra-operative photograph showing the size of
the removed, intact chondral fragment as well as the fracture
site on the lateral trochlea.
Figure 2b: Intra-operative photograph showing the bed of
the lesion after being curetted down to the bleeding bone
surface.
Figure 2c: Intra-operative photograph showing one of the
Arthrex chondral darts that was used to fix the fragment into
place.
Figure 2d: Intra-operative photograph showing excellent
alignment and fixation of the fragment back into the defect.
The patient was allowed to have full weight-bearing following
surgery, with the utilization of a brace and limited
range-of-motion. Ten days post-operatively, the patient returned
to the clinic and had significantly reduced pain, was not taking
narcotics, and was able to stand and bear weight. Radiographs
demonstrated a single metallic screw in the appropriate location
and not contacting the growth plate (Figure 3). We
opened his brace to 45 degrees to permit increased range of
motion. Approximately 5 weeks post-operatively, the patient had
returned to school, was off of all medication, was walking with
only a mild limp, and was performing light activities without
pain. Physical examination revealed moderate quadriceps
atrophy, consistent with being 5 weeks out of knee surgery. The
patient’s range of motion was 0 to 95 degrees, with a 10 degree
extensor lag and active extension.
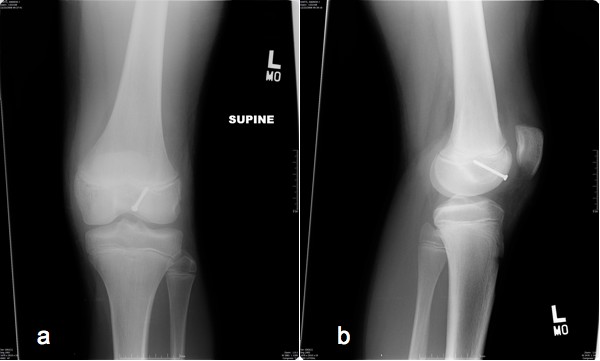
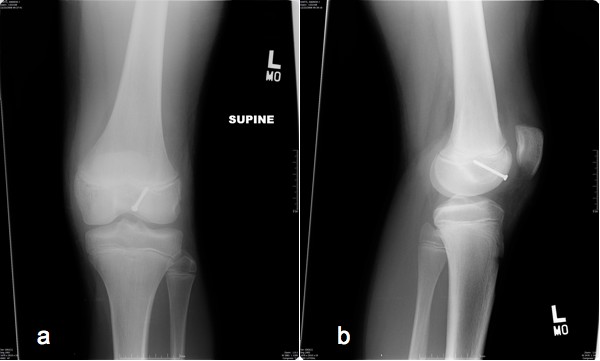
Figure 3: Post-operative radiographs showing a single
metallic screw in the appropriate location and not contacting
the growth plate (a: anterior-posterior view; b: lateral view)
Ten weeks following surgery, the patient returned for follow-up
evaluation and arthroscopic hardware removal of the metallic
screw. The patient was brought to surgery and general
anesthesia was administered. Examination under anesthesia
revealed a completely stable knee with full range of motion.
Arthroscopic incisions were made and a superomedical outflow was
used. The patella appeared completely normal and the large
trochlear defect was united throughout. After identification of
the central metallic screw, it was removed through a
transpatellar tendon technique. The peripheral margins of the
lesion were probed and were completely intact (Figure 4).
No debridement was necessary, and following surgery the patient
was taken to recovery in stable condition.
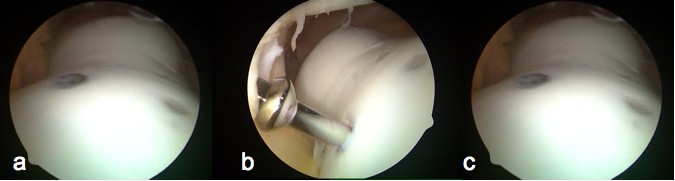
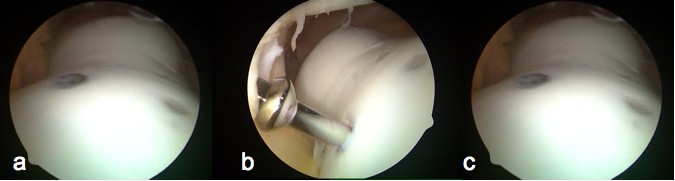
Figure 4a: Arthroscopic image portraying the healed
chondral fragment 10 weeks following fixation
Figure 4b: Arthroscopic image portraying removal of the
central metallic screw through a transpatellar tendon technique
10 weeks following initial fragment fixation
Figure 4c: Arthroscopic image portraying complete healing
of the peripheral margins of the lesion 10 weeks after initial
fragment fixation
Ten days following arthroscopic screw removal, the patient
reported to the clinic with full weight-bearing (no crutches or
assistance) with mild discomfort upon palpation and minor
swelling. Physical examination revealed a small effusion with
moderate tenderness and guarding associated anterior knee
palpation. The patient’s range of motion was 0 to 65 degrees.
At this point, we felt the patient was progressing excellently
and he was recommended to undergo formal physical therapy to
improve range of motion and strengthening. The patient was
asked to avoid use of the leg-extension and leg-press machines
and was asked to avoid all impact activities.
At most recent follow-up, 10 months after open reduction and
internal fixation of the chondral fragment, the patient is
asymptomatic with full active and passive range-of-motion.
Clinically he had no effusion and no patellar apprehension with
lateral mobilization. He had returned back to activity without
restrictions and was able to play soccer, run, squat, jump, and
hop.
Discussion :
Isolated chondral fractures of the lateral trochlea of the knee
are difficult to diagnose and thus are rarely reported in the
literature. Because these injuries cannot be diagnosed
radiographically and patient symptoms typically mimic meniscal
tears or other knee pathology, it is possible that these lesions
are more prevalent than previously thought. While several
reports in the literature describe osteochondral and chondral
fragments of the weight bearing portion of the knee, there are
only 2 reports that describe chondral fragments of the trochlea
and no reports on osteochondral fragments of the trochlea.10,
11 One additional report describes chondral injuries to
the trochlea of the knee, but does not specifically report on
chondral fractures.12
Because there are so few reports of chondral fracture of the
trochlea, it is difficult to determine specific factors that put
someone at risk for this type of injury. It is equally
difficult to determine a common mechanism of injury. While the
study by Huegli et al. does not describe trochlear
chondral fractures, the authors do state that trochlear chondral
lesions typically occur following a sudden movement
incorporating both flexion and rotational components.12
The 15 patients described in this study had an average age of 44
years, and all were older than 17 years old. In a recent report
described by Oohashi et al., an isolated case of chondral
fracture of the lateral trochlea of the femur in a 13-year-old
boy is described.11 In this case, the patient was
playing basketball and experienced a snap in his knee while
extending his knee from approximately 50-60 degrees of flexion.
The MRI and diagnostic arthroscopy revealed the chondral
fragment, however no other significant knee pathology was
noted. The authors described the mechanism of injury to be a
result of “shear force transmitted by the patella to the convex
surface of the trochlea during rapid extension of a weight
bearing knee from a flexed position.” In a report by Dory et
al., an isolated chondral fracture of the intercondylar area
of the knee in a 15-year-old boy subsequent locking of his knee
during a tennis match was described.10 Following
arthrography, this patient was found to have osteochondritis
dissecans (OCD) of the medial femoral condyle. In this report,
the author stated that the fracture had been caused by patellar
impingement of the intercondylar groove; however, it is unknown
if the underlying OCD predisposed this patient to a traumatic
chondral fracture of the trochlea.
While the patient presented in this report is a young male,
similar to the patients presented in both the Oohashi and Dory
reports, we cannot conclude that adolescent males are more prone
to isolated chondral fracture of the trochlea as the overall
reported incidence of this injury is so low. Similarly, while
the patient in our report had no prior diagnosis of OCD, unlike
the patient presented by Dory, it is possible that the initial
traumatic injury sustained by the boy during his fall
approximately 3.5 weeks prior to his soccer injury predisposed
him to chondral fracture of the trochlea. The mechanism of
injury experienced by our patient is also different from those
reported by Oohashi and Dory, further increasing the complexity
of the understanding of this type of injury. Our patient
experienced chondral fracture of the trochlea during an athletic
cutting maneuver while in full weight-bearing, but unlike the
patient from the Oohashi report, this patient did not undergo
rapid extension from a flexed position.
The lateral trochlea in general may be more prone to chondral
fracture due to traumatic contact from the patella as it is
larger and more prominent than the medial trochlea. In
addition, while the association between OCD and trochlear
chondral fracture is unknown, several authors have shown that
OCD of the trochlea is more often lateral.13-15
In conclusion, the patient presented in this report is similar
in age and gender to the patients previously reported to have
isolated chondral fractures of the lateral trochlea of the
knee. Different from the previous reports of causation of this
injury, the mechanism of injury in this case was due to patellar
dislocation during a cutting movement while in full
weight-bearing.
Reference :
-
Gilley JS, Gelman MI, Edson DM, Metcalf RW. Chondral fractures
of the knee. Arthrographic, arthroscopic, and clinical
manifestations. Radiology. Jan 1981;138(1):51-54.
-
Hopkinson WJ, Mitchell WA, Curl WW. Chondral fractures of the
knee. Cause for confusion. Am J Sports Med. Sep-Oct
1985;13(5):309-312.
-
Kennedy JC, Grainger RW, McGraw RW. Osteochondral fractures of
the femoral condyles. J Bone Joint Surg Br. Aug
1966;48(3):436-440.
-
Milgram JW, Rogers LF, Miller JW. Osteochondral fractures:
mechanisms of injury and fate of fragments. AJR Am J
Roentgenol. Apr 1978;130(4):651-658.
-
Terry GC, Flandry F, Van Manen JW, Norwood LA. Isolated
chondral fractures of the knee. Clin Orthop Relat Res.
Sep 1988(234):170-177.
-
Rosenberg NJ. Osteochondral Fractures of the Lateral Femoral
Condyle. J Bone Joint Surg Am. Jul 1964;46:1013-1026.
-
Mashoof AA, Scholl MD, Lahav A, Greis PE, Burks RT.
Osteochondral injury to the mid-lateral weight-bearing portion
of the lateral femoral condyle associated with patella
dislocation. Arthroscopy. Feb 2005;21(2):228-232.
-
Luthje P, Nurmi-Luthje I. Osteochondral fracture of the knee
treated with bioabsorbable implants in two adolescents.
Acta Orthop Belg. Apr 2008;74(2):249-254.
-
Dines JS, Fealy S, Potter HG, Warren RF. Outcomes of
osteochondral lesions of the knee repaired with a
bioabsorbable device. Arthroscopy. Jan
2008;24(1):62-68.
-
Dory MA. Chondral fracture of the anterior intercondylar
groove of the femur. Clin Rheumatol. Jun
1983;2(2):175-177.
-
Oohashi Y. Chondral fracture of the lateral trochlea of the
femur occurring in an adolescent: mechanism of injury. Arch
Orthop Trauma Surg. Nov 2007;127(9):791-794.
-
Huegli RW, Moelleken SM, Stork A, et al. MR imaging of
post-traumatic articular cartilage injuries confined to the
femoral trochlea. Arthroscopic correlation and clinical
significance. Eur J Radiol. Jan 2005;53(1):90-95.
-
Peters TA, McLean ID. Osteochondritis dissecans of the
patellofemoral joint. Am J Sports Med. Jan-Feb
2000;28(1):63-67.
-
Marshall KW, Marshall DL, Busch MT, Williams JP. Osteochondral
lesions of the humeral trochlea in the young athlete.
Skeletal Radiol. May 2009;38(5):479-491.
-
Takahashi Y, Nawata K, Hashiguchi H, Kawaguchi K, Yamasaki D,
Tanaka H. Bilateral osteochondritis dissecans of the lateral
trochlea of the femur: a case report. Arch Orthop Trauma
Surg. May 2008;128(5):469-472.
|