|
Abstract:
Background:
Streptococcus infection was originally thought to be a rare
cause of spondylodiscitis, but recent literature shows that the
incidence is on rise.
Objective:
We describe a previously unreported case of group-C
Streptococcal constellatus spondylodiscitis.
Case Report:
A 72 year old male presented with a 4 week history of worsening
back pain with no neurological deficit. Inflammatory markers
were raised and an MRI scan was suggestive of spondylodiscitis
at the T10/11 level. A CT guided biopsy lead to culture of
Streptococcus constellatus. Treatment was with IV antibiotics
and bed rest with a full recovery achieved.
Conclusion:
The culture of the pathogenic organism following CT guided
biopsy was essential in this case. The spectrum of infection has
yet to be completely described for Streptococcus constellatus.
Early diagnosis and treatment with sensitive antibiotics can
prevent the evolution of drug resistant Streptococcus in the
future.
J.Orthopaedics 2009;6(3)e7
Keywords:
Spondylodiscitis; Streptococcus constellatus; Streptococcal
infection.
Introduction:
We describe a previously unreported case of group-C
Streptococcal constellatus spondylodiscitis. Discitis is mostly
blood borne and has higher risk in the old, debilitated and
intravenous drug addicts. A history of pneumonia, urinary tract
infection, skin infection or immunocompromise is common.
The most common organism is Staphylococcus aureus in 50-75% of
cases. Escherichia coli and Proteus sp. are more common in
patients with urinary tract infections, Pseudomonas aeruginosa
and Klebsiella species are common in intravenous drug addicts1.
Streptococcus infection was originally thought to be a rare
cause, but recent literature shows that the incidence is on rise2,3,4,5.
Case Report
A 72 year old male presented to his general practitioner with a
worsening history of pain in the lower back for 4 weeks. The
pain initially started after gardening, without a history of
trauma or constitutional symptoms. There was no radiation of
pain and no bowel or bladder disturbance.
On examination, there was marked paraspinous muscle spasm and
lower thoracic spine tenderness with restriction of flexion and
extension. There was no sensory or motor deficit and all
reflexes were normal.
Inflammatory markers were raised (white cell count of 10.2× 109/lt,
erythrocyte sedimentation rate of 30mm/hr and a C reactive
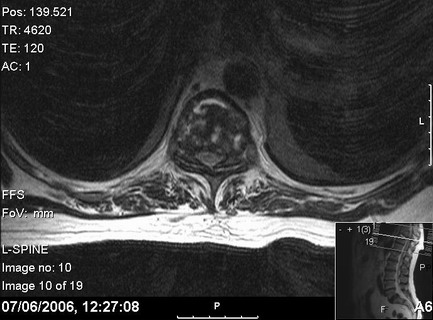
protein of 20). An MRI of the thoraco-lumbar spine showed marked
oedema at T10/T11 with high signal seen in the disc and erosion
of end plates, changes consistent with discitis (Figure 1).
An urgent CT guided biopsy of T10/T11 level grew
Strep.constellatus sensitive to penicillin, erythromycin,
vancomycin and a synergistic infection with Strep. viridans. AFB
staining and culture were negative.
Treatment was with intravenous antibiotics and bed rest.
The back pain resolved in 2 weeks and his inflammatory markers
returned to normal, with a full recovery made.
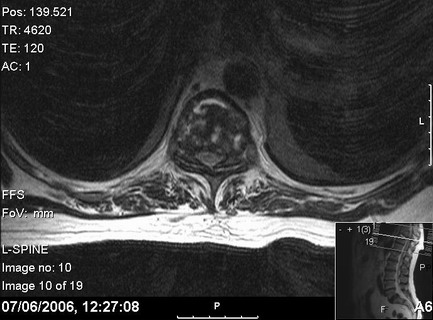
Figure 1.
MRI scan of the T10/11 disc with high signal seen in the disc
and erosion of end plates, changes consistent with discitis.

Discussion :
Strep.constellatus is a gram positive group-C β haemolytic
microaerophyllic streptococcus known to cause upper body
abscesses and respiratory infections, especially in
immunocompromised individuals6. It is a recently
discovered subclass of Strep. milleri with more virulent
characteristics. Strep. constellatus species works
synergistically with other streptococci bacteria. Their ability
to produce capsular material acts a protective shield from the
body’s defences. The complete clinical spectrum of infections
caused by this subspecies has yet to evolve.
A literature search did not find any previous reported cases of
Strep. constellatus spondylodiscitis. As it is microaerophyllic,
the organism can survive well in an oxygen-depleted environment
causing subacute spondylodiscitis. Lack of clinical suspicion
can delay diagnosis. This case highlights the importance of
doing CT guided biopsy in all cases of disctis.
Spectrum of infection has yet to be completely described and
Strep.constellatus should be considered as serious pathogen in
bone infection. Early diagnosis and treatment with sensitive
antibiotics can prevent the evolution of drug resistant
Streptococcus in the future.
Reference :
-
Cottle L, Riordan T. Infectious Spondylodiscitis. J Infect
2008; 56(6):401-12.
-
Jacobs JA, Pieterson HG, Walkenkamp GH, Stobberingh EE,
Soeters PB. Intervertebral infection caused by Streptococcus
milleri- A case report. Clin Orthop Relat Res. 1994;
302:183-8.
-
Meyes E, Flipo RM, Van Bosterhaut B, Mouligneau G, Duquesnoy
B, Delcambre B. Septic Streptococcus milleri spondylodiscitis:
J. Rheumatol.1990 ;17(10): 1421-3.
-
Balsam LB, Shepherd GM, Rouff KL.Streptococcus anginosus
spondylodiscitis: Clin Infect Dis. 1997; 24(1):
93-4.
-
Narváez J, Pérez-Vega C, Castro-Bohorquez FJ, Vilaseca-Momplet
J. Group B streptococcal spondylodiscitis in adults- 2 case
reports: Joint Bone Spine. 2004; 71(4):338-43.
-
Fuentes Olmo J, Ruiz Mariscal M, Uribarrena Amezaga R, Omiste
Sanvicente T. Spontaneous bacterial peritonitis due to
Streptococcus constellatus.
Gastroenterol Hepatol. 2006; 29(9):595-6.
|