|
Abstract:
Background: We evaluated outcomes of radial head
excisions and the subsequent elbow posterolateral rotator
instability concept.
Methods: Among 27 patients who had undergone radial head
excisions due to Mason type 3 radial head fractures between 1996
and 2006, 23 patients who had no ipsilateral upper extremity
pathology and attended routine follow-up visits were included in
the study. The mean duration of follow-up was 65.5 months
(range: 23–115). At last visits, patients were assessed
clinically and radiologically. The Steinberg criteria were used
for clinical outcomes. Patients were also evaluated with respect
to elbow posterolateral rotator instability.
Results: Clinically, 12 patients had good, 7 had fair,
and 4 had poor clinical results, according to the Steinberg
criteria. Eight patients had elbow posterolateral rotator
instability, while 16 patients had radiologically confirmed
elbow joint degeneration. Ulna plus variation was observed in 12
cases.
Conclusion: Although used frequently, total radial head
excision in comminuted radial head fractures has not been found
to give satisfactory results. Furthermore, patients should be
subjected to intraoperative assessment for lateral ulnar
collateral ligament ruptures that may lead to elbow
posterolateral rotator instability.
J.Orthopaedics 2009;6(3)e6
Keywords:
radial
head; fracture; total excision; posterolateral rotatory
instability; lateral ulnar collateral ligament
Introduction:
Radial head fractures are commonly seen injuries in the
community, representing approximately 30% of all fractures
around the elbow joint9. In these fractures, the
Mason classification is the primary categorization system used
in which total radial head excision is considered to be the
accepted method in type-3 comminuted fractures. Despite its
relatively easy application, total excision may cause
posterolateral rotator instability (PLRI) of the elbow;
clinically and radiologically, it may result in positive ulnar
variation, leading to clinical problems at the wrist joint, or
degenerative changes in the elbow3,6-10,14,15. The
anatomical structure responsible for PLRI is the lateral ulnar
collateral ligament (LUCL). In addition to the likelihood that
it may be injured in the trauma itself, this ligament may also
be damaged iatrogenically during surgery. For this reason, such
cases should be subjected to a complete evaluation during radial
head excision with respect to LUCL rupture, and the head of the
radius should be preserved to avoid additional complications.
In this study, 23 patients who had undergone total radial head
excision were assessed clinically and radiologically.
Materials
and Methods:
Twenty-seven patients with Mason type-3 radial head fractures
underwent applied radial head excisions in our clinic between
1996 and 2006. Among the 27 recruited patients undergoing radial
head excision procedure, two were excluded for failing to attend
follow-up visits and two further patients were excluded because
of additional distal radial fractures that could interfere with
the results. The remaining 23 patients (14 men and 9 women) were
followed for 65.5 months on average (range: 23–115). The mean
age at the time of injury was 39.1 years (range: 16–57;
Table).
Reasons for the fractures included falling from a height of less
than 2 m in four patients and above 2 m in two patients;
high-impact trauma, such as traffic accidents, in nine patients;
and minor trauma, such as falling while walking, in eight
patients. Twelve patients had left extremity and 11 patients had
right extremity involvement. One of the traffic accident cases
had an additional knee medial collateral ligament injury, while
another one had a tibia diaphysis fracture. No patient with
minor trauma had any additional pathology. Additionally, none of
the 23 patients had dislocation of either elbow.
All patients included in the study had comminuted fractures; 21
patients underwent radial head excisions and the remaining two
cases were treated conservatively. However, these two patients
subsequently underwent secondary excisions within the first 6
weeks due to severe persistent pain and daily function loss.
Neither patient was assessed with respect to ligamentous injury
intraoperatively, nor did they require soft tissue or annular
ligament repair. A neck sling was used postoperatively. Physical
therapy was initiated as soon as pain became tolerable. No early
postoperative complication was observed.
Patients were followed-up according to clinical condition and
roentgenograms. Evaluations were based on the unaffected elbow.
Elbow flexion and extension angles were measured clinically. Any
restriction in supination and pronation of the forearm, movement
restriction at the wrist joint, differences in elbow diameters,
and pain status and its influence on daily activities were
assessed. Varus and valgus laxities were evaluated.
Additionally, every patient underwent the lateral pivot shift
test5, chair test7, push-up test7,
and tabletop test17, each specific for PLRI. The
results were based on the Steinberg criteria, adapted to
children. Accordingly, cases with a complete range of motion and
no pain were accepted to have good results, those with
restricted movement in any direction by less than 20° were
deemed to have fair results, and those with movement restricted
by more than 20° and pain even during rest were recorded as
having poor results13.
Radiologically, AP and lateral X-ray views were taken, covering
both the unaffected side and wrist joints. Via these plain
X-rays, degenerative signs, such as sclerosis, joint narrowing,
subchondral cyst, osteophyte, heterotopic ossification in the
elbow joint, and positive ulnar variation at the wrist joint,
were assessed.
Results :
Clinical evaluation
Of the 23 patients, 12 had no pain while carrying out daily
activities, while another 7 described slight pain, generally
provoked by lifting objects. Four patients had pain even at
rest, two of whom were housewives who reported loss of function
during their household chores. Of the remaining two subjects,
one was a bakery worker who had to change his job, and the other
was a retired person with a largely sedentary lifestyle. These
four patients were offered radial head arthroplasty procedures,
but none of them chose to undergo this intervention. One of the
patients had fallen from a height above 2 m and underwent a
subsequent primary excision. Two of them had been involved in
traffic accidents and the last case was a minor trauma patient
who had undergone secondary excision.
When assessing elbow and wrist joint ranges of motion, only
seven patients had no difference in terms of elbow extension
restriction compared to the unaffected side. One patient was
observed to have extension restriction by 40°, another by 30°,
two patients by 20°, and 12 by 10°. Moreover, patients with 40°
or 30° extension loss also had further flexion losses by 20°.
Other patients had no marked flexion loss (Fig. 1). In terms of
rotation movements of the forearm, 12 patients had supination
restricted by 10°. Five patients had 10° extensions and two
patients had 10° flexion impairment at wrist joint examination.
Fifteen of the group showed valgus laxity at the elbow joint.
When performing the examination for valgus laxity, all 15 of
these patients had complaints.

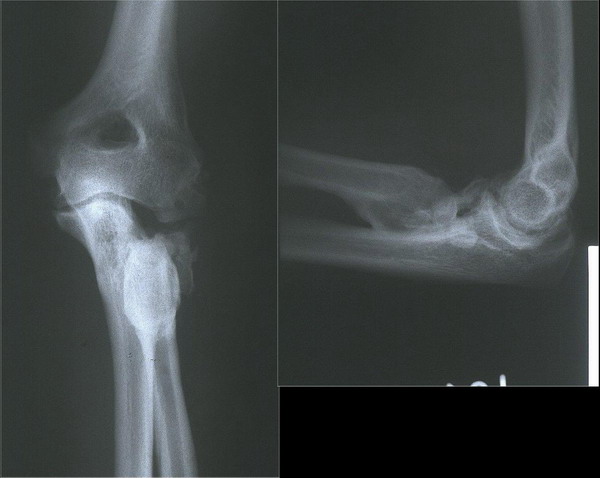
Figure 1: Lateral
view of a comminuted radial head fracture.
At final visits, 11 patients had no circumferential difference
between the two elbows. Ten patients had a 1-cm-wider elbow
compared to the unaffected side, and the remaining two patients
had a 2‑cm-wider elbow compared to the unaffected side, both of
whom underwent secondary excisions.
To establish the PLRI diagnosis clinically, patients underwent
the chair test, push-up test, tabletop test, and lateral pivot
shift test (see Discussion). Of the 23 patients, eight (34.7%)
had groove signs secondary to radial dislocation at the elbow
joint. Furthermore, they were observed to express apprehension
when conducting these tests, all of which were performed by the
same physician. As the lateral pivot shift test was not
performed under general anesthesia, patients did exhibit
over-resistance, and consequently, the test could not be
performed. We routinely perform these tests, which are important
for PLRI diagnosis, at follow-up visits of patients after total
radial head excision.
Clinical outcomes were assessed according to the Steinberg
criteria, revealing good results in 12 patients (52%), fair
results in seven (30%), and poor results in four (18%). The 12
patients with good results had all suffered low-impact traumatic
injury, such as simple falling or falling from a height below 1
m, and underwent primary excision, while those with fair or poor
outcomes were observed to have had an increased severity of
trauma (Table).
Radiological evaluation
At radiological evaluation, the excised site was observed to
possess more degenerative changes compared to the unaffected
elbow. Of the 23 patients, 16 had radiological degenerative
changes. Sclerosis was the most frequently observed finding (all
16 cases), followed by elbow joint narrowing (approx. 1 mm) in
10 patients, formation of articular heterotopic ossification in
five patients (Fig. 2), and subchondral cyst formation in two
patients. All patients developing heterotopic ossification had
restricted movement at the elbow joint.
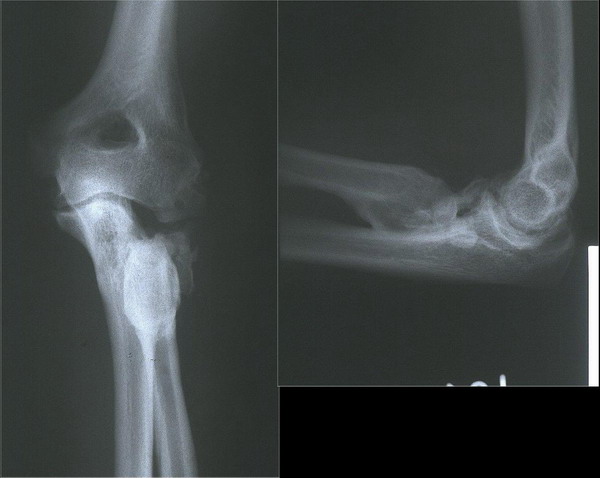
Figure 2: Postoperative second-year plane X-rays of the
same patient. The presence of severe heterotopic ossification is
remarkable.
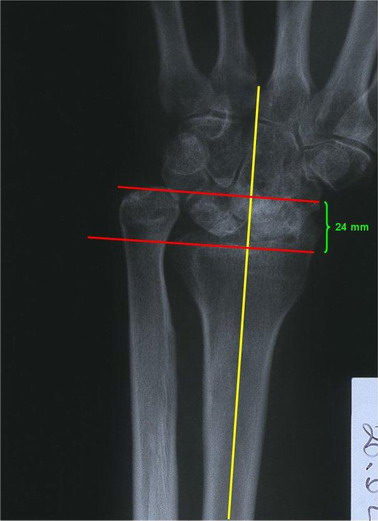
Ulna plus variation (positive ulnar variance) was demonstrated
by comparative wrist roentgenograms. While 11 of 23 patients had
no ulna plus deformity, the remaining 12 patients exhibited 2–24
mm (4.52 mm on average) positive ulnar variance. One patient was
detected to have a 15-mm and another to have a 24-mm ulna plus
deformity (Fig. 3); a severe radial deviation deformity was also
observed at the wrist joint, resulting in loss of function and
pain, which led to an avoidance of daily activities (Table).
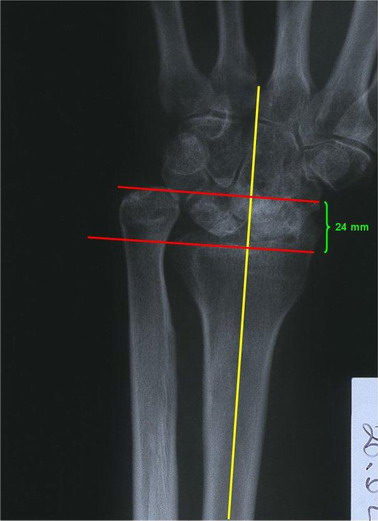
Figure 3: Wrist radiographs of a patient with a 24-mm
ulnar plus variant. Remarkable osteoarthrosis is present.
Discussion :
Fractures of the radial head are frequently seen injuries,
comprising 1.5–4.0% of all fractures. Representing about 30% of
the fractures around the elbow, they usually result from falling
in a position that makes the palmar surface hit the ground9.
The Mason classification is generally used in categorizing
fractures of the head of the radius. While Mason type 1
fractures can be treated conservatively, Mason type 2 fractures
are often treated by open reduction and internal fixation. For
Mason type 3 fractures that we focus on here, no consensus
exists as to the best treatment modality. However, one of the
most commonly applied techniques for many years has been total
excision of the radial head9.
Total excision is preferred in comminuted fractures, usually
because sufficiently sized fragments for internal fixation are
lacking, when the consistency of the coronoid process and the
condition of the ligamentous structures of the elbow gain
importance with respect to elbow stability6,8,9. In a
recent cadaveric study, the effect of the radial head on elbow
stability was demonstrated to be approximately 28–30%8.
In cases with additional coronoid process fractures and/or
ligament injury, excision of the radial head may lead to chronic
instability at the elbow joint5,6. In such cases, the
treatment of choice could be directed to fixation of coronoid
process, soft tissue repair, or prosthetic replacement of the
radial head6,9. In a recent study, however,
prosthetic radial head replacement without ligament repair
failed to provide sufficient elbow stability11. Thus,
we believe that performing a prosthetic replacement to increase
elbow stability and to achieve radius length is an appropriate
approach in cases with total radial head excision.
Outcomes of total excision of the head of the radius after
isolated radial head fractures are satisfactory according to
many studies1,3. The type of fracture, presence of
additional pathologies, and time of operation are also factors
affecting clinical outcomes. Herbertsson et al. performed either
primary or late total excision in 61 patients with Mason types
2, 3, or 4 fractures, and obtained satisfactory results, except
for type-4 fracture cases; no difference was detected between
primary and late phase cases1.
In Sanchez-Sotelo’s study of 10 cases, patients were followed
for a mean duration of 4.6 years. Early results of the total
excision were reported to be satisfactory, but long-term results
of the intervention were not discussed3.
Some studies, however, have reported poor results on performing
total excisions. In Leppilathi’s paper, 23 subjects underwent
total radial head excisions; elbow and wrist joints were checked
after 5 years on average and showed apparently restricted
movement in 17 elbow and 14 wrist joints. This study concluded
that this finding originated primarily from shortening of the
radius2. In the study of Ikeda et al., 15 patients
with Mason type-2 and -3 fractures underwent total radial head
excisions, and only five cases demonstrated good results.
Subjects were followed for 10 years on average, and pain was
shown to have persisted in 10 subjects, accompanied by loss of
movement and function. This study recommended that total
excision in comminuted radial head fractures not be performed
for patients doing physical work4.
In our study, 11 of 23 patients had fair or poor clinical
outcomes, which we consider unsatisfactory, leading us to
evaluate this technique with suspicion. As demonstrated,
although readily applicable, total excision is a method with an
outcome that may not be as innocent as it appears. In recent
studies, the PLRI context is frequently encountered, which led
us to assess the technique in detail.
PLRI is the most commonly seen pattern of elbow instability, as
first described by O’Driscoll in 1991,5,14 in which
abnormal external rotation of the ulna over the humerus and
subsequent valgus displacement in the trochlea of the humerus
was the underlying mechanism15. The lateral ulnar
collateral ligament (LUCL) is the anatomical structure
responsible for posterolateral rotator instability14.
Clinical findings may consist of a history of recurrent elbow
dislocation, the presence of painful clicks, and a feeling of
elbow dislocation during daily activities, followed by an
apprehensive state. If PLRI is symptomatic, LUCL repair or
reconstruction of the ligament by tendon graft should be
considered15.
While PLRI could result iatrogenically from lateral approaches
to the elbow, as in a radial head excision or tennis elbow
operation, it may also arise secondary to elbow trauma, such as
an elbow dislocation or comminuted fracture of the head of the
radius. Using MRI, Itamura et al. showed that 18 of 24 cases
(80.1%) with Mason type-2 and -3 fractures had concurrent
development of LUCL rupture12.
LUCL is one of the four parts of the lateral collateral ligament
(LCL); the others are the radial collateral ligament, the
annular ligament, and the accessory lateral collateral ligament.
These components can exhibit individual variations. LUCL
attaches at the anteroinferior aspect of the lateral condyle
proximally and attaches at the ulnar supinator crest distally.
In this way, it not only contributes to the formation of valgus
resistance, but also prevents posterior dislocation of the
radial head via a supportive effect. Moreover, it prevents
abnormal external rotation of the ulna over the humerus. In our
opinion, however, intraoperative assessment of LUCL is important
for elbow stability, and if it is torn, repair or reconstruction
of the ligament subsequent to the total radial head excision is
an appropriate approach. If, however, the ligament cannot be
repaired, we believe that performing a prosthetic replacement to
increase elbow stability and restore radius length is the
approach of choice.
Clinical demonstration of PLRI is not always easy7.
Several specific tests are used to diagnose this condition, all
of which are based on same rationale: they eventually result in
an “apprehensive” state in patients, as observed in anterior
shoulder instability and form a “groove sign” at the elbow,
accompanied by subluxation of the proximal radius. Nevertheless,
patients sometimes develop dramatic apprehension and resistance,
an unpleasant condition.
One such test is the “Lateral Pivot-Shift Test” described by
O’Driscoll in 19915. In this test, the arm is made to
extend while the patient is in a supine position. Concurrent
with axial loading, the elbow is forced to the valgus position.
However, this maneuver is difficult to perform while the patient
is awake, so it is recommended that it be carried out under
general anesthesia5. Another test is the “push-up
test” described by Regan et al. in 20067. The patient
is first asked to assume the push-up position. If fear ensues
when the elbow is extended from flexion and subluxation appears
at the radial head, the test outcome is deemed to be positive.
In the same article, the chair test was also described in which
the patient is seated on a chair. If the same signs appear when
the patient puts a load on his/her arm to stand up, the test is
considered positive.
The last test for diagnosing PLRI is the “tabletop test”
described by Arvind et al. in 200610. Similar to the
other tests, it consists of enduring a load while the elbow is
extended, with the patient staying near the table17.
In our study, all of these tests were performed by the same
physician and showed no significant difference that could have
influenced the outcome. The tabletop and chair tests are likely
to be more practical compared to the other tests.
Today, studies are successfully assessing LUCR using MRI12.
From a radiological point of view, ulna plus deformity at the
wrist joint may attract attention (Fig. 3). The underlying
mechanism for this deformity is the relative lengthening of
ulna, secondary to the shortening of radial length after
excision. Whereas the distal articular surface of ulna is in
line with the distal ulnar articular surface of the radius under
normal conditions, the ulna appears in a position as if it
descended distally. In ulna plus deformity, inspection of the
wrist joint may exhibit an apparent deformity that may also be
painful.
In our study, 12 patients had positive ulnar variation, four of
whom had severe deformities of 10, 10, 15, and 24 mm, which led
to clinical complaints. This severity of radius shortening can
be related to the size of the excised radial head. Thus,
appropriate choice of an osteotomy level that avoids unnecessary
distal involvement or prosthetic replacement of the radial head
is a good solution.
Conclusions :
Comminuted radial head fracture is a frequently
seen condition in which the degree of energy causing the trauma
has a net effect on the outcome. Total radial head excision is
the most commonly used treatment modality. Note, however,
despite its relatively easy application, this intervention can
be associated with complications such as posterolateral rotator
instability, chronic elbow pain, loss of function at the elbow
joint, and ulna plus deformity at the wrist joint. For this
reason, total excision of the radial head should be avoided; if
this is not possible, integrity of LUCL should be evaluated
intraoperatively. If a LUCL tear is present, it should be
repaired; if this is not possible, a radial head prosthesis
should be applied. The proximal portion of the radius should
never be left uncontrolled.
Reference :
-
Herbertsson P, Josefsson PO, Hasserius R,
Besjakov J, Nyqvist F, Karlsson MK. Fractures of the radial
head and neck treated with radial head excision.
J Bone Joint Surg Am. 2004
Sep;86-A(9):1925-30.
-
Leppilahti J, Jalovaara P. Early excision of
the radial head for fracture. Int Orthop.
2000;24(3):160-2.
-
Sanchez-Sotelo J, Romanillos O, Garay EG.
Results of acute excision of the radial head in elbow radial
head fracture-dislocations. J Orthop Trauma.
2000 Jun-Jul;14(5):354-8.
-
Ikeda M, Oka Y. Function after early radial
head resection for fracture: a retrospective evaluation of 15
patients followed for 3-18 years. Acta Orthop
Scand. 2000 Apr;71(2):191-4.
-
O'Driscoll SW. Classification and evaluation
of recurrent instability of the elbow. Clin
Orthop Relat Res. 2000 Jan;(370):34-43.
-
Hall JA, McKee MD. Posterolateral rotatory
instability of the elbow following radial head resection.
J Bone Joint Surg Am. 2005 Jul;87(7):1571-9.
-
Regan W, Lapner P. Prospective evaluation of
two diagnostic apprehension signs for posterolateral
instability of the elbow. J Shoulder Elbow
Surg. 2006 May-Jun;15(3):344-6.
-
Jensen SL, Olsen BS, Sojbjerg JO. Elbow joint
kinematics after excision of the radial head.
J Shoulder Elbow Surg. 1999 May-Jun;8(3):238-41.
-
Jensen SL, Olsen BS, Tyrdal S, Sojbjerg JO,
Sneppen O. Elbow joint laxity after experimental radial head
excision and lateral collateral ligament rupture: efficacy of
prosthetic replacement and ligament repair. J
Shoulder Elbow Surg. 2005 Jan-Feb;14(1):78-84.
-
Arvind CH, Hargreaves DG. Tabletop relocation
test: a new clinical test for posterolateral rotatory
instability of the elbow. J Shoulder Elbow
Surg. 2006 Nov-Dec;15(6):707-8. Epub 2006 Aug 7.
-
Beingessner DM, Dunning CE, Gordon KD, Johnson
JA, King GJ. The effect of radial head excision and
arthroplasty on elbow kinematics and stability.
J Bone Joint Surg Am. 2004
Aug;86-A(8):1730-9.
-
Itamura J, Roidis N, Mirzayan R, Vaishnav S,
Learch T, Shean C. Radial head fractures: MRI evaluation of
associated injuries. J Shoulder Elbow Surg.
2005 Jul-Aug;14(4):421-4.
-
Steinberg EL, Golomb D, Salama R, Wientroub S.
Radial head and neck fractures in children. J
Pediatr Orthop. 1988 Jan-Feb;8(1):35-40.
-
O'Driscoll SW, Bell DF, Morrey BF.
Posterolateral rotatory instability of the elbow.
J Bone Joint Surg Am. 1991 Mar;73(3):440-6.
-
Mehta JA, Bain GI. Posterolateral rotatory
instability of the elbow. J Am Acad Orthop
Surg. 2004 Nov-Dec;12(6):405-15.
|