|
Abstract:
Purpose:
The anterior drawer test is used to evaluate the degree of
anterior translation of the shoulder. However, it is difficult to perform it,
when the patient’s relaxation is not achieved.
Thus,
we evaluated the findings of arthroscopy and computed
tomographic arthrography in young, highly active men with
traumatic anterior shoulder dislocation or subluxation to
determine the objective factors that can predict the degree of
anterior translation
regardless of the patient’s relaxation.
Methods: A total of 65 patients 67 shoulders were
enrolled in this study. On the basis of the degree of anterior
translation of the shoulder, which was evaluated with the
patients under anaesthesia, we divided the patients with limited
shoulder movement into 2 groups: stable and unstable groups.
There were 8 patients (8 shoulders) in the stable group and 57
patients (59 shoulders) in the unstable group. We compared the
findings of arthroscopy and computed tomographic arthrography
between the stable and unstable groups.
Results: In the
univariate analysis, capsular insertion type and condition of
the
anterior band of the inferior glenohumeral ligament
were associated with excessive anterior translation (p
< 0.001).
However, logistic regression analysis revealed capsular
insertion type to be the strongest factor of excessive anterior
translation of the shoulder (p = 0.012).
Conclusion:
Evaluation of capsular insertion type on computed tomographic
arthrography after shoulder subluxation or dislocation is a
useful method to predict excessive anterior translation of the
shoulder.
J.Orthopaedics 2009;6(3)e5
Keywords:
Shoulder;
Anterior
translation;
Dislocation;
Young men;
Computed
tomographic arthrography;
Arthroscopy
Introduction:
Young men are prone to the risk of the recurrence of initial
traumatic anterior shoulder dislocation.1, 2 Anterior instability of
the shoulder is usually evaluated by manual tests such as
apprehension test, relocation test, and anterior drawer test.3
Anterior drawer test is considered to be useful in confirming
the subluxated or dislocated shoulder, but it is difficult
when the patient’s relaxation is not achieved
because of shoulder pain. Therefore, it was recommended to be
performed under anaesthesia (EUA)4, but it is
difficult on outpatient basis. Other methods that can confirm
the subluxated or dislocated shoulder on outpatient basis
reliably equivalent to EUA are required. Some clinicians have
attempted to identify the factors of the anterior stability of
the shoulder from the objective findings of X-ray, magnetic
resonance imaging or computed tomographic arthrography (CTA) and
considered fracture of the greater tuberosity (Hill-Sachs
lesion) or anterior glenoid rim (bony Bankart lesion) as a risk
factor for redislocation.2,5
Structures such as the anterior labrum, anterior band of the
inferior glenohumeral ligament (AIGHL), and rotator cuff are
also considered important for the anterior stability of the
shoulder.6–11 Further, in some studies, capsular
insertion type has been considered to enhance the anterior
stability of the shoulder.8,12 However, no studies
appear to have investigated the factors of anterior translation
of the shoulder in young men with traumatic anterior shoulder
dislocation. Therefore, this study aimed to investigate the
objective factors that could predict the degree of anterior
translation reliably equivalent to EUA in young men with
anterior shoulder dislocation or subluxation by the findings of
arthroscopy and CTA.
Materials and Methods:
Between April 2000 and February 2008, we performed arthroscopic
or open Bankart repair and the Bristow procedure in 91 patients
(93 shoulders) with anterior shoulder dislocation or subluxation
at our institution. We reviewed their information charts and
surgical records, and enrolled 70 patients (72 shoulders) on the
basis of the following inclusion criteria: (1) males, (2) age
less than 30 years at initial dislocation or subluxation, (3)
traumatic initial dislocation or subluxation, (4) no
multidirectional instability, (5) no history of symptomatic
shoulder before the initial injury, (6) observation of Bankart
and Hill-Sachs lesions at arthroscopy, and (7) no observation of
concomitant injury except bony Bankart lesion and superior
labrum anterior-to-posterior (SLAP) lesion at arthroscopy. Total
21 patients (21 shoulders) were excluded from this study: 10
patients had no obvious injury at initial dislocation or
subluxation or had multidirectional instability, 3 were over 30
years of age at initial dislocation or subluxation, 4 patients
had posterior labrum lesions, 2 had previously undergone other
shoulder surgery, and 2 patients were females. All the patients
except 1 high school student were members of the Self Defense
Force: this student was a rugby player. As compared to the other
shoulder, the flexion, abduction, and external rotation of the
injured shoulder were observed to be 10° lesser on examination
of all the patients under anaesthesia. On the basis of the
degree of anterior translation of the shoulder, which was
evaluated with the patients under anaesthesia, we divided the
patients with limited shoulder movement into 2 groups: stable
and unstable groups. There were 8 patients (8 shoulders) in the
stable group and 62 patients (64 shoulders) in the unstable
group. The average ages at initial injury and at the time of
surgical treatment were 23.7 years (15–30 years) and 24.3 years
(16–31 years), respectively, in the stable group and 21.2 years
(14–29 years) and 24.8 years (19–34 years), respectively, in the
unstable group (Table. 1). In the stable group, 7 patients (7
shoulders) experienced primary dislocation, while the remaining
1 patient (1 shoulder) showed recurrent dislocation or
subluxation. Of the 7 patients with primary shoulder dislocation
or subluxation, 5 did not feel any anterior instability of the
shoulder; however, they were unable to return to preinjury
activities because of shoulder pain. Surgical repair was
performed in the remaining 2 patients shortly (4 weeks–2 months)
after the initial injury. They had negative anterior
apprehension test results, and therefore, the symptoms were
unclear. The patient with recurrent dislocation had been able to
play rugby for 4 months after the initial dislocation without
any symptoms, but he injured his shoulder again while playing
rugby 6 months after the initial dislocation. In the unstable
group, on the other hand, 8 patients (8 shoulders) experienced
primary dislocation and 54 patients (56 shoulders), recurrent
dislocation or subluxation. Six patients with primary shoulder
dislocation or subluxation and all the 54 patients with
recurrent dislocation or subluxation were unable to return to
preinjury activities because of a sense of anterior instability.
Surgical repair was performed in the remaining 2 patients with
primary shoulder dislocation or subluxation shortly (6 weeks and
2 months) after the initial injury. They had positive anterior
apprehension test results before surgical repair.
|
Table 1 Patient demographics
|
|
|
|
|
|
Stable group |
Unstable group |
p |
|
Number of patients / shoulders |
8 / 8 |
57 / 59 |
― |
|
Average age at initial injury (range) (years) |
23.7 (15-30) |
21.2 (14-29) |
0.058 |
|
Average age at surgery (range) (years) |
24.3 (16-31) |
24.8 (19-34) |
0.98 |
|
Male/Female |
8 / 0 |
57 / 0 |
― |
|
Aetiology of initial injury (shoulders) |
|
|
|
|
Traumatic / Atraumatic |
8 / 0 |
59 / 0 |
― |
|
|
|
|
|
|
*Determined
using the Student t test. |
Based upon previously reported findings, we selected 4 variables
from the arthroscopic and CTA findings and compared these
variables between the stable and unstable groups. The variables
were capsular insertion type, SLAP lesion, bony Bankart lesion,
and condition of the AIGHL. In addition to these variables, the
average ages at surgery and at initial dislocation or
subluxation were also compared between the 2 groups. All the
shoulders had Bankart and Hill-Sachs lesions; therefore, these
findings were excluded. Rotator cuff tear was not observed in
all the shoulders, and therefore, this was also excluded. It was
difficult to evaluate the CTA findings in 5 patients (5
shoulders) in the unstable group, because the injected air
leaked from their shoulder joints; therefore, these patients
were excluded. Finally, 8 patients (8 shoulders) in the stable
group and 57 patients (59 shoulders) in the unstable group were
included in this study.
Evaluation of CTA findings
We performed CTA in all the patients before surgical repair.
Contiguous 2-mm- or 3-mm-thick axial slices of the glenohumeral
joint were obtained at 2- or 3-mm intervals with Xvision
TSX-002A (Toshiba, Tokyo) after injection of 15-ml air into the
joint. We examined the images for capsular insertion and bony
Bankart lesion. Capsular insertion was examined at the mid-glenoid
level (half-way between the superior and inferior glenoid rims)
and at the inferior glenoid level (three-quarters of the
distance between the superior and inferior glenoid rims), as
reported by Palmer.10 These levels were determined by
counting the total number of axial images through the glenoid
fossa. Thus, if there were total 12 images, capsular insertion
was examined at the level of images 6 and 9. Capsular insertion
was assigned different types on the basis of the classification
given by Moseley.8
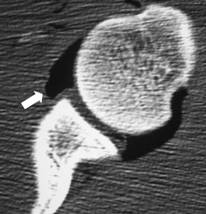
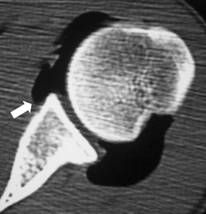
Type 1 indicated a capsular insertion on the labrum (Fig.1-A),
while type 2 indicated an insertion at the glenoid neck within 1
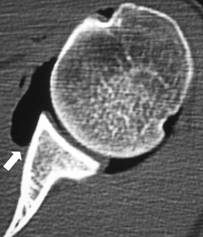
cm of the labrum base (Fig.1-B). Type 3 indicated an insertion
at the glenoid neck more than 1 cm medial to the labrum base
(Fig.1-C).
Fig.1-A, 1-B, and 1-C: Classification of capsular insertion
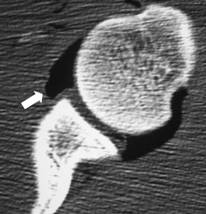
Fig.1-A: A type 1 capsule arising from the labrum.
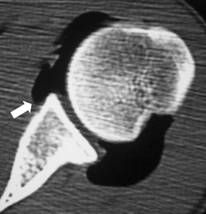
Fig.1-B: A type 2 capsule arising from the scapular neck 1 cm
medial from the labral base.
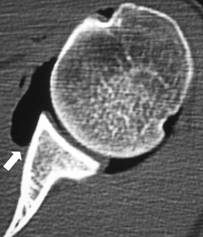
Fig.1-C: A type 3 capsule arising from the scapular neck more
than 1 cm medial from the labral base.
We defined type 1 capsular insertion when the insertion at both
the mid- and inferior glenoid levels was type 1, type 2 capsular
insertion when the insertion was type 2 at either the mid- or
the inferior glenoid level, and type 3 capsular insertion when
the insertion was type 3 at either the mid- or the inferior
glenoid level.
Bony Bankart lesion was considered to be present when bony
fragment of the anterior glenoid rim was observed and absent
when no bony fragment was observed on any image.
Evaluation of arthroscopic findings
We evaluated the anterior translation of the shoulder on
examination under anaesthesia, SLAP lesion from the patients’
surgical records, and condition of the AIGHL. These evaluations
were routinely performed for all the patients before the repair
of the Bankart lesion: all these evaluations were performed and
recorded by 1 co-author. The degree of anterior translation was
evaluated by manual anterior drawer test with the patient in
supine position and with the arm in 90°
of abduction and external rotation, and
graded as reported by Hawkins.3 The grading was as
follows: translation less than 25% of the humeral head, normal;
translation up to 50% of the humeral head, grade 1; translation
greater than 50% of the humeral head (subluxation of the humeral
head over the glenoid rim), grade 2; and frank dislocation,
grade 3. The patients with normal and grade 1 anterior
translation were assigned to the stable group and those with
grade 2 and grade 3 anterior translations to the unstable group.
Condition of the AIGHL was assessed as reported by Horii.13
The AIGHL was considered good when the ligament was clearly
observed and its upper proximal end was located in the area
superior to the middle-glenoid level or when the ligament could
be easily raised by a probe to the area above the middle glenoid
level. If the AIGHL did not satisfy this condition, it was
considered poor.
SLAP lesion was considered to be present when type 2, type 3, or
type 4 SLAP lesion was observed and absent when no SLAP lesion
was observed.
Statistical analysis
Univariate analysis was performed to evaluate the association
between anterior stability of the shoulder and the variables
selected in this study. Independent t test was used to assess
patient-group differences in average age at initial dislocation
or subluxation and at surgery. Fisher’s exact test was used to
assess the differences between categorical variables. Logistic
regression analysis with removal at p ≥ 0.15 was used to
identify the significant factors for anterior stability. The
threshold for significance in this study was set at a p value of
0.05. Analyses were performed using SPSS version 11.5 (SPSS
Inc., Chicago, Illinois).
Results :
The results of the univariate analysis of the variables with
regard to anterior stability are shown in Table 2. SLAP lesion
was absent in 5 shoulders and present in 3 shoulders (type 2: 2
shoulders, type 3: 1 shoulder) in the stable-group patients,
while it was absent in 37 shoulders and present in 22 shoulders
(type 2: 16 shoulders, type 3: 3 shoulders, type 4: 3 shoulders)
in the unstable-group patients. The lesion was not associated
with excessive anterior translation. Bony Bankart lesion was
observed in 21 shoulders, but no large bony fragment involving
greater than 20% of the glenoid fossa was observed. This lesion
was also not associated with excessive anterior translation. In
the stable group, 2 out of the 8 shoulders showed type 2 or type
3 capsular insertion, but in the unstable group, 57 of the 59
shoulders showed type 2 or type 3 capsular insertion. This type
of insertion was significantly associated with excessive
anterior translation. Similarly, condition of the AIGHL was
significantly associated with excessive anterior translation.
Table 2
Findings
of CTA and arthroscopy associated
with the outcome
| |
Stable
group |
Unstable
group |
p |
|
SLAP lesion
Present / Absent (shoulders)
Bony Bankart lesion
Present / Absent (shoulders)
AIGHL
Good / Poor (shoulders)
Type of capsular insertion
Type1 / Type2 or Type 3 (shoulders)
|
3 / 5
1 / 7
6 / 2
6 / 2
|
22 / 37
20 / 39
7 / 52
2 / 57
|
0.637
0.212
< 0.001
< 0.001
|
|
*Determined
using the Fisher’s exact test. |
Age at initial injury, type 2 or type 3 capsular insertion, and
poor AIGHL were entered into the logistic regression analysis:
the result is shown in Table 3. Type 2 or type 3 capsular
insertion was found to be the strongest factor of excessive
anterior translation.
|
Table 3 Logistic regression analysis for identifying the
factors of excessive anterior translation |
|
|
|
|
|
|
|
|
|
|
|
p |
Odds ratio |
95% confidence interval |
|
|
|
Age at initial injury |
0.264 |
0.85 |
0.65 to 1.12 |
|
|
|
Poor AIGHL |
0.354 |
3.63 |
0.24 to 55.37 |
|
|
|
Type 2 or type 3 capsular insertion |
0.012 |
33.23 |
2.13 to 517.6 |
|
|
Moreover, we compared these variables between the patients with
initial dislocation or subluxation of the shoulder in the stable
and unstable groups (7 shoulders from each group). Logistic
regression analysis could not be performed because of a small
number of shoulders. However, capsular insertion type was found
to be significantly associated with excessive anterior
translation in the univariate analysis (p = 0.01).
Discussion :
The labrum contributes about 20 % to glenohumeral stability7,
but only Bankart lesion is insufficient to cause anterior
dislocation of the shoulder.14 In our study, each
shoulder had a Bankart lesion, but the degree of anterior
translation was observed to be different between the stable and
unstable groups. Therefore, we considered that Bankart lesion
might contribute only slightly with the degree of anterior
translation. SLAP and bony Bankart lesions were also not
associated with excessive anterior translation. Itoi5
has reported that a large bony Bankart lesion including more
than 21% of the glenoid fossa caused excessive anterior
translation, but no shoulder had a large bony Bankart lesion in
our study.
In some reports, the AIGHL has been considered the major
stabilizing restraint of anterior translation11, and
its high odds ratio in this study showed that it could be
associated with the degree of anterior translation, though this
could not be statistically proved. Age at initial dislocation
did not influence the degree of anterior translation in this
study.
We considered the
exclusion of patients with over 30 years at initial injury in
this study was caused of this result.
In this study, capsular insertion type was significantly
associated with excessive anterior translation. Some reports
have indicated that type 2 or type 3 capsular insertion is
associated with the anterior instability of the shoulder.8,12
However, Palmer10 investigated the prediction
of anterior instability of the shoulder by comparing magnetic
resonance (MR) arthrography and surgical findings of stable and
unstable shoulders and concluded that capsular insertion type
plays no role in the prediction of shoulder instability.
However, he included shoulders without dislocation or
subluxation in his study. Therefore, we considered that his
result did not reflect the prediction of anterior instability of
the shoulders after dislocation or subluxation. We found type 2
or type 3 capsular insertion was associated with excessive
anterior translation in our study, however, we did not know
whether type 2 or type 3 capsular insertion was associated with
anterior instability. One of the reasons for the high ratio of
type 2 or type 3 capsular insertion in the unstable group was
that capsular insertion was classified into type 2 or type 3
when the labrum was displaced medial to the glenoid neck, even
if the capsule was inserted on the labrum. However, many
shoulders with type 2 or type 3 capsular insertion in the
unstable group had no labrum displacement. Therefore, we
considered that the capsular insertion might be type 2 or type 3
initially before dislocation or subluxation. Singson12
has also documented that the formation of a large anterior pouch
in type 3 capsular insertion is less likely after recurrent
dislocations in shoulders with strong capsular walls or with
initially small or no anterior pouch. We considered that if
capsular insertion was found to be type 2 or type 3 on CTA after
shoulder dislocation or subluxation, the shoulder had a high
possibility of excessive anterior translation which could be
subluxated or dislocated even by manual stress. Therefore,
surgical treatment in early stage would be suitable. Howkins3
documented excessive translation alone did not equal
instability, though it was related to instability. However, in
his study15, he examined the degree of anterior
translation of the shoulder in 18 patients with no history of
glenohumeral
instability, 10 patients with recurrent anterior dislocation,
and 10 patients with multidirectional instability, and he
reported no shoulders
with no history of glenohumeral
instability had
excessive anterior translation which could be subluxated or
dislocated
by manual stress under aneasthesia unlike the shoulders with
recurrent anterior dislocation or multidirectional instability.
Therefore, we considered the shoulder with excessive
anterior translation which could be
subluxated or dislocated by manual stress would be abnormal. On
the basis of the result of this study, we considered that
evaluation of capsular insertion type on CTA enabled us to
predict excessive anterior translation of the shoulder and it is
a useful method, especially when the anterior drawer test was
difficult to perform on a patient, because he experienced pain.
This study has several limitations. First, most of the shoulders
in the stable group were symptomatic. Although none of the
stable-group patients felt anterior instability of the shoulder
before surgical treatment, 5 of the 8 patients experienced pain
when their shoulders were in 90°
abduction and maximum external rotation; further, minor
instability was suggested. Moreover, 1 patient had redislocation,
although it had occurred due to a high-energy injury. Shoulders
showing no symptoms for a long time after dislocation or
subluxation should be included in the stable group, but
arthroscopic evaluation of these shoulders was difficult due to
the invasiveness of the procedure. Therefore, we did not include
such shoulders in this study. Capsular insertion type could not
evaluate anterior instability of the shoulder in this study.
Second, many shoulders in this study had recurrent dislocation
or subluxation, which may invite criticism. However, we consider
that initial and recurrent dislocations or subluxations may be
similar condition. In fact, separate analysis of initial
dislocations or subluxations also suggested a correlation
between capsular insertion type and anterior translation.
Although the number of shoulders analysed was small, we believe
that the difference between primary and recurrent dislocation or
subluxation may have little effect on the result. Third, we
excluded shoulders with complicated lesions other than
Hill-Sachs, Bankart, bony Bankart, or SLAP lesion from this
study. Therefore, the result of this study may not apply to
shoulders with complicated lesions other than those mentioned
above.
Conclussion:
Logistic regression analysis revealed type 2 or type 3 capsular
insertion to be the strongest factor of excessive anterior
translation of the shoulder. Evaluation of capsular insertion
type on computed tomographic arthrography after shoulder
subluxation or dislocation is a useful method to predict
excessive anterior translation of the shoulder.
Reference :
-
Kralinger FS, Golser K, Wischatta R, Wambacher M, Sperner G.
Predicting recurrence after primary anterior shoulder
dislocation. American Journal of Sports Medicine. 2002; 30:
116-20.
-
Shimonet WT, Cofield RH. Prognosis in anterior shoulder
dislocation. American Journal of Sports Medicine. 1984; 12:
19-24.
-
Hawkins RJ, Mohtadi NGH. Clinical evaluation of shoulder
instability. Clinical Journal of Sport Medicine. 1991; 1:
59-64.
-
Warner JJP, Miller MD, Marks P, Fu FH. Arthroscopic Bankart
repair with the
Suretac
device. Part Ι:
Clinical observations. Arthroscopy. 1995;11:2-13.
-
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a
glenoid defect on anteroinferior stability of the shoulder
after Bankart repair: a cadaveric study. Journal Bone and
Joint Surgery, American volume. 2000; 82: 35-46.
-
Lee SB, Kim KJ, O’Driscoll SW, Morrey BF, An KN. Dynamic
glenohumeral stability provided by the rotator cuff muscles in
the mid-range and end-range of motion:
a study in cadavera. Journal Bone and Joint Surgery, American
volume. 2000; 82: 849-57.
-
Lippitt SB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT
2nd, Matsen FA 3rd. Glenohumeral stability from
concavity-compression: a quantitative analysis. Journal of
Shoulder and Elbow Surgery. 1993; 2: 27-35.
-
Moseley HF, Overgaard B. The anterior capsular mechanism in
recurrent anterior dislocation of the shoulder. Morphological
and clinical studies with special reference to the glenoid
labrum and the gleno-humeral ligaments. Journal Bone and Joint
Surgery, British volume. 1962; 44: 913-27.
-
Pouliart N, Gagey O. Concomitant rotator cuff and
capsuloligamentous lesions of the shoulder: a cadaver study.
Arthroscopy. 2006; 22: 728-35.
-
Palmer WE, Caslowitz PL. Anterior shoulder instability:
diagnostic criteria determined from prospective analysis of
121 MR arthrograms. Radiology. 1995; 197: 819-25.
-
Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing
mechanisms preventing anterior dislocation of the glenohumeral
joint. Journal Bone and Joint Surgery, American volume. 1981;
63: 1208-17.
-
Singson RD, Feldman F, Bigliani L. CT arthrographic patterns
in recurrent glenohumeral instability. American Journal of
Roentgenology. 1987; 149: 749-53.
-
Horii M, Kubo T, Kurokawa M, Hirasawa Y. MRI evaluation of the
inferior glenohumeral ligament. Comparison with arthroscopic
findings in 81 shoulders. Acta Orthopaedica Scandinavica.
1998; 69: 163-6.
-
Speer KP, Deng X, Borrero S, Torzilli PA, Altchek DA, Warren
RF. Biomechanical evaluation of a simulated Bankart lesion.
Journal Bone and Joint Surgery, American volume. 1994; 76:
1819-26.
-
Hawkins RJ, Schutte JP, Janda DH, Huckell GH. Translation of
the glenohumeral joint with the patient under aneathesia.
Journal of Shoulder and Elbow Surgery. 1996; 5: 286-92.
|