|
Abstract:
Telangiectatic osteosarcoma is a rare subtype of osteosarcoma.
The commonly existed delay in diagnosis or misdiagnosis
potentially impairs the outcome and the prognosis. We
experienced a case of telangiectatic osteosarcoma presenting as
rare refractory hemorrhage, who suffered poor prognosis.
Thereafter, we present the case of the telangiectatic
osteosarcoma with rare manifestation to avoid further
misdiagnosis and improve the outcome and diagnosis.
J.Orthopaedics 2009;6(3)e13
Keywords:
osteosarcoma; telangiectatic osteosarcoma; refractory
hemorrhage; misdiagnosis
Introduction:
Telangiectatic osteosarcoma (TOS) represents 2.5%–12.0% of all
osteosarcomas.1-6 The combination of operation and
chemotherapy has improved the outcome and prognosis of
telangiectatic osteosarcoma. Prompt diagnosis is essential for
effective treatment. Delay in diagnosis will potentially impair
the treatment and outcome. The case, presenting with rare
refractory hemorrhage after right femoral shaft fracture treated
with internal fixation, was addressed in the paper to avoid
further misdiagnosis.
Materials
and Methods:
Case presentation
Telangiectatic osteosarcoma presented with refractory hemorrhage
is extremely scarce in the literature. We present a patient with
right femoral shaft fracture. The patient was initially
misdiagnosed as conventional fracture and treated by open
reduction and internal fixation in the local hospital. The
patients suffered progressive swelling at the distal femur
ensuing refractory hemorrhage. Final pathologic examination
confirmed a rare variant of osteosarcoma of the telangiectatic
type.
Case presentation
An 18-year old boy suffered right femoral shaft fracture with
significant pain and swelling when he skipped in the farm and
fell down onto the ground. The patient was admitted into the
local hospital and the fracture was confirmed on the radiographs
(Figure 1). Open reduction and internal fixation was performed
(Figure 2). The initial recovery course was uneventful, however,
the patient suffered fever and progressive swelling in the right
thigh one month later postoperatively. Physical examination
found significant swelling and high temperature in the region of
incision without other evidence of infection, effusion or
pus(Figure 3). Aspiration in the swelling revealed uncoagulated
hemorrhage and biopsy found no tumor cells. The patient was
transferred to our hospital, a level one trauma center, for
definite diagnosis and effective treatment. The stainless steel
internal fixation made the MR imaging scan impossible. CT scans
with contrast media demonstrated leakage of the contrast medium
around the femur, swelling muscle and massive hematoma with
apparent compression on the right femoral artery and right deep
femoral artery (Figure 4). Arterial injury was suspected and
angiograph was conducted from the left femoral artery. The
contrast media was found to overflow from the penetrating
branches of the deep femoral artery and the above-knee branches
of the femoral artery. The injured branches of the deep femoral
artery were embolized by gelatin sponge (Figure 5). However, the
swelling went on and the blood routine examination showed severe
anemia (RBC 2.02*1012/L, HGB 61g/L). Repeat blood transfusion
was conducted which could not reverse the condition of anemia.
The swelling of the right thigh became so severe that the
patient complained of progressive pain and anesthesia which
implied osteo-fascial compartment syndrome. Exploration into the
swelling was performed. 2000ml unaggregated blood and
approximate 400ml necrotic tissue was cleaned out in the right
thigh(Figure 6A and 6B). The muscle and other soft tissue were
dropsical, fragile and compressed significantly. No apparent
injured arteries were identified, however, errhysis was fully
filled in the wound which could not be stopped by electric
coagulation or ligation due to the crisp muscle. The incision
was finally closed with sterile package to stop bleeding(Figure
6C). During operation, 2400ml whole blood and 1000ml plasma was
transfused to maintain stable blood pressure.

Figure 1
The comminution fracture of the right femur (A, the
anterioposterior view and B, the lateral view).

Figure 2
The fracture was treated with open reduction and internal
fixation (A, the anterioposterior view and B, the lateral view).
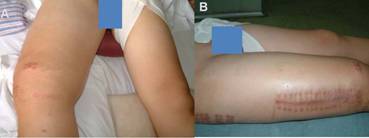
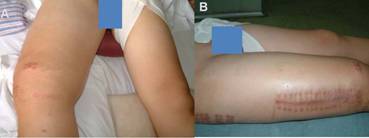
Figure 3
The right thigh appeared significant swelling and high
temperature (A and B).
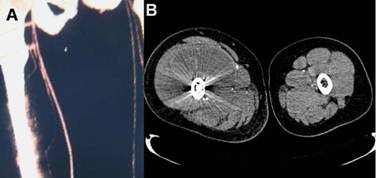
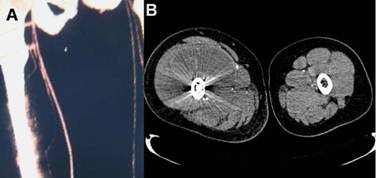
Figure 4
CT scan with contrast administration demonstrated leakage of the
contrast medium around the femur, massive hematoma with apparent
compression on the right femoral artery and right deep femoral
artery (A) and swelling muscle(B).
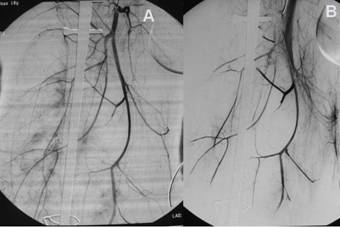
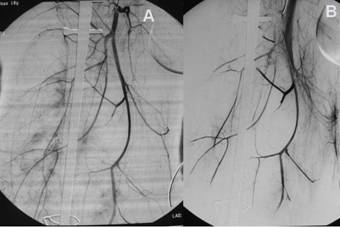
Figure 5
During angiograph, the contrast media overflow extensively from
the penetrating branches of the deep femoral artery and the
above-knee branches of the femoral artery(A). The injured
branches of the deep femoral artery were embolized by gelatin
sponge (B).

Figure 6
Massive unaggregated blood and necrotic tissue was cleaned out
in the right thigh (A and B) and the incision was closed with
sterile package to stop errhysis(C)
The package took effect during the first few days after
operation, and swelling relieved and the blood routine
examination demonstrated rising red cell and hematoglobin. The
drainage of errhysis decreased from 400ml per day to 200ml per
day. An extensive consultation was performed among the experts
in Orthopedics, Hematopathy and Traumatology. They arrived at a
conclusion that the patient suffered coagulation
disorder-acquired combined deficiency of coagulation factor
(deficiency of blood coagulation factors
Ⅱ,Ⅶ,
Ⅸ
and
Ⅹ).
400ml of fresh frozen plasma and 600U of prothrombin complexity
were transfused once a day for two days. The hemoglobin rose as
high as 110g/L. The package was dislodged and the incision was
closed with a drain pipe on the third day after operation.
However, the drainage of errhysis grew more from 400ml/day to
1360ml/day. The red blood cell and the hemoglobin re-decreased
to a worse level than the former examination five days later
even with persistent application of the fresh frozen plasma,
cryoprecipitation, and prothrombin complexity. The patient was
transferred to another level I trauma center in Beijing. However
the cause of the refractory hemorrhage was still uncertain and
the hemorrhage was still uncontrolled. The hemoglobin and the
red blood cell continued decrease. The drainage of the errhysis
could not decrease. The general condition of the patient became
worse and worse. The amputation was finally performed due to
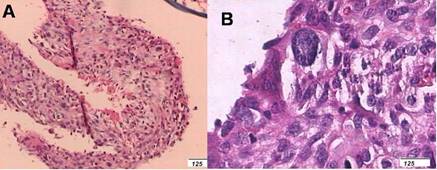
high fever and significantly severe anemia. Pathological
examination was performed. Characteristically, the lesion is
primarily composed of multiple aneurysmal dilated cavities that
contained blood and necrotic tissue, with high-grade sarcomatous
cells and irregular osteoid in the peripheral rim and septations
around these spaces(Figure 7). Some of the malignant cells
showed typical mitoses. This confirmed the diagnosis of
telangiectatic osteosarcoma. Follow-up studies showed local
recurrence and pulmonary metastasis 16 months after surgery.
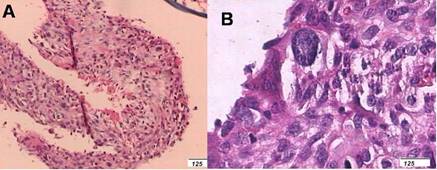
Figure 7
The thin and irregular osteoid(A) and the typical osteosarcomous
cells(B) lied unevenly in the septations of the cysts.
Discussion :
Multiple histologic subtypes of osteosarcoma have been
identified, the osteoblastic osteosarcomas, chondroblastic
osteosarcomas, fibroblastic osteosarcoma and telangiectatic
osteosarcoma. Telangiectatic osteosarcoma typically occurs in
the extremities. Its greatest predilection is for the metaphysic
of long bones, most often in bones adjacent to the knee joint
and shoulder. Like conventional osteosarcoma, pain and swelling
are the usual initial symptoms.7, 8 Another common
symptom is pathological fracture. TOS was associated with a high
rate of pathologic fracture and patients with TOS are at a
higher risk of pathologic fractures than patients with
conventional OS.1, 9 The rate of pathologic fracture
among patients with TOS (17–32%) was significantly higher than
that in conventional OS (6-13%).7, 9-12 Weiss report
9 of 21 patients (43%) had pathologic fractures in their study
of TOS.13 A even high rate of pathologic fracture
(61%) also was noted in a Murphy’s retrospective review of
radiologic features in 36 patients with TOS.14 One
possible explanation for the high rate of pathologic fractures
in patients with TOS is the extensively lytic and cystic nature
of the tumor, which may make the bone more prone to fracture.15
The patient suffered pathological fracture during a lower energy
activity- skipping in the farm and falling down onto the ground.
The review of the lateral and anteroposterior radiographs of the
right femur demonstrated osteolytic lesion in the metaphysic
with blotches of high density. Radiographs of this typical
lesion showed geographic bone lysis, a wide zone of transition,
and matrix mineralization. This subtle osteoid was recognized on
only 58% of radiographs.13,16 However, the
radiological feature was ignored by the local orthopedic
surgeon. During the ensuing treatment, the swelling and the
refractory hemorrhage confused us. The coagulation disorder was
primarily considered as the diagnosis and the therapeutic
protocols were mainly aimed to control the refractory
hemorrhage. Characteristically, telangiectatic osteosarcoma is
primarily (>90%) composed of multiple aneurysmally dilated
cavities that contain blood and necrotic tissue, with viable
high-grade sarcomatous cells around the periphery and septations
of these spaces.1-6,16-20 The telangiectatic
osteosarcoma may be more aggressive clinically than conventional
osteosarcoma.21, 22 The refractory hemorrhage is the
manifestation of the histological features of TOS since the
internal fixation has connected the blood-filled cavity with the
muscles outside of the periosteum. Definitive diagnosis on the
basis of pathological examination was delayed until amputation
was conducted. Delay diagnosis resulted in incorrect treatment
and poor outcome. Local recurrence and pulmonary metastasis was
noticed 16 months after surgery.
Conclusions:
Results of the recent studies related TOS indicate that survival
has improved apparently which is similar or even better than
that of conventional high-grade intramedullary osteosarcoma. The
presence of a pathologic fracture was not associated
significantly with the type of surgery or patient outcome
either. Therefore, it is important to provide accurate diagnosis
promptly with ensuing effective treatment. The aim of presenting
the case is to demonstrate the rare refractory hemorrhage of TOS.
All-round acknowledgment of TOS can confirm the prompt diagnosis
of the lesion to avoid misdiagnosis and guarantee the outcome
and the prognosis.
Reference :
-
Matsuno T, Unni KK, McLeod RA, Dahlin DC. Telangiectatic
osteogenic sarcoma. Cancer. 1976; 38(6):2538-2547.
-
Farr GH, Huvos AG, Marcove RC, Higinbotham NL, Foote FW, Jr.
Telangiectatic osteogenic sarcoma. A review of twenty-eight
cases. Cancer. 1974;34(4):1150-1158.
-
Campanacci M. [Atypical manifestations of osteosarcoma].
Chir Organi Mov. 1971;59(4):346-348.
-
Huvos AG, Rosen G, Bretsky SS. Telangiectatic osteogenic
sarcoma: a clinicopathologic study of 124 patients. Cancer.
1982;49:1679-1689.
-
Mervak TR, Unni KK, Pritchard DJ, McLeod RA. Telangiectatic
osteosarcoma. Clin Orthop Relat Res. 1991;
(270):135-139.
-
Bertoni F, Pignatti G, Bacchini P, Picci P, Bacci G,
Campanacci M. Telangiectatic osteosarcoma: a clinical
pathological study of 41 patients at Rizzoli Institute.
Prog Surg Pathol. 1989;10:63-70.
-
Vanel D, Tcheng S, Contesso G, Zafrani B, Kalifa C, Dubousset
J et al. The radiological appearances of telangiectatic
osteosarcoma. A study of 14 cases. Skeletal Radiol.
1987;16(3):196-200.
-
Kerr R. Telangiectatic osteosarcoma. Orthopedics.
1986;9(2):246, 248-251.
-
Bacci G, Ferrari S, Ruggieri P, Biagini R, Fabbri N,
Campanacci L et al. Telangiectatic osteosarcoma of the
extremity: neoadjuvant chemotherapy in 24 cases. Acta
Orthop Scand. 2001;72(2):167-172.
-
Scully SP, Ghert MA, Zurakowski D, Thompson RC, Gebhardt MC.
Pathologic fracture in osteosarcoma : prognostic importance
and treatment implications. J Bone Joint Surg Am.
2002;84-A(1):49-57.
-
Jaffe N, Spears R, Eftekhari F, Robertson R, Cangir A, Takaue
Y et al. Pathologic fracture in osteosarcoma. Impact of
chemotherapy on primary tumor and survival. Cancer.
1987;59(4):701-709.
-
Scully SP, Temple HT, O'Keefe RJ, Mankin HJ, Gebhardt M. The
surgical treatment of patients with osteosarcoma who sustain a
pathologic fracture. Clin Orthop Relat Res. 1996;
(324):227-232.
-
Weiss A, Khoury JD, Hoffer FA, Wu J, Billups CA, Heck RK et
al. Telangiectatic osteosarcoma: the St. Jude Children's
Research Hospital's experience. Cancer.
2007;109(8):1627-1637.
-
Murphey MD, wan Jaovisidha S, Temple HT, Gannon FH, Jelinek
JS, Malawer MM. Telangiectatic osteosarcoma: radiologic-pathologic
comparison. Radiology. 2003;229(2):545-553.
-
Rosen G, Huvos AG, Marcove R, etal. Telangiectatic osteogenic
sarcoma. Improved survival with combination chemotherapy.
Clin Orthop Relat Res. 1986;207:164-173.
-
Ruiter DJ, Cornelisse CJ, van Rijssel TG, van der Velde EA.
Aneurysmal bone cyst and telangiectatic osteosarcoma. A
histopathological and morphometric study. Virchows Arch A
Pathol Anat Histol. 1977;373(4):311-325.
-
Larsson SE, Lorentzon R, Boquist L. Telangiectatic
osteosarcoma. Acta Orthop Scand. 1978;49(6):589-594.
-
Ruiter DJ, van Rijssel TG, van der Velde EA. Aneurysmal bone
cysts: a clinicopathological study of 105 cases. Cancer.
1977;39(5):2231-2239.
-
Kaufman RA, Towbin RB. Telangiectatic osteosarcoma simulating
the appearance of an aneurysmal bone cyst. Pediatr Radiol.
1981;11(2):102-104.
-
Batsakis JG. Osteogenic and chondrogenic sarcomas of the jaws.
Ann Otol Rhinol Laryngol. 1987;96(4):474-475.
-
Link MP, Eilber F. Osteosarcoma. In: Pizzo P, Poplack D,
editors. Principles and Practice of Pediatric Oncology.
Philadelphia: Pa: Lippincott-Raven Publishers; 1997; 889-920.
-
Dhir SP, Munjal VP, Jain IS, Banerjee AK, Sharma SK.
Osteosarcoma of the orbit. J Pediatr Ophthalmol Strabismus.
1980;17(5):312-314.
|