|
Abstract:
We report a successful in situ fixation procedure for the
medial condyle in juvenile osteochondritis dissecans (OCD) of
the knee after arthroscopic retroarticular drilling failed. Our
patient was a 13-year-old boy who felt right knee pain for six
months while playing baseball. Plain radiographs and computed
tomography (CT) showed a 20 mm
´
25 mm radiolucent zone in his medial condyle and magnetic
resonance imaging (MRI) showed abnormal intensity in the same
region. We diagnosed OCD and no separation from cartilage was
seen under arthroscopy following retroarticular drilling with
K-wire, after conservative treatment for six months had failed.
After transient disappearance of the knee pain, it persisted for
eight months after the first drilling. Plain radiographs and CT
showed a discrepancy in a fragment from the subchondral bone.
No separation was identified arthroscopically and an 8.5 mm
osteochondral graft was harvested from the center of the lesion
and reimplanted in its original position after drilling
sclerotic bone marrow. The patient’s knee pain disappeared in
two months and union was attained one year after the second
surgery. This case shows the limitation of retroarticular
drilling for large lesions and in situ fixation of stable
osteochondral lesions without any other osteochondral harvest as
an effective treatment option.
J.Orthopaedics 2009;6(3)e11
Keywords:
Osteochondritis dissecans; Knee, Retroarticular Drilling; in
situ fixation
Introduction:
Osteochondritis dissecans (OCD) of the femoral condyle is seen
with increased frequency in adolescents and young adult
patients. It may respond to conservative treatment such as
immobilization, restriction of weight bearing and sports
activity; however, some cases require surgery. Surgical
treatment includes drilling 1,2,3,4, fixation 5,
meniscus transplantation 6, osteochondral allogeneic
or autologous graft 7, and chondrocyte implantation
8.
Retroarticular drilling without bone grafting for OCD is less
invasive and an effective surgical treatment 1.
However, it demands skill and may not effect bone union, the
exact rate of which remains unknown. Furthermore, a reliable
method for reoperating in cases of non-union has not yet been
established. We present the successful in situ fixation
of a medial osteochondral lesion without any other graft harvest
in stable juvenile OCD of the knee after retroarticular drilling
failed.
Case report:
A 13-year-old boy presented at our outpatient clinic with a
six-month history of right knee pain when playing baseball. He
had no swelling; ballottement and tenderness of the medial
condyle were recognized. Range of motion was 120°
flexion and 0°
extension. McMurray’s test was negative and Wilson’s test was
positive. Radiography indicated a radiolucent zone in the
medial condyle classified as an extended type of Aichroth’s
classical site. CT showed a 20 mm
´
25 mm
´
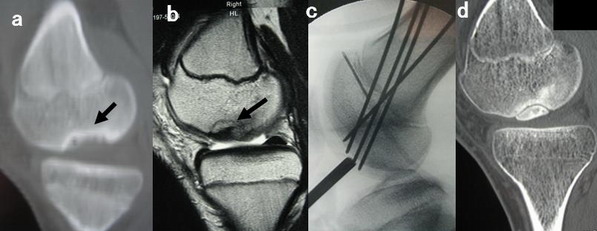
10 mm osteolytic lesion in the medial condyle (Fig. 1a). MRI
showed both a low and isointensity area in T2-weighted images
(Fig. 1b). The lesion was classified as Nelson grade 1. We
diagnosed our patient with OCD of the medial femoral condyle and
treated him conservatively, restricting sports activity for six
months. Pain did not respond to conservative treatment and a
standard arthroscopy was performed through the medial and
lateral infrapatellar approach. The preoperative Lysholm score
was 66 points. The cartilage of the medial condyle showed a 15
mm
´
20 mm softened area, which showed 0–30°
of weight-bearing area by probing, and was not separated from
the subchondral bone. Four retroarticular drillings to the
lesion from the medial epicondylar with 1.5 mm K-wire were
performed under arthroscopy using an image intensifier so as not
to penetrate the cartilage and open physis (Fig. 1c).
Continuous passive motion was begun one week postoperatively.
Partial weight bearing was allowed at two weeks and full weight
bearing at six weeks. Pain was decreased one month
postoperatively and MRI showed communication between the lesion
and bone marrow. However, the patient’s pain had not
disappeared completely and was increased during light exercise.
Radiography showed separation from the subchondral bone eight
months after surgery. CT also detected the discrimination from
subchondral bone at twenty-two months (Fig. 1d). MRI indicated
the intensity was decreased, but that union had not been
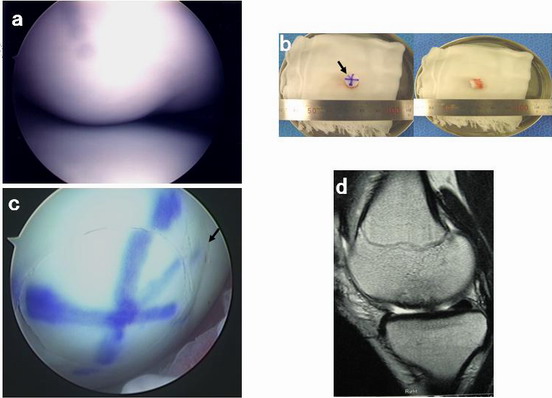
attained. We decided to reoperate. During the arthroscopy,
cartilage of the lesion showed softening in the same area as
previously, but with no apparent damage or separation (Fig.
2a). An arthrotomy was performed using a medial approach and a
medial condyle lesion was identified. Superficial cartilage of
the lesion was indicated using a purple marker and only an 8.5
mm width and 10 mm length from center of the lesion was
harvested using a mosaic plasty guide without any other graft
harvest (Fig. 2b). Multiple drillings made in the sclerotic
bone marrow area with 1.5 mm or 2.0 mm K-wire. After
identifying bleeding from the bone marrow, the harvested
osteochondral graft was reimplanted in the same position using
the marker line for guidance without any fresh bone grafting.
Arthroscopy showed no step off around the intact cartilage (Fig.
2c). Continuous passive motion was started one week
postoperatively. Partial weight bearing was allowed at two
weeks and full weight bearing at four weeks. The patient’s knee
pain disappeared completely within two months and he returned to
full sports activity. He displayed a full range of motion and
no tenderness at final follow-up. Radiography showed a complete
union and MRI indicated almost the same intensity around the
intact area one year postoperatively (Fig. 2d). The Lysholm
score was 100 points at one year after the second
operation.
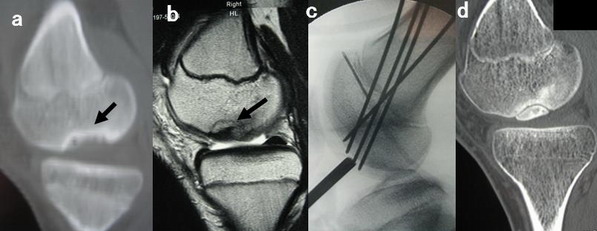
Figure 1.
(a) Preoperative CT, saggital view. Black arrows indicate the
lesion. (b) Preoperative MRI, saggital view (T2-weighted
image). Black arrows indicate the lesion. (c) Screen display as
seen intraoperatively during drilling showing four
extraarticular drillings with 1.5 mm K-wire so as not to damage
either the cartilage or epiphysis. (d) Postoperative CT,
saggital view. Discrimination of the fragment is clear.
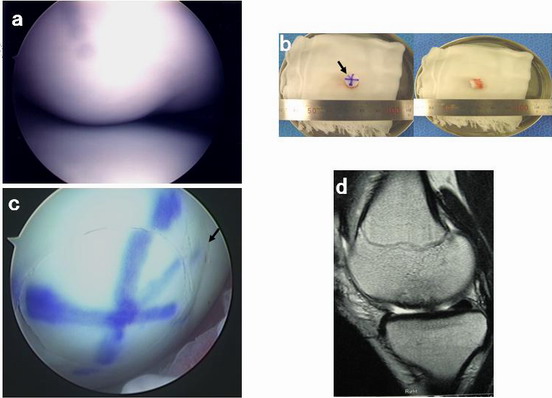
Figure 2.
(a) Arthroscopic findings of the 15 mm
´
20 mm softening lesion with 0–30°
partial weighting area. (b) Harvested 8.5 mm osteochondral graft
with purple marking. Black arrows indicate the purple marking.
(c) Arthroscopic findings of osteochondral graft implantation in
bone marrow following the purple line. Black arrows indicate
the purple marking. No step off is seen after reimplantation of
the osteochondral graft. (d) Postoperative MRI, saggital view
(T2-weighted image).
Discussion:
Surgical treatment for OCD has been reported
1,2,3,4,5,6,7,8. In particular, the effect of
arthroscopic drilling for OCD remains controversial. Antegrade
2,4 or retrograde drilling 1,3 are
effective ways to stabilize juvenile OCD. Antegrade drilling
for juvenile OCD is easy and specific to the lesion; however, it
can cause cartilage damage. Once cartilage damage has occurred,
it is weakened by shearing stress, and degenerative
osteoarthritis may follow. Extraarticular drilling for OCD was
reported by Kawasaki and all 16 lesions were perfectly joined at
a mean of 4 postoperative months as determined radiographically
3. Adachi reported the outcome of stable juvenile
OCD of the knee with retroarticular drilling without bone
grafting, 16 of which were performed from the epicondyle area
1. The unhealed rate was 5% (1/20) in that study.
This method is technically demanding to avoid penetration of the
cartilage layer and open epiphysis. In particular, the
direction from the cartilage layer to epiphyseal line is limited
when drilling the lesion and delayed or non-union may occur.
In contrast, Jürgensen concluded that the rates of remission and
progression were not significantly effective between
conservative and arthroscopic treatment as evaluated by MRI
9. We treated our 13-year-old patient with stable OCD by
retroarticular drilling; however, a union was not attained. Two
reasons why union was not attained in our patient were
considered. One was the size of the lesion. Anderson reported
four cases of non-union in twenty-four cases after antegrade
drilling 2. Two were cases in which the epiphyseal
line was not closed and in which the lesions were 2 cm
´
3 cm and 2.5 cm, respectively. The lesion size in our patient
was 2 cm
´
2.5 cm
´
1 cm and this may have been a limitation for extraarticular
drilling. The other cause is the timing of the closure of the
epiphyseal line. On the first drilling, the epiphyseal line was
not closed; however, it might have been closed by the second
operation. The gap between the first and second operations was
almost two years and the biological healing capacity could have
been reduced gradually during this time.
In cases where a large area is affected as in this case, it is
not clear what diameter of in situ osteochondral graft is
appropriate to unite bone. The lager the graft selected, the
wider the remaining lesion. The dimension of the 8.5 mm graft
was one-sixth of that of the entire lesion in this case and only
this size could be used to attain union. Further study is
needed to determine the appropriate graft size for lesions to
attain union in the OCD. This finding is interesting in terms
of OCD etiology.
This case is an example of the limitations of retroarticular
drilling and the use of osteochondral in situ fixation
without any other graft harvest as an option in case of
retrograde drilling failure. This method might be a useful
alternative in cases of stable OCD in which the size of the
lesion is large and there is closure of the epiphyseal line.
Reference :
-
Adachi N, Deie M,
Nakamae A et al.
Functional and radiographic outcome of stable juvenile
osteochondritis dissecans of the knee treated with
retroarticular drilling without bone grafting. Arthroscopy
2009;52:145–152.
-
Anderson AF, Richards DB, Pagnani MJ et al. Antegrade drilling
for osteochondritis dissecans Arthroscopy 1997;13:319–324.
-
Kawasaki K, Uchio Y, Adachi N et al. Drilling from the
intercondylar area for the treatment of osteochondritis
dissecans of the knee. Knee 2003;10:257–263.
-
Kocher MS, Micheli LJ, Yaniv M et al. Functional and
radiographic outcome of juvenile osteochondritis dissecans of
the knee treated with transarticular arthroscopic drilling Am
J Sports Med 2001;29:562–566.
-
Victoroff BN, Marcus RE, Deutsch A. Arthroscopic bone peg
fixation in the treatment of osteochondritis dissecans in the
knee. Arthroscopy
1996;12:506–509.
-
Deie M, Sumen Y, Adachi N et al. The long-term results of
meniscus transplantation for articular cartilage defects in
the knee joint. Knee Surg Sports
Traumatol Arthrosc 2007;15:61–66.
-
Emmerson BC,
Görtz S, Jamali AA et al.
Fresh osteochondral allografting in the treatment of
osteochondritis dissecans of the femoral condyle.
Am J
Sports Med
2007;35:907–914.
-
Ochi M, Uchio Y, Kawasaki K et al. Transplantation of
cartilage-like tissue made by tissue engineering in the
treatment of cartilage defects of the knee. J Bone Joint Surg
[Br] 2002;84:571–578.
-
Jürgensen I, Bachmann G, Schleicher J et al. Arthroscopic
versus conservative treatment of osteochondritis dissecans of
the knee: value of magnetic resonance imaging in therapy
planning and follow-up. Arthroscopy 2002;18:378–386.
|