|
Abstract:
Patients
with metastatic carcinoma commonly have multiple lytic bone
lesions. We
present a patient with multiple bone lytic lesions who by
clinical, radiologic and morphologic evidence appeared to have
metastatic carcinoma.
MRI revealed lesions in the right ilium, right sacroiliac
joint, right proximal femur, left ilium and left side of the
sacrum. Both
CT and MRI did not disclose any soft tissue mass or
lymphadenopathy. A
biopsy of the left posterior iliac crest showed a high grade
undifferentiated neoplasm with a marked desmoplastic response.
Only after exclusion of non-hematopoietic neoplasms by an
extended immunohistochemical panel was the diagnosis of primary
bone lymphoma (PBL, centroblastic variant) made.
This report illustrates the necessity of radiologic and
morphologic correlation in establishing the correct diagnosis.
PBL can infrequently involve multiple bones of the pelvis
in the absence of a soft tissue mass or regional lymphadenopathy
with an associated carcinoma-like desmoplastic response.
J.Orthopaedics 2009;6(2)e7
Keywords:
lymphoma;
bone; metastatic; carcinoma
Introduction:
PBL is an
infrequent bone lesion, representing only 5% of all bone
neoplasms.1 Patients typically complain of
localized pain and/or a palpable mass. PBL is defined as a
lymphoma involving a single skeletal site with or without
involvement of regional lymph nodes.2 Less
commonly, PBL involves multiple bones with an associated soft
tissue mass. Long bones are most frequently involved,
primarily at the diametaphysis. Thus clinical and
radiologic criteria may be used to suggest PBL in the
differential diagnosis. The presence of multiple lytic
bone lesions, especially in flat bones such as the pelvis, in
the absence of an associated soft tissue mass and with no
regional lymphadenopathy is more frequently associated with
metastatic carcinoma.3 We report a patient with
the later presentation who after careful pathologic and
radiologic correlation was diagnosed with a PBL. This
report demonstrates the importance of clinicopathologic
evaluation as well as a systematic immunohistochemical approach
to the diagnosis of PBL. Furthermore, PBL may be
associated with a striking carcinoma-like desmoplastic reaction.
Case
Report:
A
53 year old woman complained of generalized abdominal pain as
well as back pain. Physical
exam did not reveal any specific findings.
A CT
scan disclosed a lytic lesion involving the left portion of the
sacrum adjacent to the inferior portion of the left sacroiliac
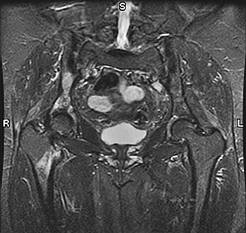
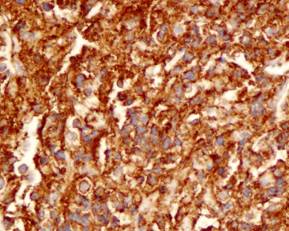
joint. An MRI
revealed lytic lesions in the right ilium, the right sacroiliac
joint, right proximal femur, left ilium and left side of the
sacrum near the left sacroiliac joint (Figure 1).
No soft tissue mass or lymphadenopathy was seen.
The radiologic impression was that of metastatic disease.
Figure
1: MRI of the pelvis and femoral heads showing multiple lesions
in the right inferior pelvis, right proximal femoral head, left
ilium and left sacrum.
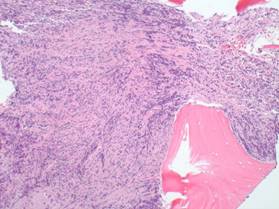
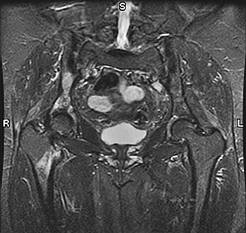
A
bone biopsy of the left posterior iliac crest was performed.
Approximately 20-30% of the bone biopsy showed a high grade
malignancy with associated fibrous tissue and bone sclerosis
(Figure 2).
Figure
2: Infiltrative malignant cell population with fibrosis and bone
sclerosis, suggestive of metastatic carcinoma
(hematoxylin-eosin, original magnification X10).
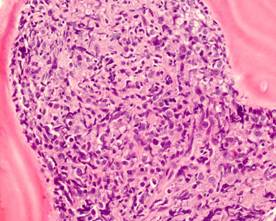
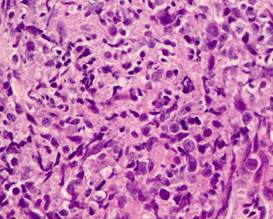
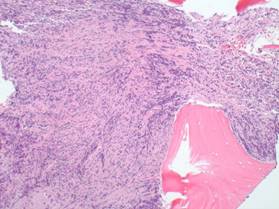
The
cells revealed large nuclei with vesicular chromatin and
non-prominent nucleoli infiltrating in a non-cohesive pattern
(Figure 3, 4).
Figure
3: Large, malignant non-cohesive cells with associated fibrosis
(hematoxylin-eosin, original magnification X20).
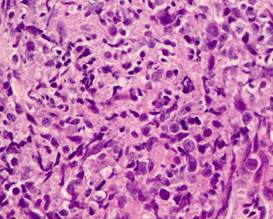
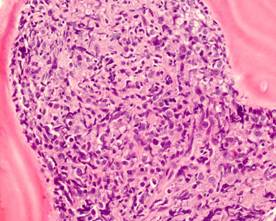
Figure
4: Malignant cells with large nuclei and vesicular chromatin
pattern (hematoxylin-eosin, original magnification X40).
In
addition there were areas of osteoclastic and osteoblastic
activity with prominent woven bone formation and sclerosis.
Immunohistochemistry showed the atypical population was positive
for CD45, CD20, and CD79a (Figure 5). They were focally
positive for BCL-6 and CD10. These cells were negative for
CK7, CK20, Cam5.2, Mak6, CK AE1/AE3, EMA, TTF-1, MART-1, HMB-45,
EMA, CD3 and CD138. Based on the immunohistochemical
findings, the diagnosis of large B cell lymphoma, centroblastic
variant was made. Of note, the bone marrow aspirate did not
reveal any malignant cells.
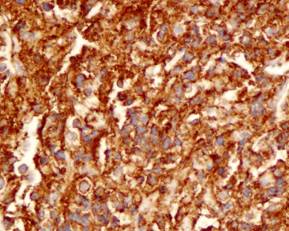
Figure
5: The malignant cells reveal CD20 positive immunostaining
(original magnification X40).
Discussion :
Metastatic
neoplasms are the most frequent of all malignancies of bone.3
In most cases the diagnosis is readily made since the
lesions are numerous and the presence of the primary malignancy
is known or evident. The
great majority of bone metastases originate in breast, lung,
prostate, thyroid or kidney.4
Approximately 70% of bone metastases affect the axial
skeleton (skull, ribs, spine, sacrum). The remaining metastatic
lesions involve large bones of the limbs alone or in combination
with the axial skeleton.
Radiologically,
the lesions are usually osteolytic, but may be osteoblastic or
both.5, 7 Periosteal bone proliferation and exuberant
new bone formation can less commonly occur.
In the absence of a known primary, histological
evaluation combined with a selective immunohistochemical panel
can narrow or confirm the nature of the neoplasm. Associated
histologic findings such as a marked desmoplastic response may
be also be helpful in identifying the presence of carcinoma.6
In
contrast to metastatic bone neoplasms, PBL is infrequent.
Although PBL usually affects the diaphysis or metaphysis
of a long bone, it can more rarely involve multiple bones, thus
simulating metastases.7
The absence of an associated soft tissue mass or
lymphadenopathy does not exclude the presence of PBL.
The diagnosis of PBL clearly requires histologic as well
as immunohistochemical analysis.
Usually the H and E stained tissue suggests a lymphoma as
opposed to a carcinoma, even in those cases where the clinical
and radiological findings are more suggestive of bone
metastases.
Our
patient revealed considerable clinical and radiological overlap
with bone metastases. PBL was not clinically suspected due to
the multifocal lytic lesions of the pelvis and the right
proximal femur. Furthermore, the absence of a soft tissue mass,
lymphadenopathy or “B” symptoms did not raise the
possibility of PBL to the clinicians or radiologists.
The presence of a high grade malignant cell infiltrate
associated with marked fibrosis and new bone formation continued
to suggest the diagnosis of bone metastasis even after reviewing
the H and E slides of the biopsy.
In fact, carcinoma frequently evokes a desmoplastic
response with new and sclerotic bone formation.
PBL usually infiltrates in an interstitial pattern with
at most associated increased reticulin fibers surrounding
individual or clusters of malignant cells.2
The
establishment of the correct diagnosis in this unusual
presentation of PBL required an extensive immunohistochemical
panel as well as correlation of the clinical and radiological
findings. Only with
an understanding of the less common pattern of bone involvement
by PBL as well as excluding carcinoma or other non-hematopoietic
neoplasms due to the marked associated fibrosis was the
diagnosis made. Furthermore,
subtyping of the non-Hodgkin lymphoma is critical to appropriate
management.8,9 This
PBL was of the centroblastic variant, germinal-center like
(BCL-6+, CD10+). In conclusion, a systematic approach to the
pathologic evaluation of bone lesions is of fundamental
importance. PBL has
quite different therapeutic and prognostic significance than the
other more frequently present neoplasms in the differential
diagnosis. Thus, missing the diagnosis of an atypical PBL
presentation can have serious consequences.
Reference :
-
Hicks
DG, Gokan T, O’Keefe RJ et al.
Primary Lymphoma of the Bone.
Cancer 1995;75:973-980.
-
Unni
KK, Hogendoorn PCW. Malignant
Lymphoma, In : Fletcher CDM, Unni KK, Mertens F, eds.
WHO Classification of Tumours: Pathology and Genetics
of Tumours of Soft Tissue and Bone, Lyon, France: IARC
Press; 2002:306-308.
-
Simon
MA, Bartucci EJ. The
search for the primary tumor of patients with skeletal
metastases of unknown origin.
Cancer 1986;58:1088-1095.
-
Berrettoni
BA, Carter JR. Mechanisms
of cancer metastasis to bone.
J Bone Joint Surg 1986;68:308-312.
-
Mulligan
ME, McRae GA, Murphey MD.
Imaging features of primary lymphoma of bone.
Am J Rad 1999;173:1691-1697.
-
Krishnan
C, George TI, Arber DA. Bone marrow metastases: a survey of
nonhematologic metastases with immunohistochemical study of
metastatic carcinomas. Appl Immunohistochem Mol Morphol
2007; 15: 1-7.
-
Huebner-Chan
D, Fernandes B, Yang G, Lim M.
An immunophenotypic and molecular study of primary
large B-cell lymphoma of bone.
Modern Pathology 2001; 14: 1000-1007.
-
De
Leval L, Braaten KM, Ancukiewicz M et al.
Diffuse large B-cell lymphoma of bone: An analysis of
differentiation-associated antigens with clinical
correlation. Am
J Surg Pathol 2003: 27:1269-1277.
-
Pettit
CK, Zukerberg LR, Gray MH et al.
Primary lymphoma of bone.
A B-cell neoplasm with a high frequency of
multilobated cells. Am
J Surg Path 1990;14:329-334.
|