|
Abstract:
The
aim of this study was to review a multicentre experience in
treating segmental humeral fractures and report related
complications and outcomes.
From 1996 to 2005 adult patients with segmental humeral
fractures were identified. Demographic details, method of
fixation, time to union and complications were recorded. At
follow up all patients were assessed in terms of radiological
result, range of movement and pain. Pain and range of movement
were combined to give a final outcome rated as good, moderate or
poor.
There were 63 patients.
22 non-operative, 11 intramedullary nailing, 17 plating, 2
Rush pins, 6 Enders nails and 5 external fixation. The non-union
rate was 22.2% (14 patients). 64.2% (9 patients) of the 14
non-union patients went on to union in one, but not both,
fracture sites. The Pearson chi-squared test is highly
significant (p=0.002).
It is clear that some treatments give better results than others
with nails showing better outcomes.
Despite the severity of this injury a satisfactory outcome can
be expected. The most successful method of surgical treatment
was found to be the intramedullary fixation.
J.Orthopaedics 2009;6(2)e6
Keywords:
Segmental;
humeral fracture; multicentre experience.
Introduction:
Segmental
humeral fractures have been successfully treated using closed
reduction and splinting followed by functional bracing21.
Sarmiento et al found consistent restoration of shoulder and
elbow movements with this method of treatment and similar
results were confirmed by others3,5. Severely
comminuted or segmental fractures however treated
non-operatively may predispose to an unsatisfactory outcome13.
Bone distraction and loss of fracture reduction could lead to
delayed or non-union of the fracture15. Surgical
stabilisation is advocated in certain circumstances including
failure of acceptable closed reduction13,6,17, open
fracture with nerve injury4, the multiply injured
patient6, pathological fracture14 and the
uncooperative patient6. Different stabilisation
techniques have been described including intramedullary nailing13,15,6,14,19,
open reduction and internal fixation (ORIF)6,4,16,25
or external fixation16. Intramedullary fixation
offers the advantages of biomechanical load-sharing6,
closed insertion technique6, decreased soft-tissue
disruption13,14 and preservation of the
extramedullary blood supply6. However, this method
has been implicated in the development of shoulder and elbow
dysfunction6,17 malrotation14 and radial
nerve palsy15. Chen et al6 stated that
plate osteosynthesis allows early active mobilisation of the
shoulder and elbow but may require extensive soft tissue
exposure and periosteal stripping13,6,14,15,25 thus
disturbing the local biological substrate of the fracture.
External fixation also plays its part particularly, although
certainly not exclusively, in stabilising open fractures16
but pin site infection, non-union and patient compliance may
limit their use16. Currently, the literature with
regard to the management and outcomes of segmental humeral
fractures remains poor.
The
aim of this study therefore was to review a multicentre
experience in treating segmental humeral (AO type 12B or C)
fractures. We wished to investigate the experience of our
institutions in managing these injuries and report related
complications and outcomes.
Materials
and Methods:
A
retrospective study of all adult patients treated with humeral
fractures in three trauma centres between 1996 and 2005 was
performed using clinical data and radiographs. Inclusion
criteria for participation in the study were the presence of
either a closed or an open fracture of the humerus with a
segmental component. Patients with impending or pathological
fractures were excluded. A segmental fracture was defined as a
two-level humeral fracture with at least one intermediate free
segment.
Fractures
were classified according to the AO system and type 12B or C
were included in the study20. Demographics, injury
severity score (ISS)2, mechanism of injury, whether
the fracture was closed or open (Gustilo Classification12),
presence of associated injuries and method of stabilisation were
recorded. Post-operative data such as the time to union,
incidence of delayed union and non-union, other complications
and range of movement were also recorded. Clinical healing was
defined as pain-free functional range of movement and
radiological union was defined as the evidence of callus
formation in both the antero-posterior and lateral radiographs.
Non-union was defined as a fracture not conforming to these
characteristics by 6 months post-injury. At the final follow-up
the patients were asked to complete a visual analogue scale for
pain (table 1) and examined for range of movement of the upper
limb (table 2). These were combined to give an overall
outcome score of good, moderate or poor (table 3).
|
Pain level on visual analogue scale (1-10)
|
Grade
|
|
1-3
|
Good
|
|
4-6
|
Moderate
|
|
>7
|
Poor
|
Table
1: Grading system for pain
|
Range
of movement
|
Grade
|
|
100%
to 50% of the normal range
|
Good
|
|
Between
50% and 25% of the normal range
|
Moderate
|
|
Less
than 25% of the normal range
|
Poor
|
Table
2: Grading system for range of movement.
|
Combination
of pain grade and range of movement grade
|
Outcome,
for the purposes of results and statistical analysis
|
|
Good
and good
|
Good
|
|
Good
and moderate
|
Moderate
|
|
Moderate
and moderate
|
Moderate
|
|
Moderate
and poor
|
Poor
|
|
Poor
and poor
|
Poor
|
|
Good
and poor
|
Moderate
|
Table
3: How the pain and range of movement grades were combined to
give a final outcome.
The
results were analysed using the Kruskal–Wallis test for
one-way non-parametric ANOVA (analysis of variance) using SPSS,
R18 and Stata23 packages.
Results :
Out
of 810 humeral shaft fractures identified from our prospectively
documented databases, 66 were found to fulfil the inclusion
criteria (8.1%). Out of 66 patients identified, there were 3
deaths all unrelated to fracture treatment leaving 63 cases for
the final analysis (Figure 1a,b,c,d). There were 33 females and
30 males with a mean age of 51.1 years (range 18–95) and a
mean ISS 14.1 (range 9–41). There were 29 type 12B (12B1, 9B2,
8B3) and 34 type 12C (16C1, 5C2, 13C3) fractures. The mean
length of the intermediate segment was 7.9 cm (range
3.5–17.5). The causes of injury included 23 vehicular
accidents, 22 falls from standing (elderly), 13 falls from
heights, 3 skiing injuries, 1 cyclist and 1 climber. Thirty
patients had associated injuries including head, chest, pelvis
and other long bone fractures. The mean follow up was 36 months
(range 24–60).
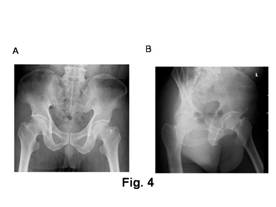 
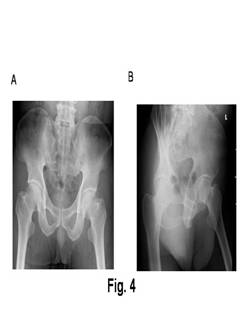 
Figure
1a and b
Radiographs showing a segmental humeral fracture in a 55 year
old female following a motorcycle collision.
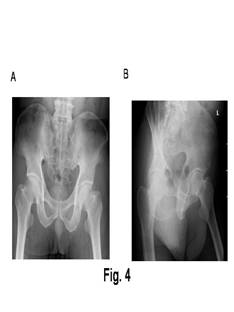   
Figure1
c and d
Antero-posterior and lateral radiographs showing union of the
fractures at the 5 month follow up having been originally
stabilised with plating.
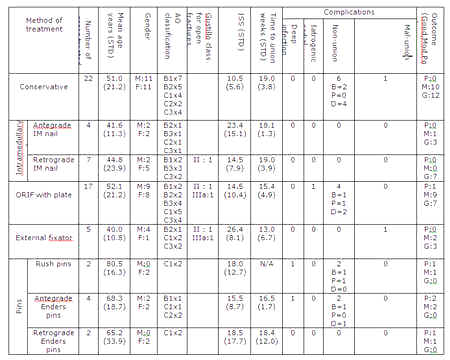
Demographics,
fracture classifications, Injury Severity Scores, methods of
treatment, complications and outcome measures are all presented
in table 4. We correlated total range of movement, complications
and time to union in all patients. For the purposes of analysis,
due to small numbers we combined Enders and rush pins to make
one group of ‘pins’. The overall non-union rate was 22.2%
(14 patients). In 9 out of 14 cases (62.4%) of non-union, one
site united but the other did not. The details are discussed in
the complications section.
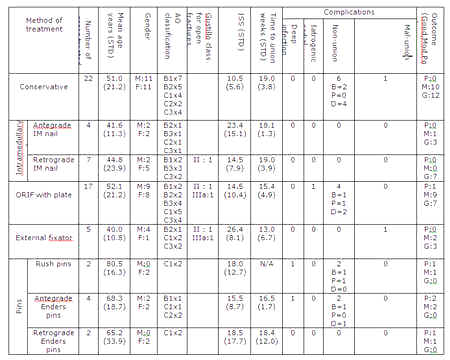
Key
Non-union column
B=Non-union both proximally and distally
P=proximal non-union only
D=distal non-union only
Table
4 : Results
Table
5 shows a simple comparison of outcome with treatment group. The
Pearson chi-squared test for association between treatment type
and outcome is highly significant (chi-square = 17.03 with 4
degrees of freedom and p=0.002).
Thus it is clear that some treatments give better results than
others with nails showing more good outcomes and pins much less
so.
|
|
|
Good or moderate/poor
|
Total
|
|
|
|
G
|
MP
|
|
|
Treatment
group
|
cons
|
Count
|
12
|
10
|
22
|
|
|
|
%
within Treatment group
|
54.5%
|
45.5%
|
100.0%
|
|
|
ex
fix
|
Count
|
3
|
2
|
5
|
|
|
|
%
within Treatment group
|
60.0%
|
40.0%
|
100.0%
|
|
|
nail
|
Count
|
10
|
1
|
11
|
|
|
|
%
within Treatment group
|
90.9%
|
9.1%
|
100.0%
|
|
|
pin
|
Count
|
0
|
8
|
8
|
|
|
|
%
within Treatment group
|
.0%
|
100.0%
|
100.0%
|
|
|
plate
|
Count
|
7
|
10
|
17
|
|
|
|
%
within Treatment group
|
41.2%
|
58.8%
|
100.0%
|
|
Total
|
Count
|
32
|
31
|
63
|
|
|
%
within Treatment group
|
50.8%
|
49.2%
|
100.0%
|
Table 5: Treatment group and good or moderate/poor cross
tabulation
The
above analysis is unadjusted for other factors such as sex and
age. Logistic regression was used to adjust for further
factors. A moderate/poor outcome can be predicted for pins and
so these patients were dropped from the analysis. Sex, ISS,
open/closed were all found to be not significant but age and
therapy type remained of interest since they were significant at
the 10% level in this exploratory model. A moderate or
poor outcome is considered bad and the adjusted results are: Age
OR=1.032 per year increase in age (95% CI is (0.999, 1.066), p-0.059)
so that the risk of bad outcome is increased with age; compared
to non-operative treatment, the OR for External Fixation is 5.12
(95% CI (0.43, 6.47), p=0.196),
the OR for Nail is 0.14 (95% CI (0.01, 1.33), p=0.087),
the OR for the Plating group is 1.82 (95% CI (0.47, 6.98), p=0.385).
Figure
2 demonstrates that range of movement varies considerably with
treatment. This is confirmed by Kruskal–Wallis test for
equality of median range of movement which is highly significant
(Chi-square=43.9; df=4, p=0.0001). Nails and external fixation
provided greater range of shoulder movement whilst Enders/Rush
pins and plates were more restrictive than non-operative
treatment.
Figure
2: Total range of movement against method of treatment. A
Kruskal–Wallis test for equality of median range of movement
yields c2= 43.9 with 4 d.f. (p= 0.0001).
Time
to union varies with type of treatment. The variation was small
however, with most fractures healing between 12 and 19 weeks.
The non-operative, plate and Rush/Enders pins groups did have
non-unions as detailed in the complications section of this
paper. Since these patients required revision surgery to achieve
union they did not have a true time union, therefore an analysis
would be unhelpful.
Complications
and outcomes:
a)
Non-operative treatment
Complications are summarised in Table 4. Of the twenty-three
patients who had non-operative management, six progressed to
non-union. Four had united at the proximal but not the distal
site. Two uni-nonunion and two bi-nonunion patients were
operated on with plating, 2 with iliac crest bone grafting.
These patients went on to bony union. The other two uni-nonunion
patients developed painless pseudoarthroses but were left alone
due to acceptable function and co-morbidities. Another
patient’s fracture displaced after a week of conservative
management and required a manipulation in theatre but went on to
union. Another patient developed a malunion but this was left
alone as she was functionally acceptable. There were 2 injury
related radial nerve palsies which both recovered within 4
months fully.
b)
Intramedullary nails
Eleven patients had intramedullary nail fixation. Only one
reported on-going shoulder discomfort post-operatively (antegrade
nail). There were no infections reported and no non-unions. One
case of injury-related radial nerve palsy was noted which
recovered within 8 weeks of the nailing.
c)
Plate fixation
Eighteen patients had plate fixation of their humeral fracture.
Four patients went on to non-union, three of whom had united at
one site but not the other (one ununited proximally and two
distally). Three were revised with further plating and bone
grafting from the iliac crest. The first of these patients had a
broken plate 8 weeks post initial operation. The second patient
was an open fracture which was revised with an LC-DCP at 20
weeks with bone grafting. The third non-union went on to have a
long-stem hemiarthroplasty inserted with a poor eventual
outcome. The fourth patient had a painless non-union and was
left alone. There were 3 radial nerve palsies. Two were injury
related and one iatrogenic intraoperatively. One patient whose
injury caused the palsy, fully recovered and in the other two
only partial recovery was noted.
d)
External fixation
One of the 5 patients in the external fixation group progressed
to a malunion and was taken down and revised with a plate. All
the other four externally fixated fractures (including one open
fracture) went on to satisfactory union. There was one case of
injury-related radial nerve palsy which resolved gradually over
1 month to full recovery.
e)
Pins
Two patients were treated with Rush pins and both progressed to
non-unions. One patient united distally but not proximally and
developed a painless pseudoarthrosis and was left alone. The
other was revised with double recon plates and iliac crest
autograft which then went on to union.
Six
patients had Enders nails inserted, 4 antegrade and 2
retrograde. Four went on to union. There were 2 cases of
non-union (both antegrade) and one of these became infected. The
infected case was later revised with a long stem
hemiarthroplasty with eventual outcome as moderate. The other
case of non-union (united proximally but not distally) had
revision with a plate. One injury related radial nerve
palsy occurred in the antegrade approach group which recovered.
Discussion :
Our
data suggests that patients who have fixation of their segmental
humeral fracture using an intramedullary nail, have a greater
chance of a good outcome than when treated by the other reported
methods.
There
is obscurity in the literature with regards to best treatment
method for the segmental humeral fractures. Balfour et al16
and Sarmiento et al21 stated that when uncomplicated
diaphyseal fractures of the humerus are treated conservatively
by reduction and subsequent immobilisation of the arm,
successful healing occurs in 95% to 98% of cases. However, these
studies are collective retrospective studies for one level, low
energy fractures. In these circumstances non-operative treatment
may be a good option but in our study we are dealing with
segmental fractures which are usually associated with high
energy trauma where significant soft tissue disruption has
occurred. The non-union rate for our non-operative group was
27.2% (6 cases). In many cases one site of the segmental
fracture went on to union but the other site did not. This can
be attributed to compromised biology or biomechanics of
attempted simultaneous healing in two sites.
Closed
locked nailing has been reported to yield satisfactory results
for femoral and tibial segmental fractures13.
Intramedullary nailing has the advantages of being relatively
minimally invasive, offers axial and rotational stability (when
locked) and good alignment. The literature suggests the union
rate for intramedullary nailing of straight forward humeral
shaft fractures is 95% with a low risk of problems such as
mal-union, delayed or non-union, infection or radial nerve palsy9.
In the herein study, locked nailing of segmental humeral
fractures yielded a 100% union rate in a mean time of 18.5
weeks. Amjal1 reported a 30% non-union rate when 33 humeri with
non-segmental but comminuted fractures were nailed using the
antegrade Russell-Taylor nail. He reported no significant
correlation between fracture comminution and healing time. All
the nailings in this study were reamed. One study that compared
nailing with and without reaming was unable to document
differences in union rates or complications9. Recent
interest has been directed towards the issue of axial loading on
surgically stabilised humeral diaphyseal fractures, with
controversy over the ideal method of fixation when it is
necessary6. When compared to plate fixation, for example, it is
generally well accepted that patients can load more confidently
through a nail than a plate4. We had one case of
shoulder pain post-operatively which was associated with one of
the proximally inserted nails. There were no other differences
between the antegrade and the retrograde nail group. We had no
cases of rotator cuff malfunction nor adhesive capsulitis.
Plate
fixation is an alternative method of treating segmental humeral
fractures4,25. The literature reports plating of
non-segmental humeral shaft fractures has a non-union rate of
3.6%14,10 but it traditionally requires an extensive
open operation with a variable degree of stripping of the soft
tissues from the bone. It also provides less secure fixation in
osteoporotic bone or if crutch walking is required14.
An argument for plating against nailing is the accurate fixation
under direct vision and control of malalingment and malrotation.
Plating is a very reasonable method of fixation for fractures
that cannot be nailed, for example, ones that are comminuted
close to the metaphysis (meaning that either the entry point or
the distal locking is compromised) or fractures associated with
radial nerve palsy which require exploration. The results of
plating in this study showed a 23.5% non-union rate. As with the
non-operative group, the relatively high rate of non-union could
be explained by considering that fact that one of the fractures
may not unite as can be the case in segmental fractures in all
long bones. There was also a case of compartment syndrome
post-operatively and one iatrogenic radial nerve palsy.
External
fixation is well recognised as a quick and easy way to stabilise
an extremity fracture whether open or closed. In our study the
results showed a 100% union rate albeit one patient had a
malunion. Care must be taken with pin sites although we had no
cases of deep infection in our study.
Rush
and Enders pins are used less frequently now as compared to
other intramedullary nailing fixation techniques. Here 4 of the
8 patients treated with these methods developed a non-union, 2
due to infection. The reason behind the high rate of non union
is possibly the poor stability that pins and nails provide to
the fracture site and in particular in segmental fractures. The
number of cases also is very small and a type II error could be
present.
We
are aware that this study has a number of limitations including
the retrospective nature, the non-randomisation process, a small
number of cases and the personal experience of four surgeons.
Furthermore the decision to operate or not and the type of
fixation was purely based on the surgeon’s decision. Despite
all of the above, the number of patients treated (63) provides
valid information compared to the current available literature
with scarce numbers of segmental humeral fractures 15,6,17,25.
Strengths of this study include its focus on this specific
subgroup of patients (segmental fractures and not humeral
fracture treatment in general), analysis of the different
methods of fixation (including non-operative treatment), the
multiple outcome measures analysed and the fact that there is an
element of randomisation as supported by the surgeon’s
preference in terms of management decision. The findings
therefore in the herein study can provide valuable information
when such rare cases are considered for stabilisation.
In
conclusion, this study noted consistently good results with
intramedullary nailing. The other management options may also be
considered but a higher rate of complications may be
encountered.
Reference :
-
Ajmal
M, O’Sullivan M, McCabe J, Curtin W. Antegrade locked
intramedullary nailing in humeral shaft fractures. Injury
2001;32:692–4.
-
Baker
S et al. The Injury Severity Score: a method for describing
patients with multiple injuries and evaluating emergency
care. J
Trauma 1974;14:187-196.
-
Balfour
G, Mooney V, Ashby M. Diaphyseal fractures of the humerus
treated with a ready-made fracture brace. J
Bone Joint Surg [Am] 1982;64-A:11.
-
Bell
M, Beauchamp C, Kellam J, McMurtry R. The results of plating
humeral shaft fractures in patients with multiple injuries. J
Bone Joint Surg [Br] 1985;67-B No.2:293-296.
-
Camden
P, Nade S. Fracture bracing the humerus. Injury
1992;23: 245.
-
Chen
AL, Joseph TN, Wolinsky PR et al. Fixation stability of
comminuted humeral shaft fractures: locked intramedullary
nailing versus plate fixation. J
Trauma, Injury, Infection and Critical Care 2002;
53(4):733-737.
-
Cole
P, Wijdicks. The Operative Treatment of Diaphyseal Humeral
Shaft Fractures. Hand Clinics 2007; 23(4): 437-448.
-
Court-Brown
CM, Garg A, McQueen MM. The translated two-part fracture of
the proximal humerus. J
Bone Joint Surg.2001;83-B(6):799-804.
-
Crates
J, Whittle AP. Antegrade interlocking nailing of acute
humeral shaft fractures. Clin
Orthop. 1998;(350):40-50.
-
Gregory
PR, Sanders R. Compression Plating versus intramedullary
fixation of humeral shaft fractures. J
Am Acad Orthop Surg. 1997;5:215-223.
-
Gregory
P, Sanders R. Compression plating versus intramedullary
fixation of humeral shaft fractures. J
Am Acad Orthop Surg. 1997;5: 215-223.
-
Gustilo
R, Anderson J. Prevention of infection in the treatment of
one thousand and twenty-five open fractures of long bones:
retrospective and prospective analyses. J
Bone Joint Surg [Am]. 1976;58:453-458.
-
Ikpeme
J. Intramedullary interlocking nailing for humeral
fractures: experiences with the Russell-Taylor humeral nail.
Injury
1994;Sep(25):447-455.
-
Ingman
A, Waters D. Locked intramedullary nailing of humeral shaft
fractures: implant design, surgical technique and clinical
results. J
Bone Joint Surg [Br]1994; 76-B:23-9.
-
Lin
J, Hou S. Locked nailing of severely comminuted or segmental
humeral fractures. Clin
Orthop and Rel Res 2002;406,195-204.
-
McCormack
R, Brien D, Buckley R et al. Fixation of fractures of the
shaft of the humerus by dynamic compression plate or
intramedullary nail: a prospective, randomised trail.
J Bone Joint Surg [Br] 2000; 82,Iss 3; 336-340.
-
Modabber
M, Jupiter J. Operative management of diaphyseal fractures
of the humerus: plate versus nail. Clin.
Orthop 1998;347:93-104.
-
R
Development Core Team (2006). R: A language and environment
for statistical computing. R Foundation for Statistical
Computing, Vienna, Austria. ISBN 3-900051-07-0.
-
Remiger
A, Miclau T, Lindsey R, Blatter G. Segmental avascularity of
the humeral diaphysis after reamed intramedullary nailing. Journal
of Orthop Trauma 1997;Vol 11(4):308-314.
-
Ruedi
T, Murphy W et al. (2000). Principles of Fracture
Management. Davos: AO Publishing & Stuttgart New York:
Georg Thieme Verlag.
-
Sarmiento
A, Kinman P, Galvin E et al. Functional bracing of the
humerus. J
Bone Joint Surg [Am] 1977;59-A:596.
-
Stannard
J, Harris, McGwin G, Volgas D, Alonso J. Intramedullary
nailing of humeral shaft fractures with a locking flexible
nail. J
Bone Joint Surg. 2003; 85: 2103-2110.
-
Stata
9.2. Copyright 1984-2006. Statistics/Data Analysis Stata
Corp, 4905 Lakeway Drive, College Station, Texas 77845. USA
(800-STATA-PC) http://www.stata.com 979-696-4600, stata@stata.com.
-
Webb
J. Distal humeral factures in adults. J
Am Acad Orthop Surg.1996;4:336-344.
-
Yang
K. Helical plate fixation for treatment of comminuted
fractures of the proximal and middle one-third of the
humerus. Injury
2005;36:75-80.
|