|
Abstract:
Chronic
inflammatory demyelinating polyneuropathy (CIDP) is a
neurological disease affecting peripheral sensory and motor
neurons about 2 per 100,000 adults.
We present a case of a woman with CIPD who underwent
total knee arthroplasty and her postoperative course was
complicated by a severe life threatening exacerbation of her
neurologic condition. She required intubation and respiratory
support in an intensive care unit before recovering post IV
immunoglobulin and steroid treatment. Based on this case, we
advocate preemptive dosing with either immunoglobulins or
steroids to minimise the risk of a potentially life threatening
exacerbation of CIPD post elective surgery.
J.Orthopaedics 2009;6(2)e12
Keywords:
Chronic inflammatory demyelinating polyneuropathy; CIDP; total knee replacement; TKR
Introduction:
We
present a case report of a woman with severe osteoarthritis and
a chronic inflammatory demyelinating polyneuropathy. She
underwent arthroplasty and her postoperative course was
complicated by a severe life threatening exacerbation of her
neurologic condition. Treatment with emergent respiratory
support, intravenous immunoglobulins and corticosteroids was
successful.
Case
Report:
A
74-year-old lady presented to an orthopaedic surgeon with
complaints of severe pain due to osteoarthritis of her right
knee. She
had a past history of chronic inflammatory demyelinating
polyneuropathy.
A
neurologist had been consulted 3 years prior, because of the
appearance of sensory disturbances in her fingers and toes, and
impaired balance. Her
sensory symptoms had gradually worsened over several years. A
previous urinary tract infection and an episode of
diverticulitis had both led to transient exacerbation of
symptoms. Post these illnesses she suffered multiple falls and
noted proximal leg weakness, needing a walking frame to mobilise.
Once these episodes had resolved, she regained strength and was
able to discard the walking aid.
Apart from osteoarthritis and the above recent health
events, her past medical history included mild hypertension,
controlled ischemic heart disease and gastroesophageal reflux.
Her
initial neurological examination revealed evidence of a motor
and sensory polyneuropathy. Her gait was slightly ataxic. There
was slight ptosis on the right, otherwise a normal cranial nerve
examination. Wasting
and weakness was noted in the thenar, hypothenar and
interosseous muscles bilaterally. Her toes were slightly clawed
and she had prominent plantar arches. Upper limb reflexes were
present but knee and ankle jerks were absent. The Babinski test
was negative bilaterally. Sensation to pin prick, light touch
and vibration was impaired in a glove and stocking distribution.
There was evidence of dyscoordination with inaccurate “finger
to nose” and “heel-knee-shin” tests.
Her
screening electrolyte and haematologic blood tests were
unremarkable. Nerve conduction studies showed that there was
evidence of peripheral neuropathy, with velocity in the
demyelinating range (range 29 – 39M/s).
She
began treatment with a course of intravenous immunoglobulins (Intragam®,
0.4g per Kg), which led to a significant clinical improvement.
Her balance and strength improved, she was walking normally and
her sensation to her fingers and toes returned. Attempts were
made to wean from the Intragam®, however she had a chronically
relapsing clinical course and required monthly dosing to control
the disease.
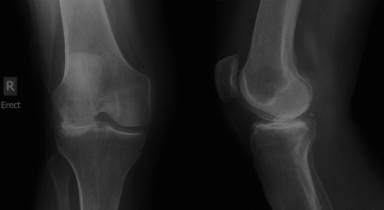
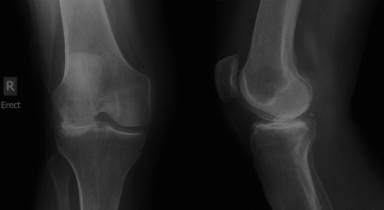
Assessment
and investigation by the orthopaedic surgeon revealed severe
degenerative joint disease of the right knee. As her pain was
insufficiently relieved by analgesics and anti-inflammatories,
she elected to undergo right total knee replacement.
The
elective procedure went smoothly without any technical or
anaesthetic problems.
After the operation she had a severe flare of her CIDP.
She progressively developed slurred speech but no obvious
dystonia of her tongue or oropharyngeal muscles. Cranial nerves
were normal to examination. She had an intermittently flaccid
four limb paresis and her lower limb reflexes were absent.
Sensory examination was difficult and inconsistent.
Three
days post surgery she developed difficulty breathing and a
paradoxical respiratory pattern.
An arterial blood gas showed that she was hypoxic (60.9
mmHg) and hypocapnic (24.9 mmHg), with a negative base excess of
11.0 and a pH of 7.375.
She was not significantly anaemic and Troponin was
negative. A CT pulmonary angiogram was normal.
Unable to maintain spontaneous breathing, she was
transferred to the intensive care unit where she was sedated and
intubated. Nerve
conduction studies revealed a marked worsening of her peripheral
neuropathy (range 20 – 36M/s).
She was investigated for myasthenia gravis, with
acetylcholine receptor antibody of <0.20nmol/L.
Serum protein analysis showed a decreased total protein
57 g/L (n: 60 – 80g/L), albumin level of 27.5g/L (n: 35.0 –
50.0g/L) and a slight increase in Alpha 1 protein 4.6g/L (n: 1.0
– 3.0g/L).
She
was administered an Intragam® infusion (0.4g /kg) and commenced
on prednisolone 75mg daily.
She received a total of 12 doses of prednisolone. Her
symptoms recovered dramatically with return of strength in upper
and lower limbs and she was able to spontaneously and
independently breathe. She was extubated after four days and was
continued on a monthly infusion of Intragam®. Seventeen days
after her procedure she was discharged home. At six week review
she had returned to her pre-operative neurological status, had
achieved an excellent range of knee motion and was mobilising
satisfactorily.
Discussion :
Chronic
inflammatory demyelinating polyneuropathy (CIDP) is a
neurological disease affecting peripheral sensory and motor
neurons, causing progressive sensory loss and weakness,
secondary to a cellular and humoral autoimmune medicated
reaction towards peripheral nerve antigens1.
The prevalence is about 2 per 100,000 in adults with a
mean age of onset at around 47 years of age, increasing with age1.
The course of the disease can be monophasic, relapsing
(14%) or progressive (45%), over months or years 1,2.
Typical
clinical presentation is a symmetrical, proximal and distal
muscle weakness progressing for more than two months.
Pain, ataxia and facial weakness can also be encountered.
There are absent or diminished deep tendon reflexes,
signs of demyelination on nerve conduction studies, increased
levels of protein in cerebrospinal fluid (CSF) and nerve
biopsies show axonal demyelination3.
Differential
diagnosis include Guillain-Barré syndrome (GBS), inherited
demyelinating polyneuropathies, metabolic neuropathies
(associated with diabetes, uraemia acromegaly, amyloidosis and
hypothyroidism), paraneoplastic neuropathies, multifocal motor
neuropathy, neuropathies associated with IgM, IgG or IgA
monoclonal gammopathies, infections with the Human
immunodeficiency virus, Lyme disease or Hepatitis C, Sjögren’s
Syndrome and inflammatory bowel disease 1,2.
Diagnosis
is based on a widely used criteria set out by Saperstein et al.1
and the Inflammatory Neuropathy Cause and Treatment Group 1,
which incorporate clinical features and electrophysiological
studies. The
American Academy of Neurology also recommends obtaining CSF and
nerve biopsies to confirm the diagnosis. The fundamental
clinical features are the duration of symptoms and progressive
nature, extending for more than 2 months, differentiating this
condition from GBS.
There
is no definitive treatment in the current literature and a
positive response to treatment is achieved in 70% at best6.
Recognised and successful treatments for CIDP that are
currently being used are intravenous immunoglobulins, plasma
exchange and corticosteroids.
Other therapy includes immunosuppressive medications,
such as azathioprine, cyclophosphamide, cyclosporine, and
interferon therapy1.
The
occurrence of a sudden and life threatening neurologic
deterioration in a patient with inflammatory neuropathy
following arthroplasty (or other surgery) has to our knowledge
not been previously reported. A fluctuating but progressive
course is not uncommon in this condition. Despite considering
the possibility of a relapse associated with the surgery we
could find no reports of such in the published literature and
hence elected to proceed with surgery in a standard fashion. It
is conjectural as to whether preemptive dosing with either
immunoglobulins or steroids would have prevented the episode.
Given this near death experience for our patient we would
advocate preemptive treatment for individuals with CIDP coming
to elective surgery.
Reference :
-
Kieseier
BC, Kiefer R, Gold R, et al.
Advances in understanding and treatment of
immune-mediated disorders of the peripheral nervous system.
Muscle Nerve 2004; 30:131-156.
-
Mcleod JG, Pollard JD,
Macaskill P, Mohamed A, Spring P, Khurana V.
Prevalence of chronic inflammatory demyelinating
polyneuropathy in New South Wales.
Ann Neurol 1999; 46:910-913.
-
Bouchard C, Lacroix C, Planté,
et al. Clinicopathologic
findings and prognosis of chronic inflammatory demyelinating
polyneuropathy. Neurology
1999; 52(3):498-503.
-
McCombe PA, Pollard JD, McLeod JG.
Chronic inflammatory demyelinating
polyradiculoneuropathy.
A clinical and electrophysiological study of 92
cases. Brain
1987; 110:1617-1630.
-
Van Schaik IN, Winer JB, De Haan R, Vermeulen
M. Intravenous immunoglobulin for chronic inflammatory
demyelinating polyradiculoneuropathy. Cochrane Database Syst
Rev 2002;2:CD001797
-
Köller H, Kieseier BC, Jander S, et al. Chronic
Inflammatory Demyelinating Polyneuropathy.
N Engl J Med 2005; 352(13):1343-1356.
-
Saperstein DS, Katz JS,
Amato AA, et al. Clinical
spectrum of chronic acquired demylinating polyneuropathies. Muscle Nerve 2001;24:311-324.
-
Hughes R, Bensa S, Willison
H, et al. Randomized
controlled trial of intravenous immunoglobulin versus oral
prednisolone in chronic inflammatory demyelinating
polyradiculopathy. Ann
Neurol 2001;50:195-201
-
Kuntzer T, Radziwill AJ, Lettry-Trouillat R, et al. Interferon-beta1a in
chronic inflammatory demyelinating polyneuropathy. Neurology
1999;53:1364-1365.
|