|
Abstract:
Objective:
This study investigated the characteristics of spontaneous
osteonecrosis of the knee (SONK) in order to establish
appropriate surgical indications.
Materials and Methods:This is a retrospective study of 70
knees with SONK observed in our hospital, with an average
follow-up of 37.9 months after conservative treatment.
Results: The pain and functional scores of the subjects with
SONK significantly improved over the period. X-ray findings
worsened slightly, whereas limb alignment, size of necrosis, and
knee range-of-motion were stable. Of the cases that progressed
to higher X-rays stage during the follow-up period, 71.4% of
knees changed within 12 months of disease onset. Of the cases
that demonstrated stage III to IV at the first visit, 81.1% of
knees maintained the same stage at the final examination.
Conclusions
According to both observations, it seems reasonable to choose
conservative treatment for SONK, even if X-rays of the affected
knee reveal more than stage III severity.
J.Orthopaedics 2009;6(1)e6
Keywords:
knee; osteonecrosis; conservative treatment
Introduction:
Spontaneous
osteonecrosis of the knee (SONK) was first described in 1968
[1]. The
typical SONK patient is a woman over sixty years old who has
sudden onset of severe pain on the medial side of the knee which
often is related to a specific activity or a minor trauma. In
clinical situations, it is sometimes difficult to decide the
timing and indication of surgical treatment because SONK shows
variable prognoses [2-6]. Some cases need surgery because of
severe discomfort and joint deformity, while in others the
symptoms disappear a few months later and no joint deformity
occurs.
We aimed to clarify the characteristics of this disease and
establish an appropriate surgical indication. We hypothesize
that the progression of joint deformity is quite slow or in due
time reaches a plateau if the patient is responsive to
conservative treatment. In this study, we assessed
retrospectively the characteristics of subjects who successfully
continued conservative treatment for SONK.
Materials
and Methods:
We
retrospectively evaluated the natural history of 70 knees in 64
subjects (48 female, 16 male) with SONK, with an average
follow-up of 37.9 months (range 8 to 96). They were selected
from the patient list of our hospital from January 1998 through
December 2007 at their first visit. The average age was 68.9±8.5 years old and the average body mass index was 24.9±3.7
kg/m2. All subjects initially demonstrated positive
magnetic resonance imaging with a well-localized low signal
intensity lesion on T1-weighted images over the medial femoral
condyle that was diagnosed according to past reports [5,7] by
expert radiologists. None of the patients had a history of
cortisone consumption or any disease known to cause secondary
osteonecrosis. The time interval between the onset of symptoms
and the first visit was 13.0 months on average (range 0 to 60
months). All patients were encouraged to exercise the affected
knee at home (description in detail as below) and used a lateral
wedged sole to avoid mechanical overload to the medial
compartment of the knee. Only non-steroidal anti-inflammatory
drugs were used as pain rescue analgesics. The characteristics
of our subjects are summarized in Table 1.
|
Description
|
Total
subjects
|
Acute
group
|
Chronic
group
|
p
|
|
number of knees (subjects)
††
|
70
(64)
|
40
(38)
|
30
(26)
|
.443
|
|
men : women†
|
16
: 48
|
10
: 28
|
7
: 19
|
.815
|
|
age at the first visit ††
(y.o.: minimum to maximum)
|
68.9±8.5
(48
to 83)
|
70.9±6.4
(57
to 80)
|
65.5±10.3
(48
to 83)
|
.123
|
|
body mass index (kg/m2)
††
|
24.9±3.7
|
24.8±3.8
|
24.8±3.2
|
.960
|
|
time interval from the onset to the
first visit (month) ††
|
13.0
(0 to 60)
|
5.7±4.5
|
27.3±12.9
|
.000
|
|
follow-up period (month) ††
|
37.9
(8 to 96)
|
30.1±17.6
|
52.0±18.7
|
.000
|
|
site of necrosis
|
medial
femoral condyle in all cases
|
-
|
† Yates chi-square test
†† unpaired t-test
Table 1: Subject
characteristics
We recommended subjects perform the exercises as follows:
(1) isometric muscle exercises of the bilateral lower limbs, 1
set (each exercise done 20 times) of straight leg rising
training, and hip abduction and adduction exercises twice a day,
in the morning and evening. SLR exercise: Lying on the back,
raise the entire involved leg straight. Be sure to keep the
involved ankle 10 cm above the floor. Hold for 5 seconds, then
slowly lower. Hip abduction exercise: Lying on the uninvolved
side, slowly lift the involved leg straight out to the side to
the horizontal level. Hold for 5 seconds, then slowly lower. Hip
adduction exercise: Sitting on the edge of a table or a high
chair with the knees bent, squeeze an appropriately sized ball
between bended knees. Hold for 5 seconds, then slowly open.
(2) As a ROM exercise, maximum flexion and maximum
extension were performed twice a day in the morning and evening
after the knee was warmed (in a bath or shower). After
decreasing the pain and improvement in symptoms, we recommended
normal speed walking as much as possible to the subjects.
For the clinical and physical evaluation, three scales
that are usually used for osteoarthritis of the knee were used.
With the visual analogue scale (VAS) for pain, patients can
indicate their actual pain level using a 100-mm straight line as
a scale of pain. The JKOM (Japanese Knee Osteoarthritis Measure)
consists of 25 self-completion questionnaires with 4
subcategories: Pain and stiffness during activities of daily
living, social activities, and general health with 100 points as
the maximum score [8],
incorporating the concepts of the World Health
Organization’s International Classification of Functioning,
Disability and Health (ICF 2004) [9]. The (Japan Orthopaedics
Association) JOA score reflects the treatment criteria of the
Japanese Orthopaedic Association, which is used by physicians
for subjective evaluation of sub-categories: pain during
walking, pain when using stairs, range of motion, and swelling,
with 100 points set as the full score [10]. Clinical findings,
as active range of motion (ROM; maximum extension and flexion in
degrees) measured by an orthopaedic goniometer and swelling of
the affected knee in three degrees, non=0, mild=1, moderate or
more=2, were also recorded at the same time.
The radiographic evaluation was also assessed.
Weight-bearing anteroposterior X-rays of the tibiofemoral joint
using the standing extended view (also known as the standing
anteroposterior view) were taken to measure the femorotibial
joint space width (JSW) as the degree of joint deformity [11].
JSW was determined at the center point of the medial
femorotibial compartment on a radiograph using a 0.1-mm
graduated magnifying lens. In order to obtain acceptable X-rays
for accurate reading, we decided to take X-rays according to the
Buckland-Wright criteria [12] in which inter-margin distance (IMD)
of the medial tibial plateau fell within 1 mm. If the IMD was
over 1 mm, another X-ray was taken up to three times. If we
failed to obtain an X-ray within 1 mm of IMD from the three
X-rays, we adopted the X-ray of the least IMD. The femorotibial
angle (FTA) as a parameter of limb alignment was also measured
according to the method of Moreland et al. [13]. In the plane
X-ray examination, we determined X-ray stage according to
Agliatti et al. [2], and also simply assessed the occupied ratio
(OR) of the osteonecrotic lesion in the standing anteroposterior
view because exact measurement of the lesion was sometimes
difficult, especially in the lateral view. In cases of early
SONK with stage I that represented no radiographic abnormality,
magnetic resonance imaging of the affected knee was also used to
measure this ratio instead. All radiographs were obtained by an
experienced expert technician and quantified by a single reader
who was blinded to the features of the subjects.
Statistical
analysis
Seventy knees in 64 SONK subjects were included in the analyses.
Changes in factors including JKOM, VAS, JOA, ROM, JSW, FTA,
X-ray stage, and OR from the first visit to the final status of
follow-up were assessed using a paired t-test for parametric
data, or Wilcoxon’s signed ranks test for other data.
It could not be ignored that our subjects had various time
intervals from the onset to the first visit, and this appeared
to affect their clinical course. Therefore, for analysis we
divided subjects into two groups so as to divide the population
close to equal distribution as follows: One was the acute or
subacute group (n=40) of subjects who visited within 12 months
from the disease onset, and the other was the chronic group
(n=30) of subjects who visited later than 12 months. The
characteristics of all subjects and each group are summarized in
Table 1. The gender difference was estimated by chi-square test,
and other factors were compared using the unpaired t-test. There
was no difference between the both groups except for time
intervals from disease onset and follow-up period.
Linear mixed model analysis was also devised to address the
effect of inter-group and longitudinal course on the eight above
factors. This method
provides the most reliable results as it uses all available data
to estimate the dependent variables. Subjects with at least 8
months’ follow-up were selected for analysis from the
complete, longitudinal dataset. Time intervals from the
first visit through the examination were divided into five
categories as follows; the first visit, less than 12 months from
the first visit, 12 to less than 36 months, 36 to less than 54
months, 54 months or more.
The estimations were made by using 267 observations from 70
subjects. A P value of <.05 was considered significant
and all tests were two sided. All data analyses were conducted
with SPSS for Windows, version 16.0J (SPSS Inc., Chicago, IL,
USA).
Results:
Pain
and functional scores of the affected knee with JKOM, JOA, and
VAS initially were 34.1, 70.0, and 50.5 on average, respectively
(Table 2). The scores at the final follow-up examination were
22.7, 82.1, and 32.3, and the differences were statistically
significant (P<.01) from the first visit. For radiographic
evaluations, there were also significant differences regarding
JSW and X-ray stage between the first visit and the last
follow-up examination, while OR, FTA and ROM demonstrated no
differences. In the acute group, there were significant
differences between the first and last examinations regarding
JKOM, JOA, VAS, and X-ray stage, whereas no such differences
were seen in the chronic group regarding JOA, VAS, or X-ray
stage.
|
|
Total
subjects (n=70)
|
Acute
group (n=40)
|
Chronic
group (n=30)
|
|
|
first
visit
|
last
observation
|
p
|
first
visit
|
last
observation
|
p
|
first
visit
|
last
observation
|
p
|
|
ROM (degree) ††
|
131.0±16.1
|
132.9±18.7
|
.126
|
131.8±13.0
|
134.8±14.0
|
.189
|
125.3±24.1
|
127.7±27.0
|
.429
|
|
VAS (0-100) †
|
50.5±23.9
|
32.3±27.1
|
.003
|
51.0±20.6
|
33.5±29.3
|
.005
|
41.1±23.2
|
34.5±25.4
|
.325
|
|
JOA (0-100) †
|
70.0±15.5
|
82.1±15.4
|
.000
|
67.8±15.3
|
82.2±16.5
|
.000
|
77.7±14.3
|
81.6±13.6
|
.277
|
|
JKOM (0-100) †
|
34.1±18.3
|
22.7±17.7
|
.000
|
36.4±17.2
|
22.3±18.9
|
.002
|
26.6±14.0
|
18.9±13.0
|
.006
|
|
X-ray stage [2]
(1,2,3,4,5) ††
|
2.9±1.1
|
3.3±.9
|
.000
|
2.6±1.0
|
3.2±.8
|
.000
|
3.2±1.0
|
3.4±.9
|
.102
|
|
occupied ratio (%) ††
|
30.0±15.3
|
32.5±12.8
|
.830
|
29.8±17.1
|
32.7±13.8
|
.433
|
32.0±11.8
|
31.7±12.0
|
.345
|
|
JSW (mm) †
|
2.8±1.2
|
2.6±1.1
|
.014
|
2.8±1.2
|
2.6±1.2
|
.074
|
2.8±1.3
|
2.5±1.0
|
.060
|
|
FTA (degree) ††
|
180.7±4.2
|
181.7±9.8
|
.310
|
180.2±3.8
|
179.0±3.8
|
.276
|
181.5±5.4
|
181.4±4.9
|
.799
|
†
paired t-test
†† Wilcoxon’s signed
rank test
ROM: range of motion, VAS: the visual analogue scale, JOA: the
Japan Orthopaedics Association score, JKOM: the Japanese Knee
Osteoarthritis Measure, JSW: joint space width of the affected
condyle, FTA: the femorotibial angle
Table
2: Differences in variables between the first visit and the
final follow-up
The
changes in the X-ray stage from the first visit through the
final observation are summarized in Table 3, which includes the
cases for whom follow-up periods were at least 12 months. Of 21
cases that progressed to the higher X-ray stage during the
period, 15 knees (71.4%) changed within 12 months of disease
onset. Of 37 cases that demonstrated stage III to IV on the
X-ray at the first visit, 30 knees (81.1%) maintained their
stage level at the final examination.
|
X-ray
stage
|
stage
at the last examination*
|
|
I
|
II
|
III
|
IV
|
V
|
|
stage
at the first visit
|
I
(n=7)
|
1
|
3
|
3
|
|
|
|
II
(n=13)
|
|
5
|
6
|
2
|
|
|
III
(n=24)
|
|
|
18
|
6
|
|
|
IV
(n=13)
|
|
|
|
12
|
1
|
|
V
(n=3)
|
|
|
|
|
3
|
Sixty
subjects with at least 12months’ observation period are
summarized.
* 38.5 months on average (range 12-96).
Table 3:Changes in X-ray staging between the first visit and the
last examination.
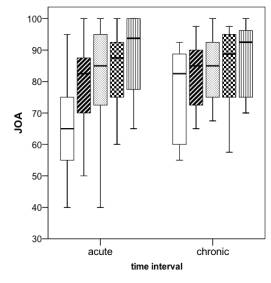
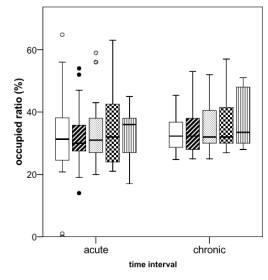
There was no difference in the inter-group analysis regarding
all dependent variables in linear mixed model analysis (Figure
1, Table 4). These
analyses also revealed that VAS, JKOM, JOA, JSW and X-ray stage
changed significantly with time, even in the chronic group. This
means that time intervals are significant to improve of
the functional scores of VAS, JKOM, and JOA. JSW and X-ray stage
worsened slightly, whereas FTA, OR and ROM were unchanged in
each group.
|
Dependent
variables
|
Fixed
effects
|
|
group†
|
time†
|
time*group
|
|
ROM (degree)
|
.128
|
.361
|
.770
|
|
VAS (0-100)
|
.868
|
.015
|
.178
|
|
JOA (0-100)
|
.687
|
.000
|
.053
|
|
JKOM (0-100)
|
.559
|
.000
|
.208
|
|
radiographic stage [2]
(1,2,3,4,5)
|
.195
|
.000
|
.149
|
|
occupied ratio (%)
|
.888
|
.448
|
.618
|
|
JSW (mm)
|
.817
|
.002
|
.233
|
|
FTA (degree)
|
.568
|
.781
|
.490
|
† Univariate
Test.
This test is based
on linearly independent pairwise comparisons among the estimated
marginal means.
ROM: range of motion, VAS: the visual analogue scale, JOA: the
Japan Orthopaedics Association score, JKOM: the Japanese Knee
Osteoarthritis Measure, JSW: joint space width of the affected
condyle, FTA: the femorotibial angle
Table
4 Fixed
effects in the linear mixed model analysis
Typical cases of SONK with conservative treatment are shown in
Figure 2 and 3. A 72 y.o. woman had severe knee pain with acute
onset, scoring 45 on VAS, 54 on JKOM, and 70 on JOA (Figure 2).
She visited our hospital 5 months after the disease onset.
X-rays revealed typical characteristics of stage III SONK and
she was treated conservatively with home exercise and protected
from excess weight bearing. Three
months after the first visit, she complained of
intense knee pain with a VAS score of 90 and requested surgical
treatment. We planned surgical treatment for the affected knee,
but she could not undergo surgical treatment immediately due to
her family reasons. Nine months after the first visit, her pain
decreased gradually, although X-rays showed progression to stage
IV. At the last observation, symptoms had almost resolved and
X-rays showed no progression. She could climb a slope, fold
her legs under herself in the Japanese style ‘seiza’,
and even run a short distance without pain. Scores at the last
examination were 20 on VAS, 11 on JKOM, and 90 on JOA. The OR
was 37.4% and JSW was 2.1 mm at the last observation (-0.8mm
compared to that of the first visit).
Another case of SONK belonged to the chronic group. An 83
y.o. woman who had severe pain with sudden onset 18 months
earlier and was treated at another hospital followed by our
hospital with continued pain, scored 40 on VAS, 30 on JKOM, and
85 on JOA at her first visit (Figure 3). X-rays revealed typical
characteristics of stage III SONK and she was treated
conservatively with home exercise and protected from excess
weight bearing. Twenty-four months after the first visit at the
last observation, symptoms almost resolved and X-rays showed no
progression and slight sclerotic changes. She could climb a
slope and even run a short distance without pain. Scores at the
last examination were 10 on VAS, 9 on JKOM, and 100 on JOA. The
OR was 42.5% and JSW was 4.0 mm at the last observation (no
change from that of the first visit).
A.  |
B.  |
|
Figure 3.
An 83-year-old woman had sudden onset of medial pain in
the right knee. A. Plain radiographs after 18 months
demonstrated a radiolucent area of the medial femoral
condyle that appeared to be stage III SONK, scoring 40 on
VAS, 30 on JKOM, and 85 on JOA. B. After 24 months:
Symptoms had almost resolved and X-rays showed no
progression and slight sclerotic change. Scores at the
last examination were 10 on VAS, 9 on JKOM, and 100 on JOA.
The OR was 42.5% and JSW was 4.0 mm at the last
observation. |
Discussion:
Since
Ahlbach’s first description of SONK in 1968 [1], there have
been many published data concerning its clinical prognosis and
it is well known that the clinical course of this disease varies
from remission with conservative treatment to severe dysfunction
requiring surgical treatment [14].
In the cases of early SONK of stage I that shows no radiographic
abnormalities, there are several reports of a benign prognosis
with conservative treatment [7,15,16]. Yates et al. [16]
described 20 sequential
cases of early SONK diagnosed by magnetic resonance imaging (MRI)
in which non-operative management led to the spontaneous
resolution of symptoms and MRI changes at an average of
4.8 months after disease onset.
In our study, most of the stage I cases changed to a
higher stage at the last examination. It is possible that we
missed early stage SONK by omitting of magnetic resonance image
or radioisotope examination in our outpatient department. There
were some attempts to predict the prognosis of SONK in past
reports [7, 17]. It is worth noting that Locouvet et al. [7]
demonstrated that predictive data for irreversible osteonecrosis
by means of MR images was a subchondral low signal on T2 of
>4 mm depth or >14 mm long, focal epiphyseal contour
depressions and low signal lines deep in the affected condyle.
Regarding stage II or higher stages when these radiographic
findings are visible on X-rays, the clinical course and
prognosis were reported to depend on the radiographic size of
the lesion [2,18,19,20]. In these reports, several authors noted
that when a more than 50% of the occupied ratio of the lesion,
and more than 5 cm square of the lesion area, the patient had a
poor clinical and radiographic prognosis with rapid development
of osteoarthritis and surgical treatment was recommended. In
this study, we retrospectively evaluated SONK subjects who were
successfully treated without surgical treatment over the past
ten years. There was no discrepancy between the past reports and
our findings that revealed a 32.5% lesion occupied ratio and
181.7 degrees of FTA on average at the final evaluation (37.9
months’ observation period on average). Aglietti et al.,
suggested other factors that worsened prognosis. They were
flexion contracture and extent of local swelling [2], and our
results were also consistent with these findings. In seventy
knees with SONK, non of the knees represented severe contracture,
and only 4 knees had swelling, scoring 1 in three knees and 2 in
one knee at the final observation. Of these knees, the case with
severe swelling (score=2) had worse symptoms and ROM, but not in
terms of X-ray stage, which consistently showed stage 4 (data
not shown in the results).
The difference between the first visit to the last observation
regarding the eight examined factors in the acute group tended
to be much clearer compared with that of the chronic group
(table 2). The two-comparison analyses (paired
t-test and Wilcoxon
signed rank test) revealed that changes in VAS, JOA, ROM and
X-ray stage were significant only in the acute group.
In our conservatively treated subjects with SONK, however,
linear mixed model analyses revealed that pain and function
gradually improved, JSW and X-ray stage barely progressed, and
no malalignment or joint contracture was seen, regardless of the
time interval from disease onset to the first visit. In
addition, it appears that the improvements in pain and
functional scores were rapid within a year from the disease
onset, although the differences were not significant between the
groups. After that period, the symptoms became stable and joint
deformity tended to be unchanged or remained at a plateau in our
selected population.
Among 60 subjects with SONK who were followed up for at least 12
months, the change in the X-ray stage from the first visit
through the final observation reveals that 71.4% of knees
(15/21) progressed to the higher stage within 12 months from
disease onset (Table 3). Also 81.1% (30/37) of knees with stage
III to IV on X-rays at the first visit maintained the same stage
until the final examination. According to both observations, it
seems reasonable to choose conservative treatment for SONK, even
if X-ray of the affected knee reveals greater than stage III
severity.
In clinical situations, the timing of surgical treatment for
SONK remains controversial. For younger SONK patients with
severe malalignment, proximal tibial osteotomy is preferred in
most cases, while for elderly SONK patients with secondary
osteoarthritis, total knee arthroplasty may be the first choice.
Unicompartmental replacement can be considered for patients with
single compartment involvement and no degenerative changes in
the opposite compartment in the femorotibial joint.
In the early stage, Koshino [14] concluded that bone grafting or
drilling into the necrotic lesion are effective in promoting
osteonecrosis healing, and surgery should be performed in the
early stages of the disease (before the onset of degenerative
changes) to obtain maximum clinical and radiographic
improvement. It remains unclear when surgical treatment is
indicated; the timing depends on whether degenerative changes
have progressed to represent varus knee, an earlier stage of
SONK, or severe impediment of activity of daily living
regardless of these stages.
Although it is clear that there are cases who need surgical
intervention and cases without progression of joint deformity.
Therefore, we think it important to consider the natural course
of SONK under conservative treatment to avoid unnecessary
surgery. Our findings suggest that surgical treatment may not be
the first choice even if symptoms are severe at the first visit,
especially within 12 months, or radiographic examination
demonstrates stage III or later X-ray characteristics. Our
recommended home-based exercise is effective for SONK to
maintain good condition.
There are several limitations to this study as follows. First,
surgical treatment cases were excluded from this study and were
not compared with the present subjects, so we could not show the
cumulative survival rate of SONK with conservative treatment.
Second, a 3-year follow-up period on average may not be
enough to evaluate the prognosis of SONK, and some of our
subjects may undergo surgery in the future.
Third, the term ‘12-months’ from the disease onset in this
study was merely a convenient way to divide subjects into 2
groups according to equal deviation. It is necessary to
calculate an accurate ‘safety’ period cut-off value so the
ROC curve or survival rate can be computed together with cases
of surgical intervention. Another study is required to explore
these issues.
Although there are several limitations as described above, this
study reveals relevance of conservative treatment for SONK.
Further study is needed to explore the accurate timing of
surgical treatment.
Conclusion:
The
70 knees receiving conservative treatment for SONK was
retrospectively assessed. Most cases demonstrated that changes
in the functional scores were correlated with the time interval
from the disease onset, while the radiological aspects did not
progress in the 3 year follow-up period. It appears that
conservative treatment in useful to alleviate SONK symptoms, if
it is over 12-months from disease onset, even if X-rays of the
affected knee reveal greater than stage III severity.
Reference :
-
Ahlbäck
S, Bauer GCH, Bohne WH. Spontaneous osteonecrosis of the
knee. Arthritis Rheum 1968; 11: 705-33.
-
Aglietti
P, Insall JN, Buzzi R, Deschamps G. Idiopathic osteonecrosis
of the knee. Aetiology, prognosis and treatment. J Bone
Joint Surg Br 1983; 65: 588-97.
-
Lotke
PA, Ecker ML. Current concept review. Osteonecrosis of the
knee. J Bone Joint Surg Am 1988; 70: 470-3.
-
Björkengren
AG, Al-Rowaih A, Anders L, Thorngren K, Pettersson H.
Spontaneous osteonecrosis of the knee: Value of MR imaging
in determining prognosis. AJR 1990; 154: 331-6.
-
Motohashi
M, Morii T, Koshino T. Clinical course and roentgenographic
changes of osteonecrosis in the femoral condyle under
conservative treatment. Clin Orthop Related Res. 1991; 266:
156-161.
-
Levcouvet
FE, van der Breg BC, Maldague BE, Lebon CJ, Jamart J, Saleh
M, et al. Early irreversible osteonecrosis versus transient
lesions of the femoral condyles: prognostic value of
subchondral bone and marrow changes on MR imaging. Am J
Roentgenol 1998; 170: 71–7.
-
Akai
M, Doi T, Fujino K, Iwaya T, Kurosawa H, Nasu T. An Outcome
Measure for Japanese People with Knee Osteoarthritis. J
Rheumatol 2005; 32: 1524-32.
-
World
Health Organization. International classification of
functioning, disability and health. Geneva: World Health
Organization 2004. http://www.who.int/classifications/icf/en/
-
Koshino
T, Saito T, Wada J, Akamatsu Y. New design of TKA;
unicompartmental arthroplasty for osteoarthritis of the knee
using the ceramic YMCK model. In: Niwa S, Yoshino S,
Kurosawa M, Shino K, Yamamoto S eds. Reconstruction of the
Knee Joint. Berlin: Springer, 1997: 200–206.
-
Ravaud
P, Auleley GR, Chastang C, Rousselin B, Paolozzi L, Amor B,
et al. Knee joint space width measurement: an experimental
study of the infl uence of radiographic procedure and joint
positioning. Br J Rheumatol 1996;35:761–6.
-
Buckland-Wright
JC, Macfarlance DG, Williams SA, Ward RJ. Accuracy and
precision of joint space width measurements in standard and
macroradiographs of osteoarthritic knees. Ann Rheum Dis
1995;54:872-880
-
Moreland
JR, Bassett LW, Hanker GJ. Radiographic analysis of the
axial alignment of the lower extremity. J Bone Joint Surg Am
1987; 69: 745-9.
-
Koshino
T. The treatment of spontaneous osteonecrosis of the knee by
high tibial osteotomy with and without bone-grafting or
drilling of the lesion. J Bone Joint Surg Am 1982; 64:
47-58.
-
Lotke
PA, Ecker ML, Alavi A. Painful knees in older patients.
Radionuclide diagnosis of possible osteonecrosis with
spontaneous resolution. J Bone Joint Surg Am 1977; 59:
617-21.
-
Yates PJ,
Calder JD, Stranks GJ, Conn KS,
Peppercorn D, Thomas NP.
Early
MRI diagnosis and non-surgical management of spontaneous
osteonecrosis of the knee. Knee 2007; 14: 112–116.
-
Mont
MA, Baumgarten KM, Rifai A, Bluemke DA, Jones LC, Hungerford
DS. Atraumatic osteonecrosis of the knee. J Bone Joint Surg
Am 2000; 82–9:1279–90.
-
Muheim
G, Bohne WH. Prognosis in spontaneous osteonecrosis of the
knee: investigation by radionuclide scintimetry and
radiography. J Bone Joint Surg Br 1970; 52: 605-12.
-
Rozing
PM, Insall J, Bohne WH. Spontaneous osteonecrosis of the
knee. J Bone Joint Surg [Am] 1980; 62: 2–7.
-
Lotke
PA, Abend JA, Ecker M L. The treatment of osteonecrosis of
the medial femoral condyle. Clin Orthop 1982; 171: 109-16.
|