| CASE
REPORT |
|
Fulminating Fatal Paradoxical Fat Embolism Without Cardiac Septal
Defect - Clinical And Histopathological Features |
|
Seetharaman Hariharan*,Chalapathi
Rao AdidamVenkata
*Faculty of Medical Sciences ,
The University of the West Indies, St Augustine,
Trinidad and Tobago
Address for Correspondence:
Seetharaman Hariharan,
Senior Lecturer
Department of Clinical Surgical Sciences
Faculty of Medical Sciences
The University of the West Indies
Eric Williams Medical Sciences Complex
Mount Hope, TRINIDAD (West Indies)
Telephone/Fax: 1 868 662 4030
E-mail: uwi.hariharan@gmail.com
|
|
Abstract:
Paradoxical fat embolism involving multiple
organs is usually reported to have been associated with cardiac
defects such as patent foramen ovale. We report a case of fat
embolism syndrome following unilateral femoral and bimalleolar
fracture, which rapidly progressed to death. The patient did not
satisfy the required Gurd’s criteria to diagnose fat embolism
syndrome clinically. At autopsy, the patient did not have any
cardiac septal defects or arteriovenous malformations. But fat
deposition could be demonstrated histopathologically in many
organs. The increase in the pulmonary vascular resistance would
have opened the physiological anastomoses between the pulmonary
arteries and veins, leading to massive embolisation of fat into
the left side of the heart and dissemination to other organs.
This patient did not receive PEEP during his mechanical
ventilation which could have possibly physically prevented
embolisation through the arteriovenous shunts. Massive
paradoxical fat embolism can occur without a cardiac septal
defect. Fat embolism syndrome should be suspected even when a
patient does not satisfy the Gurd’s criteria.
J.Orthopaedics 2008;5(4)e8
Introduction:
Fat embolism syndrome is characterized by
symptoms and signs involving the respiratory, haematological,
dermatological and neurological systems (1). Paradoxical fat
embolism is commonly reported after orthopaedic surgeries such
as hip arthroplasty and placement of intramedullary rods (2-4).
It has also been proposed as a cause of postoperative
neurocognitive dysfunction and persistent unconsciousness after
anaesthesia following orthopaedic surgery (5, 6). Massive
paradoxical fat embolism has been usually reported to be
associated with cardiac defects such as Patent Foramen Ovale (PFO)
(7, 8). We report a patient with no such
abnormality, and had fat deposition in many
organs and rapidly progressed to death.
Case Report :
A
20-year-old otherwise healthy man sustained a closed comminuted
fracture involving the mid-shaft of the right femur and bi-malleolar
fractures of left ankle following motor vehicle accident. He was
initially taken to a primary health centre and after a two-hour
wait was transferred to a tertiary care centre. Because the
patient was dissatisfied with the care he received in this
hospital, he discharged himself in 12 hours and got admitted to
another tertiary care centre. He was placed on tibial-pin
traction. 24 hours following the fracture, while on the
orthopaedic ward he developed tachypnoea; the pulse oximeter
reading showed 94-95% oxygen saturation. At this point of time,
he was fully conscious and orientated, there were no petechial
spots on the skin, and his haematological and biochemical
parameters were completely within the normal range. His chest
radiograph did not show any changes. He was given oxygen
supplementation by facemask and later by Venturi devices
increasing the FiO2 until 60%. However, in a six-hour
period, his tachypnoea and hypoxaemia worsened. He also had
confusion at this point, which was attributed to his hypoxaemia
(pulse oximeter showed 89-90% saturation). He had tachycardia in
the range of 110-120 beats per minute. He was endotracheally
intubated and was awaiting Intensive Care Unit (ICU) admission,
hand ventilated by a physician. Patient was later provided
mechanical ventilatory support in an operating room by an
anaesthetic ventilator, where his condition worsened. He had a
severe hypoxaemia (PaO2 of 52 mmHg with a FiO2
of 100%), but a normocarbia. He required noradrenaline infusion
to maintain the mean arterial pressure. Even at this
stage he did not have a low haematocrit, thrombocytopaenia or
leucocytosis. He did not have any cutaneous petechial spots.
However, he developed anuria and the renal biochemical
parameters started to rise. He had adequate volume replacement
guided by the central venous pressure but did not receive blood
transfusion. Dobutamine infusion was started along with the
noradrenaline because of a low value of the central venous
oxygen saturation. He was continued to be ventilated in the
operating room with the anaesthetic ventilator. 48 hours after
the trauma, a CT scan of the head along with a spiral CT of the
pulmonary vessels was requested and he was transported to the
radiology suite. He had a cardiac arrest on the CT scan table
and could not be successfully resuscitated.
An
autopsy was performed, which revealed the following findings:
There
was a closed comminuted fracture of the mid-shaft of right femur
with haematoma (200 ml). Bimalleolar fractures of left ankle
with swelling and contusions were present. Cyanosis was present
but skin petechiae were absent. Bronchial lumen contained
haemorrhagic frothy fluid. Pleural surface of lungs had
petechiae. Both the lungs were heavy (> 1000 g), congested and
had patchy haemorrhagic areas. Right pleural cavity contained
300 ml of straw-coloured fluid.
Histology of lung revealed clear spaces within blood vessels
with displacement of red blood cells, parenchymal haemorrhages,
focal pneumonic changes, and fibrinous material in the air
spaces.
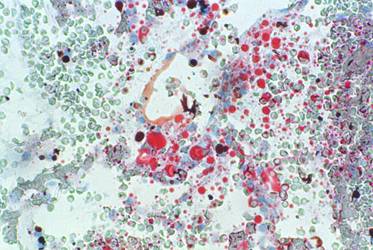
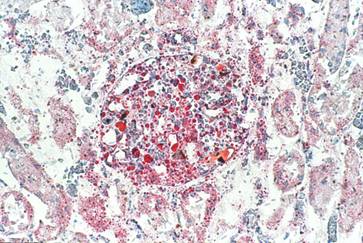
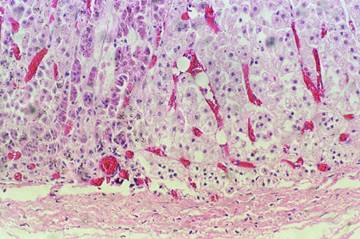
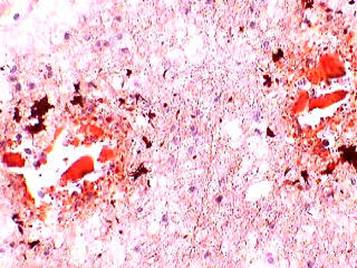
Most
organs (lungs, brain, kidney, spleen and liver) revealed
congestion and clear vacuoles in the blood vessels. Frozen
section and Oil red O staining of lungs, kidneys, adrenals and
brain showed fat deposition with foci of inflammatory response
(Figures 1-4).
There
was no evidence of PFO or any other cardiac septal defects, and
there was no evidence of arteriovenous malformations in any
organs studied.
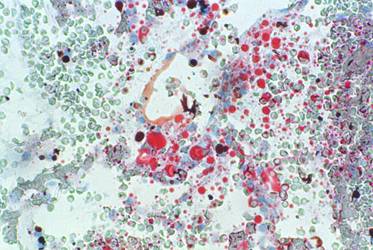
Figure 1: Frozen section of the lung stained with oil red O
showing multiple orange red fat globules of varying sizes in the
septal vasculature
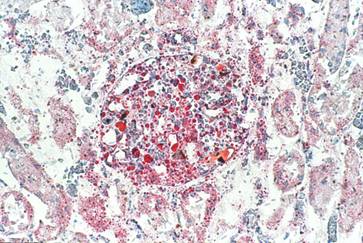
Figure 2: Frozen section of the kidney stained with oil red
O showing multiple orange-red fat globules of varying sizes in
the glomerular capillaries
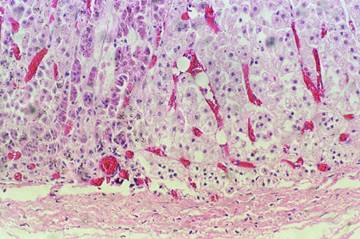
Figure 3: Section from the adrenal gland showing cortical
distended capillary containing clear refractile fat vacuoles
(H&E, ×20)
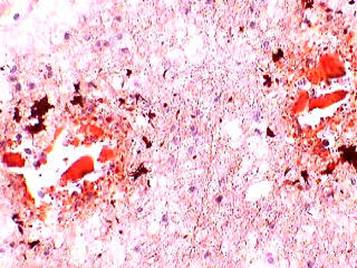
Figure 4: Frozen section of brain tissue stained with oil
red “O” reveals fat globule in the lumen of blood vessel (10×)
Discussion :
Although
fat embolism syndrome is commonly reported in the literature,
there are few reports which have histopathologically
demonstrated the presence of fat in multiple organs. A recent
histopathological report demonstrated fat in the lungs; however
this was an artificial lung used for resuscitation of the
patient (9).
Fat
embolism syndrome is predominantly a clinical diagnosis.
Radiological and laboratory findings are mostly inconsistent and
nonspecific (10). The diagnosis may be assisted by employing the
Gurd’s criteria, which include both clinical and laboratory
parameters (11). At least one major criterion and two minor
criteria should be satisfied to establish the diagnosis of fat
embolism. However, in the present case, the only major criterion
to be satisfied was hypoxaemia and the only minor criterion was
tachycardia. Despite this, the patient had a fatal fat embolism
and the autopsy showed systemic fat deposition.
Multi-organ dysfunction syndrome (MODS) can be
associated with Acute Respiratory Distress Syndrome, which is a
common sequel to fat embolism (12). However, this is usually
common in trauma involving multiple anatomical regions and the
post-mortem findings of MODS is found when the patient dies
after 72 hours (12). In the present case, the patient died in 48
hours following an isolated femoral and bimalleolar fracture
with no other co-morbidities or cardiac abnormalities.
Reports in the literature have suggested the
possibility of systemic fat embolisation through pulmonary
capillaries, although this is on the basis of animal studies
(13, 14). An earlier report which demonstrated the presence of
veno-arterial shunts in the brain by Transcranial Doppler (TCD),
proposed these shunts as a possible explanation for paradoxical
cerebral fat embolism following orthopaedic surgeries (15). The
study reported that some of the cerebral emboli were spontaneous
and many required ‘provocation’ such as Valsalva manœuvre. The
authors also opined that the small and delayed emboli through
pulmonary arteriovenous shunts may be clinically insignificant
(15). But the question remains that when the systemic arterial
pressure is at a higher level than the venous pressure, how does
large amount of fat get into the systemic arterial side in
various organs to cause a massive paradoxical fat embolism?
Intrapulmonary arteriovenous shunts are known
to be dormant in healthy humans, which could be recruited in
certain conditions such as physical exercise (16). In the
present case, the increased pulmonary vascular resistance caused
by the pulmonary fat embolism would have opened the
physiological pulmonary arteriovenous shunts. The higher
pressure in the pulmonary arterial network relative to the
pulmonary venous network would have assisted this massive
embolisation to the left side of the heart and eventually to all
the other organs. Although there is proposal of the mechanical
theory of fat embolism (17), the feasibility of massive systemic
embolisation through pulmonary arteriovenous shunts has not been
widely investigated in both animal and human studies.
Another corroborative finding in the present
case is that, the patient was provided mechanical ventilatory
support with an anaesthetic ventilator, which had no provision
of Positive End Expiratory Pressure (PEEP). PEEP and Continuous
Positive Airway pressure (CPAP) are presumed to be therapeutic
interventions in fat embolism (in distinction to being a
supportive intervention) (18). PEEP and CPAP are well known to
recruit alveoli, increase the functional residual capacity and
also prevent the alveoli from collapsing thus facilitating a
better gas exchange (19). Improvement in ventilation – perfusion
ratio and reduction of the shunting of the deoxygenated blood to
the arterial side is the well-established function of PEEP/CPAP.
However, it is possible that the constant distending pressures
offered by these ventilatory modes may also prevent fat emboli
reaching the systemic side through both the pulmonary capillary
system as well as the arteriovenous shunts. Hence in the present
case, because PEEP was not provided, there could have been a
massive systemic embolisation of the fat through these routes.
There are additional features, which could
have contributed to the deterioration of this patient. Early
fixation of the long bone fractures is known to prevent
continuous embolisation (20). This was not done in this patient,
which could have been another reason for continuous embolisation.
In addition, transportation to various health care institutions
as well as within the hospital could have aggravated the
embolisation process into many organs. The patient did not also
receive corticosteroids, which could have prevented rapid
progression of the systemic inflammatory response.
In
summary, the present report highlights the following points:
1.Fat embolism syndrome should be suspected
even when a patient does not satisfy the Gurd’s criteria.
2.Massive paradoxical fat embolism can occur even without a
cardiac septal abnormality or arterio-venous malformations.
3.Pulmonary arterio-venous shunts, which are otherwise
physiological may open up and lead to embolisation of fat into
the left side of the heart from which it may be disseminated to
other organs, which needs to be further investigated.
4.Mechanical ventilation with PEEP/CPAP may ‘physically’ prevent
embolisation through the above route, which also needs further
investigation.
Reference :
-
Mellor A, Soni N. Fat embolism. Anaesthesia 2001;
56:145-54.
-
Thienpont E, Kaddar S, Morrison S. Paradoxical fat embolism
after uncemented total hip arthroplasty: a case report. Acta
Orthop Belg 2007; 73: 418-20.
-
Byrick R, Korley EK, McKee M, Schemitsch E, Probe RA, Kallina C.
Paradoxical fat embolism after intramedullary rodding. J
Orthop Trauma 2002; 16: 211-2
-
Kallina IV C, Probe R. Paradoxical fat embolism after
intramedullary rodding: a case report. J Orthop Trauma
2001; 15: 442-5.
-
McIntyre K, French S, Rose TH, Byrick R. Case report: acute
postoperative neurological impairment from fat embolism
syndrome. Can J Anaesth 2007; 54: 296-300.
-
Dive
AM, Dubois PE, Ide C, Bulpa PA, Broka SM, Installé E.
Paradoxical cerebral fat embolism: an unusual cause of
persistent unconsciousness after orthopedic surgery.Anesthesiology
2002; 96:1029-31.
-
Pell
AC, Hughes D, Keating J, Christie J, Busuttil A, Sutherland GR.
Brief report: fulminating fat embolism syndrome caused by
paradoxical embolism through a patent foramen ovale. N Engl J
Med 1993; 329: 926 -9
-
Kariya N, Shindoh M, Hayashi Y, Nakasuji M, Nishi S, Nishikawa
K, Asada A. A case of fatal paradoxical fat embolism syndrome
detected by intraoperative transesophageal echocardiography.
Anesth Analg 2001; 92: 688-9
-
Arai F,
Kita T, Nakai T, Hori T, Maki N, Kakiuchi M, Sasaki S.
Histopathologic features of fat embolism in fulminant fat
embolism syndrome. Anesthesiology 2007; 107: 509-11
-
Habashi NM, Andrews PL, Scalea TM. Therapeutic aspects of fat
embolism syndrome. Injury 2006; 37: S68-73
-
Gurd
A. R. Fat embolism: an aid to diagnosis.
J Bone Joint Surg 1970; 52: 732-737.
-
Robinson CM. Current concepts of
respiratory insufficiency syndromes after fracture.J
Bone Joint Surg Br 2001; 83: 781-91
-
Sevitt
S. The significance and pathology of fat embolism. Ann Clin
Res1977; 9:173 -80
-
Byrick
RJ, Mullen JB, Mazer CD, Guest CB. Transpulmonary systemic fat
embolism. Studies in mongrel dogs after cemented arthroplasty. Am J Respir Crit Care Med 1994; 150: 1416 -22
-
Riding
G, Daly K, Hutchinson S, Rao S, Lovell M, McCollum C.
Paradoxical cerebral embolisation. An explanation for fat
embolism syndrome. J Bone Joint Surg Br 2004; 86:95 -8
-
Eldridge MW, Dempsey JA, Haverkamp HC, Lovering AT, Hokanson JS.
Exercise-induced intrapulmonary arteriovenous shunting in
healthy humans. J Appl Physiol 2004; 97: 797-805
-
Koessler MJ, Pitto RP. Fat embolism and cerebral function in
total hip arthroplasty. Int Orthop 2002; 26: 259-62
-
Kusajima K, Webb WR, Parker FB Jr, Bredenberg CE, Markarian B.
Pulmonary responses of unilateral positive end expiratory
pressure (PEEP) on experimental fat embolism.
Ann Surg 1975; 181: 676-80
-
Ranieri VM, Eissa NT, Corbeil
C, et al.
Effects of positive end-expiratory pressure on alveolar
recruitment and gas excahnge in patients with adult respiratory
distress syndrome. Am Rev Respir Dis 1991; 144: 544-551
-
Pinney SJ, Keating JF, Meek RN. Fat embolism syndrome in
isolated femoral fractures: does timing of nailing influence
incidence? Injury 1998; 29:131 -3
|
|
This is a peer reviewed paper Please cite as
:Seetharaman Hariharan : Fulminating Fatal
Paradoxical Fat Embolism Without Cardiac Septal Defect -
Clinical And Histopathological Features
J.Orthopaedics 2008;5(4)e8
URL:
http://www.jortho.org/2008/5/4/e8 |
|
|