|
Abstract:
Introduction: Repairing lateral meniscal
injuries has some controversial aspects that still have not been
well-responded to. The indications for lateral meniscus repair
have been well defined and avoiding the placement of sutures
crossing the popliteal hiatus is usually recommended. The
purpose of our work is to evaluate the reliability of including
the popliteal tendon in an lateral meniscus repair. Methods: An
experimental work on lateral meniscal repair including or not
including the popliteal tendon was designed using an
experimental knee-simulator. Six fresh frozen human cadaveric
knees were used. A lateral condile osteotomy and a bucket handle
tear of the lateral meniscus were created in a reproducible
manner. The knees were divided into three groups: group A: the
meniscus was repaired with five vertical stitches avoiding the
popliteal hiatus (control group), Group B: an additional suture
was placed including the popliteal tendon and in Group C: the
same additional suture including the popliteal tendon as well as
the joint capsule was done. After a one thousand gait cycles, we
macroscopically evaluated the condition of the popliteal tendon,
the lateral meniscus and the sutures. Thereafter, the osteotomy
was again fixed and the knees were tested with external and
internal tibial rotation for five hundred cycles more in each
position and finally the last macroscopic evaluation was
performed. Results: No differences were observed between the
distinct groups. Conclusion: Repairing the lateral meniscus
along with the popliteal tendon does not seem to cause any
damage to either structure and thus suggests that lateral
meniscus can be safely repaired using this method.
J.Orthopaedics 2008;5(4)e14
Keywords:
Popliteal tendon;
Lateral meniscal repair;
Meniscus suture;
Posterolateral corner;
Knee.
Introduction:
The posterolateral corner of the knee has
received great attention over the past decade [4, 10]. Some of
its anatomical structures are thought to play an important role
as restraints on the external rotation of the tibia [12, 25].
The popliteus tendon (PT) is one of the main contributors to
static stabilization of the particular area [7, 14, 19].
The lateral meniscus’ (LM) plays a protective
effect in preventing degenerative changes in the knee joint [1,
3]. Although the connections between the PT, fibular head, and
the LM have been well established [13, 20], its dynamic
interaction is not completely understood.
In clinical practice, indications for LM
repair are well defined [8, 9, 22-23]. However, there is no
consensus with regard to repairing the LM when the rupture
involves its posterolateral zone. The main doubt being when the
tears involve the popliteal hiatus. Avoiding the placement of
sutures through the PT is usually recommended. However, no
evidence has been published about the effects of including the
PT in an LM repair, to our knowledge.
The purpose of this study is to ascertain the
reliability of including the PT in an LM repair.
Material and Methods :
Twelve fresh frozen human knees (8 left, 4
right) were obtained from donors with a mean age of 47 years
(range, 28-67 years). After the specimens were thawed overnight
at room temperature, arthroscopy of the knees was performed to
identify any previous pathology. Six knee joints had to be
excluded from the study because of LM tears, ACL insufficiency
or cartilage degeneration Outerbrigde grades III or IV. In the
end, 6 cadaveric knees (4 left and 2 right) were included in
this study.
Preparation of the cadaveric knees and
Lateral Meniscus
Each knee was prepared by transecting the
femur and tibia approximately 25 cm from the joint line. An
anatomical dissection to the capsular plane, preserving
quadriceps as well as biceps tendons, was performed. A
non-absorbable suture was used on the quadriceps and biceps
tendons to improve the attachment in the experimental knee
simulator. The lateral compartment was approached using a
lateral femoral condyle osteotomy previously described by Dienst
et al [6]. This osteotomy was planned as a vertical cut starting
directly lateral to the femoral origin of the ACL aiming towards
the lateral transition of the femoral diaphysis and metaphysis
(Fig.1). After the osteotomy, a bucket handle tear in the LM was
made. To achieve this in a reproducible manner, the LM was
divided into 3 parts starting from the meniscal wall to the free
margin. The bucket handle tear was always made at the junction
between the two-thirds medial point and the external third
(Fig.2). Afterwards, the knees were randomly divided into three
groups. In group A, the tear was repaired with five 00 vertical
non-absorbable stitches. The repair was performed combining
inside-out and outside-in techniques using 18 gauge curved
spinal needles. Two vertical stitches were placed posterior to
the popliteal hiatus and three anterior to it. This first group
was used as a control. In group B, an additional vertical suture
including the LM and the PT was added. In group C, this
additional stitch included the LM, the PT and the knee joint
capsule. Subsequently, reduction and fixation of the femoral
condyle was done with two 6.5mm cancellous screws. The bone
defect created by the saw was compensated for with a thin rubber
film.
The bone ends of the tibia and femur were
then solidly mounted using a high resistance epoxy resin in a
15cm diameter PVC tube. To improve the fixation of the tibia and
fibula in the simulator, some screws were added to the distal
part of the tibia. Finally, two additional Steimann rods were
drilled through the construct to improve rotational stability.
The femur was assembled in a cylindrical
stainless steel piece and fixed with three additional shafts.
The knees were then prepared for mounting in the experimental
knee simulator.

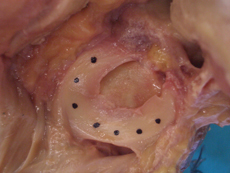
Fig.1
Technique for the lateral
condile osteotomy described by Dienst
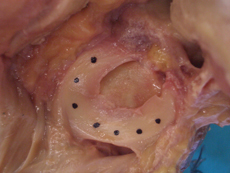
Fig.2
Lateral meniscus
preparation previous to create a bucket-handle tear

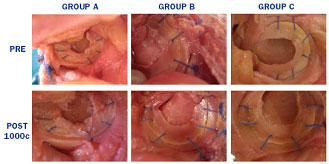
Fig.3
Type I experimental knee
simulator
Fig.4
A normal curve of a human gait cycle that reproduces the
simulator
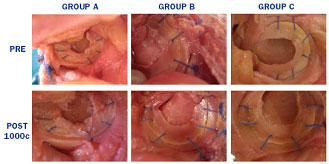
Fig.5
Macroscopic evaluation of LM, PT and sutures before and after
one thousand gait cycles and “rotational test”
Experimental Knee-Simulator
For this experimental study, we used a type I
knee-simulator (Fig.3). In the aforementioned simulators, the
forces were externally applied to the bones and
musculotendinosus structures. The simulator includes five
hydropneumatical cylinders that allow for the reproduction of
the human gait cycle. These cylinders are able to control the
flexo-extension movement of the knee during a gait cycle
(Fig.4), the ground reaction forces and its mediolateral
component as well as the extension and flexion forces of
quadriceps and femoral biceps muscles, respectively. After
putting the knees in the simulator, we were able to reproduce
the gait cycle as many times as was needed as well as control
tibial rotation.
As in previous works, the forces applied to
the knees were approximately 20% of the physiological strength
[16]. This allowed for simulating a greater number of cycles
without damaging the tendon attachments.
After a careful preparation of the specimens,
they were mounted on the simulator and one thousand gait cycles
were carried out on each one. The screws of the lateral
osteotomy were then removed and a second macroscopic look was
taken in order to evaluate the situation of the LM repair, the
PT and the sutures. In order to evaluate the viability of the
repair under rotational movements, we added as a “rotational
test” of five hundred cycles with 20º external rotation and five
hundred more with 20º internal rotation. Finally, the indemnity
or breakages of the LM, the PT as well as the stiches were
evaluated using a digital calliper (ProMax, Fowler; USA, range
0-150mm, resolution 0.02mm).
Results :
Each was evaluated after one thousand cycles.
The digital calliper was used in order to measure any disruption
of the LM or the PT. If a breakage was greater than 1mm it was
considered as a re-tearing of the LM or a partial rupture of the
PT.
With regards to the LM repair evaluations,
there were no signs of re-tearing in any of the groups and there
were no differences in them (Table I).
|
|
|
LM |
PT |
STITCH |
|
GROUP A |
KNEE 1 |
<1mm |
<1mm |
No rupture |
|
|
KNEE 2 |
<1mm |
<1mm |
No rupture |
|
GROUP B |
KNEE 3 |
<1mm |
<1mm |
No rupture |
|
|
KNEE 4 |
<1mm |
<1mm |
No rupture |
|
GROUP C |
KNEE 5 |
<1mm |
<1mm |
No rupture |
|
|
KNEE 6 |
<1mm |
<1mm |
No rupture |
Furthermore, the PT was not damaged by the
non-absorbable 00 stitches when they were included in the repair
(Fig.5).
We were also able to prove that there were
not any ruptures of the stitches in the three groups.
Furthermore there were no differences between
the three groups before or after the “rotational test.”
Discussion :
There is much mention in recent literature
about the posterolateral corner of the knee and lateral meniscal
repair. Most of the material covers anatomical descriptions or
biomechanical studies of some of the structures in this
particular area [4, 7, 10, 12, 14, 19, 25]. It is well known
that the entire periphery of the LM is not fused to the capsule.
The posterior margin of the meniscus is adjacent to the
articular recess that separates the LM from the tendon. This is
confirmed in other works, using late-stage human fetuses, with
arthroscopical and also histological evaluation [13, 20]. It is
also known that popliteus muscle inserts into a triangular area
along the posteromedial aspect of the proximal tibia and has
some static and dynamic functions such as the “unlocking” of the
knee joint and preventing forward dislocation of the femur from
the tibia during initial flexion. Ricklin et al. [18] described
“two thin tissue bridges” attaching the LM to the joint capsule
and the synovial membrane of the PT around the popliteal hiatus.
Using 10 fresh frozen human knee specimens in 1979, Conh et al.
[5], considered the popliteomeniscal fascicles to be the
superior and inferior limits of the popliteal hiatus. They
emphasized that the anatomy of the popliteal hiatus is constant.
Nowadays, there is a relative consensus with
regard to the necessity to repair the popliteomeniscal fascicles
in cases of posterolateral instability of the knee [11].
Furthermore, the role of LM stabilizers was
well-studied during the flexo-extension movement of the knee.
Minowa et al. described solid PT attachments to the fibula and
LM in late-stage fetuses [13]. Sussmann et al. [20] hypothesized
a retractor function of the PT and popliteofibular ligament of
the LM during knee flexion. All these physiological actions on
the LM are very important in order to better understand the
effect of a lateral meniscectomy or a LM repair.
On the other hand, the long-term effects of
the meniscectomy are well-known. Kimura et al., obtained better
results after a subtotal meniscectomy or an LM repair rather
than with a partial meniscectomy in an analysis of the knee
functional scores [10]. This was thought to be due to the fact
that the LM was forcefully pulled back by the popliteal muscle
when the knee was flexed. After a partial meniscectomy, this
force was not transmitted to the portion where the residual
meniscus and synovial membrane meet.
Stäubli et al. [19] performed a dynamic study
with videoarthroscopic control in order to gain a better
undertanding of the PT’s work. They found the PT was covered by
synovial tissue. The superior and inferior popliteal fascicles
control the play of the LM. With increased flexion of the knee,
the tendon progressively glided into the popliteal sulcus, which
was angled at 30º to the saggital plane of the femoral shaft.
The PT clearly changed position and orientation between the
extended and the flexed positions. Furthermore, the tension in
the tendon gradually increases when the knee extends.
In a cadaveric study, Tria et al. [21]
reported that the PT in 7 out of 40 knees had strong dual
attachments to the LM and the lateral femoral condile. More
recently, Bozkurt et al. [4] described the importance of the PT
and meniscofibular ligament in LM movement during flexo-extension
of the knee. They hypothesized that all these solid attachments
to the LM may be one of the causes of repeating LM tears.
Our results suggest that the inclusion of the
PT in a lateral meniscal repair does not appear to cause
excessive tension on all these structures. Consequently, there
is no significant repercussion on the LM’s or PT’s functioning.
The closure of the popliteal hiatus may have a similar effect on
the LM, more so than all the ligaments previously mentioned.
Including the PT in the repair and the closure of the popliteal
hiatus with an additional stitch can probably improve the
stability and the strength of the repair without significantly
changing the kynematics of the posterolateral corner of the
knee.
We are aware that this work has some
limitations that we should take into account. In the first
place, in spite of the number of cycles, we cannot simulate the
popliteal muscle contraction. This might be one of the reasons
why the “rotational test” does not affect the viability of the
repair. To our knowledge, there is no exact measurement of the
force that the popliteal muscle exerts and we do not know its
repercussion on the kynematics of the knee.
Moreover, the experimental simulator worked
within the range of infra-physiological forces [16] and the
relation of 1000 cycles corresponded approximately to a distance
of 1500 meters. A greater number of cycles might be necessary to
come to a definitive conclusion.
Notwithstanding, to our knowledge there are
no works in the literature dealing with lateral meniscal repair
that include the PT. In conclusion, repairing the LM along with
the PT does not seem to cause any damage to either structure and
this suggests that the LM can be safely repaired using this
method. More research and clinical series are needed to confirm
these preliminary findings.
Reference :
-
Alford JW, Lewis
P, Kang RW, Cole BJ (2005) Rapid progression of chondral
disease in the lateral compartment of the knee following
meniscectomy. Arthroscopy 21(12):1505-9
-
Aronowitz ER,
Parker RD, Gatt CJ (2001) Arthroscopic identification of the
popliteofibular ligament. Arthroscopy 17(9):932-9
-
Beaufils P, Hardy
P, Chambat P, Clavert P, Djian P, Frank A, Hulet C, Potel JF,
Verdonk R (2006) Adult lateral meniscus. Rev Chir Orthop
Reparatrice Appar Mot 92(5 Suppl):2S169-2S194
-
Bozkurt M, Elhan
A, Tekdemir I, Tonuk E (2004) An anatomical study of the
meniscofibular ligament. Knee Surg Sports Traumatol Arthrosc
12(5):429-33
-
Cohn AK, Mains DB
(1979) Popliteal hiatus of the lateral meniscus. Anatomy and
measurement at dissection of 10 specimens. Am J Sports Med
7(4):221-6
-
Dienst M, Greis
PE, Ellis BJ, Bachus KN, Burks RT (2007) Effect of lateral
meniscal allograft sizing on contact mechanics of the lateral
tibial plateau: an experimental study in human cadaveric knee
joints. Am J Sports Med 35(1):34-42
-
Ferrari DA (2005)
Arthroscopic evaluation of the popliteus: Clues to
posterolateral laxity. Arthoscopy 21(6):721-6
-
Haas AL, Schepsis
AA, Hornstein J, Edgar CM (2005) Meniscal repair using FastT-Fix
all-inside meniscal repair device. Arthroscopy 21(2):167-75.
-
Jones HP, Lemos MJ,
Wilk RM, Smiley PM, Gutierrez R, Schepsis AA (2002) Two year
follow-up of meniscal repair using a bioreabsorvable arrow.
Arthroscopy 18(1):64-9
-
Kimura M,
Shirakura K, Hasegawa A, Kobayashi Y, Udagawa E (1992) Anatomy
and pathophysiology of the popliteal tendon area in the
lateral meniscus: 2. Clinical investigation. Arthroscopy
8(4):424-7
-
LaPrade RF,
Konowalchuk BK (2005) Popliteomeniscal fascicle tears causing
symptomatic lateral compartment knee pain: diagnosis by the
figure-4 test and treatment by open repair. Am J Sports Med
33(8):1231-6
-
Maynard MJ, Deng
X, Wickiewicz TL, Warren RF (1996) The popliteofibular
ligament. Rediscovery of a key element in posterolateral
stability. Am J Sports Med 24(3):311-6
-
Minowa T, Murakami
G, Suzuki D, Uchivama E, Kura H, Yamashita T (2005)
Topographical histology of the posterolateral corner of the
knee, with special reference to laminar configurations around
the popliteus tendon: a study of elderly Japanese and
late-stage fetuses. J Orthop Sci 10(1):48-55
-
Nielsen S, Helming
P (1986) The static stabilizing function of the popliteal
tendon in the knee. An experimental study. Arch Orthop Trauma
Surg 104(6):357-62
-
Perez Carro L,
Sumillera Garcia M, Sunye Gracia C (1999) Bifurcate popliteus
tendon. Arthroscopy 15(6):638-9
-
Prilutsky BI,
Petrova LN, Raitsin LM (1996) Comparison of mechanical energy
expenditure of joint moments and muscle forces during human
locomotion. J Biomechanics 29(4):405-15
-
Reis FP, de
Carvalho CA (1975) Anatomical study on the proximal
attachments of the human popliteus muscle. Rev Bras Pesqui Med
Biol 8(5-6):373-80
-
Ricklin P,
Ruettimann A, Del Buono MS (1971) Meniscus Lesions. New York,
Grune&Stratton 41
-
Staubli HU, Birrer
S (1990) The popliteus tendon and its fascicles at the
popliteal hiatus: gross anatomy and functional arthroscopic
evaluation with and without anterior cruciate ligament
deficiency. Arthroscopy 6(3):209-20
-
Sussmann PS,
Simonian PT, Wickiewicz TL, Warren RF (2001) Development of
the popliteomeniscal fasciculi in the fetal human knee joint.
Arthroscopy 17(1):14-8
-
Tria AJ, Johnson
CD, Zawadsky JP (1989) The popliteus tendon. J Bone Joint Surg
(Am) 71:714-6
-
Tsai AM,
McAllister DR, Chow S, Young CR, Hame SL (2004) Results of
meniscal repair using a reabsorvable screw. Arthroscopy
20(6):586-90
-
Tuckman DV,
Bravman JT, Lee SS, Rosen JE, Sherman OH (2006) Outcomes of
meniscal repair: minimum of 2 year follow-up. Bull Hosp Jt Dis
63(3-4):100-4
-
Ullrich K, Krudwig
WK, Witzel U (2002) Posterolateral aspect and stability of the
knee joint. I. Anatomy and function of the popliteus
muscle-tendon unit: an anatomical and biomechanical study.
Knee Surg Sports Traumatol Arthrosc 10:86-90
-
Veltri DM, Deng XH,
Torzilli PA, Maynard MJ, Warren RF(1996) The role of the
popliteofibular ligament in stability of the human knee. A
biomechanical study. Am J Sports Med 24(1):19-27
|