|
Abstract:
Background and aim: Magnetic resonance imaging of the knee
is frequently used in the diagnosis of anterior cruciate
ligament (ACL) and meniscal injuries. Arthroscopy has remained
as the gold standard in the diagnosis of internal pathologies
of the knee, against which other modalities are compared. The
aim of this retrospective study was to determine the reliability
and value of clinical history, physical examination and MRI in
our management of ACL and meniscal tears in the local context.
Methods:
A total of 86 patients with a preoperative MRI done underwent
arthroscopy over a 10 month period in a tertiary institution.
Clinical history, physical examination and MRI findings were
compared with arthroscopic findings. Sensitivity, specificity,
positive predictive value (PPV), negative predictive value (NPV)
were then calculated.
Results:
The sensitivity of clinical examination and MRI is 80.3% and
84.3% and specificity 94.2% and 91.4% for ACL tears
respectively. Clinical examination for ACL tears has a PPV and
NPV of 95.3% and 76.7% respectively while the PPV and NPV of MRI
is 93.4% and 80% respectively. MRI is superior than clinical
methods in diagnosing meniscus lesions. For the medial meniscus,
It has a sensitivity of 91.4% and specificity of 66.6%. For the
lateral meniscus, it has a sensitivity and specificity of 76%
and 86.6% respectively.
Conclusion:
Based on these findings, our current practice of requesting
scans to routinely confirm the diagnosis should be altered.
Unnecessary MRI scanning increases the financial burden and
delays patient treatment. Equivocal clinical findings in
patients with acute knee injury should lead to use of MRI in an
appropriate clinical setting, and may lead to a reduction in
unjustified knee arthroscopy.
J.Orthopaedics 2008;5(3)e8
Introduction:
Magnetic Resonance Imaging (MRI) has gained in popularity as a
diagnostic tool of the musculoskeletal system since its
introduction in the 1980s1. It is non-invasive and
requires no exposure to ionizing radiation. Diagnostic
arthroscopy of the knee has also been increasingly performed as
it is highly accurate and can be therapeutic at the same
setting. However, it may be complicated by infection,
haemoarthrosis, adhesions and reflex sympathetic dystrophy, as
well as complications related to anaesthesia2. In a
medical environment with ever-increasing health costs and
litigation, the judicious use expensive MRI or invasive
arthroscopy in the diagnosis of internal derangements of the
knee has not been clearly defined.
Clinical diagnosis of knee pathology depends on the experience
and expertise of the clinician. The high incidence of abnormal
MRI findings in asymptomatic subjects underscore the danger of
relying on a diagnostic test without careful correlation with
clinical history or examination3. Few would argue
that there
is little role for MRI when patients have definite clinical
signs. However, when clinical symptoms and signs are subtle, MRI
should be done as it may spare patients from unnecessary and
expensive surgery4.
Some authors5 suggest physical examination and well
taken history are more cost-effective means of diagnosing
anterior cruciate ligament and meniscal injury than MRI. If the
clinical findings are sufficiently predictive, then an
additional imaging study may be unnecessary before proceeding
with a therapeutic arthroscopy. The patient can be saved time
and expense.
On the
other hand, multiple nonrandomized studies in the literature
have shown that MRI is cost-effective before the performance of
knee arthroscopy6,7,8 and can decrease the frequency
and subsequent need for arthroscopic surgery9.
Rangger10 and Spiers11 have shown that in
their studies that MRI examination of suspected meniscus
injuries before the scheduled operation could reduce the total
number of arthroscopies by 30%. Crotty12 proposed MRI
as a screening tool before arthroscopy due to its high
sensitivity for arthroscopically remediable lesions in cases of
internal derangement of the knee. However,
Bridgman et al13 reported that that MRI did not
reduce arthroscopy rates or improve outcomes for his series of
252 patients waiting for knee surgery.
The aim of this review is to determine the accuracy of clinical
history, physical examination and MR Imaging in the diagnosis of
knee injuries in our local population. This allows us to
practice in a more cost effective approach, thus saving the
patient unnecessary MRI or unjustified knee arthroscopy.
Material and Methods :
From our operative records between July 2007 and May 2008, we
identified 86 patients who had a MRI knee investigation
performed, and subsequently underwent knee arthroscopy as day
case procedure under either regional or general anaesthesia.
There were 8 female and 78 male patients age ranged from 18 to
53 years of age.
We retrospectively reviewed their medical records to review
their clinical history and physical examination findings, MRI
and arthroscopy findings of ACL and meniscus pathology.
A positive clinical history of a torn ACL includes symptoms of
giving way or instability, and complaints of locking or
decreased range of motion signify a positive history of meniscus
pathology. A torn ACL is determined by clinical examination
using the anterior drawer test or Lachman test while Mcmurray
test is used to determine the presence of a meniscus tear.
Direct signs of ACL tear on MRI include nonvisualisation,
discontinuity, wavy and irregular appearance and edematous mass
in region of anterior cruciate ligament. Meniscal tears are
depicted on MR images as areas of linear abnormally increased
signal intensity within the meniscus, which extend to and
communicate with an articular surface.
The MRI findings of anterior cruciate ligament (ACL), medial and
lateral meniscal tears were recorded. This was compared against
the intraoperative knee arthroscopy findings, which were
regarded as the gold standard.
The sensitivity, specificity, positive predictive value (PPV),
negative predictive value (NPV) and accuracy were then
calculated.
The sensitivity measures the proportion of actual positives
which are correctly identified while the specificity measures
the proportion of negatives which are correctly identified as
such. The positive predictive value is the proportion of
patients with positive test results who are correctly diagnosed.
The negative predictive value is the proportion of patients with
negative test results who are correctly diagnosed. Accuracy is
the proportion of true results (both true postive and true
negatives) in the study cohort.
We then tabulated the sensitivity, specificity, PPV, NPV and
accuracy of clinical history, physical examination and MRI
against arthroscopy, which was used as a gold standard, in the
diagnosis of ACL and meniscus tears. We then compared MRI
against arthroscopy in determining medial and lateral meniscus
tears.
Results :
ACL Tears
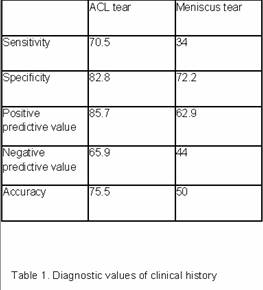
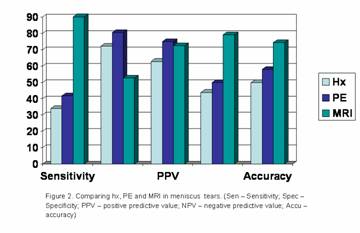
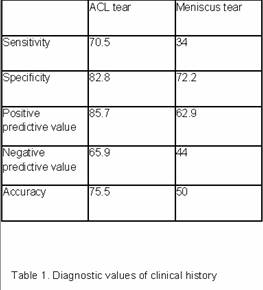
Figure 1 showed that clinical history has lower sensitivity,
specificity, PPV and NPV than clinical examination and MRI.
Clinical history of giving way or instability only has an
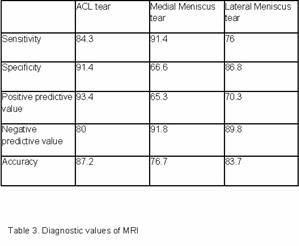
accuracy of 75.7% (table 1). Both clinical examination and MRI
have higher accuracy of 86% and 87.2% respectively.
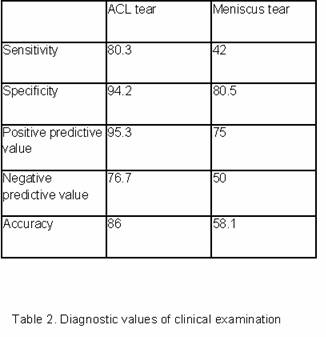
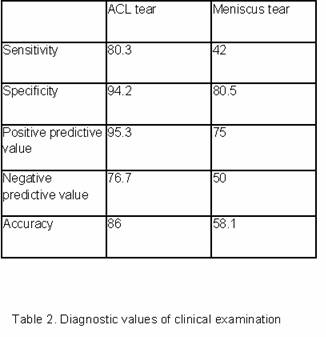
Clinical examination and MRI share similar sensitivity (80.3% v
84.3%) and specificity (94.2% v 91.4%) for ACL tears. Clinical
examination for ACL tears has a PPV and NPV of 95.3% and 76.7%
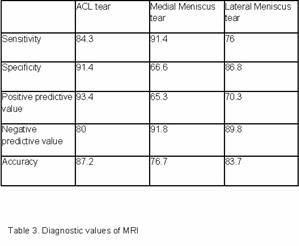
respectively while the PPV and NPV of MRI is 93.4% and 80%
respectively. (refer to table 2 and 3)
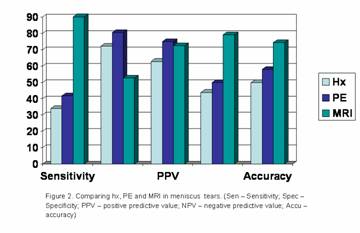
Meniscus tears
Clinical history of locking or decreased ROM has low sensitivity
and specificity in diagnosing meniscus tears (table 1). Similary,
the McMurray test exhibits only a sensitivity and specificity of
42% and 80.5% respectively (table 2). The overall accuracy of
clinical history and examination is 50% and 58.1% respectively.
According to our results, MRI is superior to clinical methods in
diagnosing meniscus tears (figure 2). Table 3 showed that for
the medial meniscus, MRI has a sensitivity and specificity of
91.4% and 66.6% respectively. For the lateral meniscus, it has a
sensitivity and specificity of 76% and 86.6% respectively.
MRI has a higher NPV of 91.8% (medial meniscus) and 89.8%
(lateral meniscus), as compared to NPV of 80% for ACL tears.
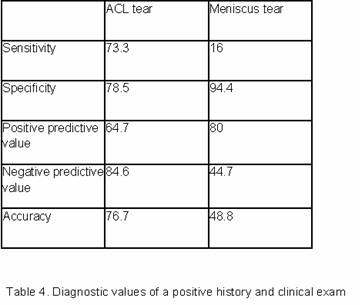
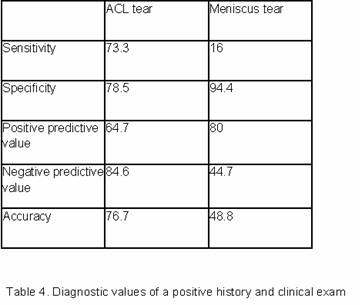
Table 4 shows in the presence of a positive history and McMurray
test, the PPV is 80%, which is higher than the PPV of MRI.
However, it only has a low sensitivity of 16%.
Discussion :
The usefulness of MRI in evaluating the knee was first
recognized in the early 1980s. It has also been shown to
determine the extent of an injury and help in the planning of
its management. Even when a particular diagnosis is clinically
apparent, MRI can be used to delineate associated abnormalities
and more fully demonstrate the extent of the injuries.
Our results suggest that in diagnosing ACL tears, clinical
examination is comparable to MRI. The anterior drawer or Lachman
test in diagnosing ACL tear has also been validated in other
studies14, although the sensitivity varies depending
on the experience of the surgeon. Madhu15 and Gelb16
reported 100% sensitivity while Nikolaou17 reported
only 68% sensitivity of clinical examination. In our study,
sensitivity of clinical examination is 80.3% and specificity is
94.2%, compared to sensitivity of MRI 84.3 and 91.4%
respectively. Jackson18 reported a MRI sensitivity of
100% while Glashow19 reported only 61% in his cohort.
In a multi-centre analysis of 1014 patients20, the
accuracy of the diagnosis of ACL tear by MRI was 93%, compared
to 87.2% in our centre. These results suggest that MRI is centre
and radiologist dependent. The high PPV of clinical examination
of 95.3% is comparable to other studies. This means that MRI may
not cost effective in diagnosing ACL tears21, as
compared to clinical methods.
In the diagnosis of meniscus lesions, the McMurray test, Apley
test, Steinman sign and Childress test are examples of the
numerous tests described in the literature. Joint line
tenderness of the knee joint is non specific. Graham Apley wise
words of “there is no pathgnomoic sign of meniscus” still ring
true today, as our results show.
Clinical history of locking or decreased range of motion is not
accurate (50%) and McMurray test has low accuracy of 58.1% in
our study. Madhu15 reported only 38.75% sensitivity
for meniscus tear by clinical examination and 59% sensitivity by
MRI. His finding that clinical examination has low sensitivity
is rather similar to our results of 42%, although we found that
MRI has a sensitivity of 90% of identifying meniscus tears. In
contrast, Rayan22 reported that clinical examination
was overall superior to MRI in terms of sensitivity,
specificity, PPV, NPV and accuracy in diagnosing meniscus tears.
Our study showed a sensitivity of 91.4% and 76% of MRI in
diagnosing medial meniscus and lateral meniscus tears
respectively. In our cohort, MRI has a specificity of 66.6% for
medial meniscus tears and 86.8% for lateral meniscus tears and
our results are similar to other published reports. Rangger10
reported sensitivity of MRI compared to arthroscopic findings
was 93% for medial meniscus and 78% for lateral meniscus;
specificity was 74% for medial meniscus and 89% for lateral
meniscus. Raunest23 and Oei 24 also showed
that MRI has a higher sensitivity for detection of tears of
medial meniscus than for tears of lateral meniscus. Specificity
is higher for tears of the lateral meniscus than for tear of
medial meniscus.
Nevertheless, MRI has its limitations in diagnosing meniscus
tears25, hyaline articular cartilage wear and in
differentiating of complete and partial anterior cruciate
ligament tears26. False positive MRI diagnoses of
meniscal tears may lead to unjustified knee arthroscopy27.
However, some authors sugest that at these meniscal
abnormalities seen at MRI represent closed intrasubstance tears,
which may not be detected at arthroscopy unless carefully
probed.
We
recognise the limitations of this study in terms of the small
numbers but believe that the groups studied are representative
of the population normally attending the orthopaedic clinics.
Conclusion:
Our results emphasize the importance of history and clinical
examination in the diagnosis of ligament and meniscus injuries
of the knee. The anterior drawer or Lachman test is highly
accurate compared to the MRI in diagnosing ACL tears. Our study
also showed that a positive history and clinical finding of a
meniscus tear has a higher positive predictive value than MRI.
Therefore, MRI in these clinical scenarios may be unnecessary.
However, MRI has a role in excluding meniscus tears due to its
high negative predicitive value, and may save the patient
unjustified surgery. This study enables us to counsel our
patients appropriately on the value of doing such an
investigation as well as the subsequent management of MRI
findings.
Reference :
-
Barronian AD, Zoltan JD, Bucon KA: Magnetic resonance imaging of
the knee: correlation with arthroscopy. Arthroscopy 1989; 5:
187-91.
-
Polly DW
Jr,
Callaghan
JJ,
Sikes RA,
McCabe JM,
McMahon K,
Savory CG.
The accuracy of selective magnetic resonance imaging compared
with the findings of arthroscopy of the knee.J
Bone Joint Surg Am. 1988 Feb;70(2):192-8.
-
Boden SD, Davis DO, Thomas SD, et al: A prospective and
blinded investigation of magnetic resonance imaging of the knee.
Clin Orthop 1992; 282: 177-85.
-
Ryzewicz M , PetersonB, Siparsky PN, Bartz RL. The
Diagnosis of Meniscus Tears The Role of MRI and Clinical
Examination. Clinical Orthopaedics and Related Research. Number
455, pp. 123–133
-
Liu SH, Osti L, Henry M, Bocchi L. The diagnosis of acute
complete tears of the anterior cruciate ligament. Comparison of
MRI, arthrometry and clinical examination. J Bone Joint
Surg [Br] l995;77-B:586-8.
-
Boden SD, Labropoulos PA, Vailas JC: MR scanning of the
acutely injured knee: sensitive, but is it cost effective?
Arthroscopy 1990; 6: 306-10.
-
Newman AP, Daniels AU, Burks RT: Principles and decision making
in meniscal surgery. Arthroscopy 1993; 9: 33-51.
-
Vincken
PW, ter Braak BP, van Erkell AR, de Rooy TP, Mallens WM, Post W,
Bloem JL.Effectiveness of MR imaging in selection of
patients for arthroscopy of the knee. Radiology. 2002
Jun;223(3):739-46.
-
Trieshmann HW, Mosure JC: The impact of magnetic resonance
imaging of the knee on surgical decision making. Arthroscopy
1996; 12: 550-6.
-
Rangger C, Klestil T, Kathrein A, Indenter A, Hamid L.
Influence of Magnetic Resonance on Imaging on Indications for
Arthroscopy of the Knee. Clinical Orthopaedics and Related
Research 330;133-142
-
Spiers ASD, Meagher T, Ostlere SJ, Wilson DJ, Dodd CAF: Can MRI
of the knee affect arthroscopic practice? J Bone Joint Surg Br
1992; 75: 49-52.
-
Crotty JM, Mom JUK, Pope TL. Magnetic Resonance Imaging
of the Musculoskeletal System Part 4. The Knee Clinical
Orthopaedics and Related Research 330;288-303.
-
Bridgman S, Richards PJ, Walley G, MacKenzie G, Clement
D, McCall I, Griffiths D, Maffulli N. The Effect of Magnetic
Resonance Imaging Scans on Knee Arthroscopy: Randomized
Controlled Trial. Arthroscopy. 2007 Nov;23:1167-73.
-
Lee JK, Yao L, Carlton TP, Wirth CR, Czajka J, Lozman J:
Anterior cruciate ligament tears: MR imaging compared with
arthroscopy and clinical tests. Radiology 1988; 166: 861-4.
-
Madhusudhan
T, Kumar T, Bastawrous S, Sinha A.Clinical
examination, MRI and arthroscopy in meniscal and ligamentous
knee Injuries - a prospective study.J Orthop Surg. 2008 May
19;3:19.
-
Gelb HJ, Glasgow SG, Sapega AA, Torg JS: Magnetic resonance
imaging of knee disorders, clinical value and cost-effectiveness
in a sports medicine practice. Am J Sports Med 1996; 24: 99-103.
-
Nikolaou
VS, Chronopoulos E, Savvidou C, Plessas S, Giannoudis P,
Efstathopoulos N, Papachristou G.MRI efficacy in
diagnosing internal lesions of the knee: a retrospective
analysis.J Trauma Manag Outcomes. 2008 Jun 2;2(1):4.
-
Jackson DW, Jennings LD, Maywood RM, Berger PE.Magnetic
resonance imaging of the knee Am. J. Sports Med. 1988; 16; 29
-
Glashow Ll, Katz R, Schneider M, Scott WN: Double-blind
assessment of the value of magnetic resonance imaging in the
diagnosis of anterior cruciate and meniscal lesions. J Bone
Joint Surg Am 1989; 71: 113-9.
-
Fischer SP, Fox JM, Pizzo WD, et al: Accuracy of diagnoses from
magnetic resonance imaging of the knee. J Bone Joint Surg Am
1991; 73: 2-10.
-
Rose NE, Gold SM: A comparison of accuracy between clinical
examination and magnetic resonance imaging in the diagnosis of
meniscal and anterior cruciate ligament tears. Arthroscopy 1996;
12: 398-405.
-
Rayan F, Bhonsle S, Divyang D, Shukla D.Clinical, MRI,
and arthroscopiccorrelation in meniscal and anterior cruciate ligament
injuries.International Orthopaedics 2008 Feb 23.
-
Raunest J, Oberle K, Loehnert J, Hoetzinger H: The clinical
value of magnetic resonance imaging in the evaluation of
meniscal disorders. J Bone Joint Surg Am 1991; 73: 11-6.
-
Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG. MR
Imaging of the Menisci and Cruciate Ligaments: A Systematic
Review. Radiology. 2003 Mar 226:837-48.
-
Silva I
Jr,
Silver DM.
Tears of the meniscus as revealed by magnetic resonance imaging.J
Bone Joint Surg Am. 1988 Feb;70(2):199-202.
-
Oberlander MA, Shalvoy RM, Hughston JC: The accuracy of the
clinical knee examination documented by arthroscopy. Am J Sports
Med 1993; 21: 773-8. 17.
-
Peleg Ben-Galim, Ely L. Steinberg, ; Hagai Amir, ;
Nachman Ash, Shmuel Dekel, MD, Ron Arbel
Accuracy of Magnetic Resonance Imaging of the Knee and
Unjustified Surgery. Clinical Orthopaedics and Related Research.
447, pp. 100–104
|