| ORIGINAL
ARTICLE |
|
Posterior-Stabilized Total Knee
Replacement In Rheumatoid Arthritis |
|
Almeida F*, Martin J M**, Silvestre A ***, Gomar F #.
*
Consultant Orthopaedic Surgeon
**
Resident
***
Consultant Orthopaedic Surgeon
#
Director Department of Orthopaedics, Clinic University Hospital, Valencia.
Spain
Address for Correspondence:
Fernando Almeida Herrero.
Av Cortes Valencianas 41 61. 46015.
Valencia. Spain.
Tel: +34606609925.
Fax:
+34963987651.
E-mail: falmeidah@gmail.com
|
|
Abstract:
We
retrospective compared the outcomes of 42 total knee
replacements in 28 patients with rheumatoid artritis, after an
average follow-up of 7.5 years. Revision was necessary in nine
knees (21.4%). No revision for deep infection was done. Four
patients died and two patients (with bilateral replacement) had
a follow-up less than two years, so they are not included in
this serie. The mean Hospital for Special Surgery score was 79.6
and the mean clinical and functional Knee Society score were 83
and 61, respectively. The mean flexion angle at follow-up
evaluation was 97.8º+18.4. The rate of survival at eight years
was 81% with femoral or tibial revision for any reason as the
end point. Total knee arthroplasty is a good option in patients
with rheumatoid arthritis in the medium term follow-up, even
though it is not free of complications.
J.Orthopaedics 2008;5(3)e3
Keywords:
Arthroplasty; Knee; Rheumatoid arthrtitis
Introduction:
Total knee arthroplasty (TKA) provides good pain relief and
functional recovery in patients with impaired walking ability
and persistent knee pain caused by chronic rheumatoid arthritis.
Patients with rheumatoid arthritis are on average approximately
10 years younger than patients with osteoarthritis at the time
of total knee arthroplasty.
[1]
Assuming the patient has a normal life span, a total knee
arthroplasty in a patient with rheumatoid arthritis will have to
be good functioning for a longer time so we should take into
account this for late complications such as infection,
loosening, component wear, and osteolysis.
The
aim of this retrospective study was to review our clinical and
radiological mid-term results (mean follow-up of 7 years) after
total knee arthroplasties in patients with rheumatoid arthritis.
Preoperative patient evaluation
Before performing a total knee replacement on a patient with
rheumatoid arthritis, a careful preoperative assessment is
crucial.
Systemic nature of the disease and long-term therapies with
corticoisteroids and immunosuppressive drugs can modify the
immune system of these patients. Approximately 10% of patients
with RA at the time of total knee arthroplasty are taking
maintenance corticosteroids.[1,2]
These drugs and the patient´s nutritional status can affect the
rate of wound healing and the incidence of infection, in the
immediate post-op and in the long run. The incidence of
infection after joint replacement surgery in patients with RA is
three times greater than in the general population.[1]
As
well as corticosteroids and immunosuppressive therapies,
nonsteroidal anti-inflammatory drugs are a mainstay in the
treatment of rheumatoid symptoms. These drugs have influence on
deep venous thrombosis prophylaxis, anesthesia and postoperative
pain management. Aspirin and ibuprofen harmfully influence the
coagulation profile of the patients, so the use of warfarin or
low-molecular-weight heparin together with these nonsteroidal
anti-inflammatory drugs is contraindicated.
The
knee is among the most commonly affected joint in rheumatoid
arthritis. Indeed, it is estimated that up to 90% of these
patients will eventually have involved one or both knees.[3]
Polyarticular involvement of rheumatoid arthritis requires
careful planning in order to optimize the patient´s overall
function. As much as 50% of patients with rheumatoid disease of
the knee have concomitant hip involvement.[4]
Hip replacement should be done before knee replacement when both
are indicated in the same leg for several reasons. Pain from an
unhealthy hip may be referred to the knee, so hip arthroplasty
may delay the need for total knee prosthesis. On the other hand,
rehabilitation after hip arthroplasty is possible in the
presence of knee arthritis but the opposite situation is quite
hard. Finally, the overall experience of undergoing hip
arthroplasty is easier from patient´s perspective in terms of
pain and rehabilitation and therefore will set up patient
confidence in the use of these devices more promptly.
Upper-extremity involvement of the disease must also be assessed
prior to undertaking total knee arthroplasty in rheumatoid
patients. Often, the involvement of the shoulders, elbows or
wrists hinders the use of canes which are necessary for walking
in the weeks following knee replacement. Up to 105º of knee
flexion is required to rise from a seated position without the
help of the upper extremities. Hence, any surgical technique
should attempt to restore plenty knee flexion in order to
maintain independent function in patients with upper-extremity
disease.[5]
Finally, the use of disease-modifying agents in the
perioperative period has been of great concern for orthopaedic
surgeons. Use of methrotrexate should finish just about 2 weeks
before surgery and in the immediate postoperative period because
of fluid-balance disturbances and the possibility of infections.[6,7]
However, larger prospective clinical trials are required to
ascertain the precise effects of these disease-modifying agents
on the TKA population.
Material and Methods :
Between February 1990 and May 2005, 42 cemented primary
posterior-stabilized total knee arthroplasty were performed in
28 patients with rheumatoid arthritis at our Hospital. Four
cemented posterior-stabilized designs were included: Hermes
(Osteal-Ceraverâ),
Performance (Biometâ),
Link (Linkâ)
and Interax (Strykerâ)
(Figure 1). The Hermes implant was mainly use in 16 knees while
the Link and Interax implant was used only in one case
respectively.
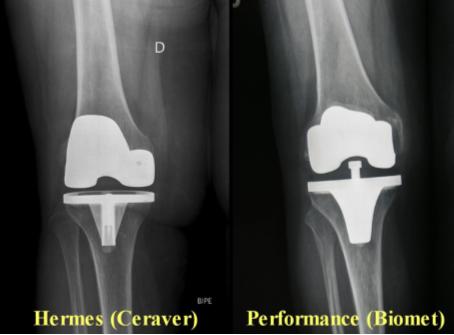
Fig. 1. Main posterior-stabilized designs used. Hermes
(Osteal-Ceraverâ),
Performance (Biometâ)
Four patients (8 knees) died during the follow-up,
two patients (4 knees) have not included in the group because
the follow-up was less than two years and revision surgery was
done in five patients (9 knees), so they have also been
excluded. None of the patients who died underwent revision
surgery or reported complications related to their knees while
they were alive. Therefore 21 knees in 17 patients have been
included in our group for clinical and X-ray evaluation. The end
of the follow-up was July 2007, so all patients had a minimum of
two years record (mean 7.4; 2 to 12).
The study included 16 female and one male with a
mean age of 62 years (range 28-80 years) at the time of their
replacement. Four patients had bilateral surgery. A previous
operation, open synovectomy, had been performed in only one
patient.
A midline skin incision with a medial parapatellar
splitting of the quadriceps was used in all the patients. The
distal femur was then excised to achieve a tibiofemoral
alignment of 5º of valgus in the coronal plane. After achieving
ligamentous balance, the proximal tibia was resected in order to
get a surface perpendicular to the shaft of the tibia in coronal
plane. Careful awareness to match gaps and to the correct any
pre-operative flexion contracture was paid. The patella was
resurfaced in all cases.
Patients began active and passive motion of their
knees and started walking with aids about two days, after
surgery. We used in our hospital continuous passive motion
machines for the rehabilitation program.
The patients were evaluated clinically using the
rating systems of the Hospital for Special Surgery (HSS)
[8]
and the Knee Society (KS).[9]
In the KS rating system, two scores were assigned: one for knee
score (pain, range of motion, and stability) and another for
function score (walking, stair climbing, and use of walking
aids).
In the early post-operative and final follow-up
standing anteroposterior and lateral radiographs were assessed
for radiolucency at bone-implant interfaces, lateral and medial
joint spaces, measurement of angles
a,b,d
and
g,
change in the position of the components and osteolysis,
according to the method of the Knee Society.[9]
Radiolucencies at the bone-cement interface were evaluated in 7
zones in the anteroposterior view of the tibial component, 3
zones in the lateral view of the tibial component and 5 zones in
the lateral view of the femoral component. Patients were
reviewed by two senior physicians, independently of the surgeon
performing the procedure.
Survivorship analysis was performed using the
Kaplan-Meier method with the end-point being removal or revision
of a component for any reason.
[10]
Results :
The
average Hospital for Special Surgery score was 79.6+10.2 at the
final follow-up assessment. The mean clinical and functional
Knee Society in knee score were 83 (41 to 99) and in the
function score were 61 (0 to 100) at the end of the follow-up.
All the patients were included in category type C with multiple
arthritis and medical infirmity.[9]
At this time 14 knees (66.6%) were pain-free, four knees (19.1%)
were somewhat painful during long walks, two knees (12.2%) were
fairly painful during stair climbing and a knee (2.1%) was
hardly painful while walking. No one was painful at rest. Twelve
patients (70.5%) did not require a cane for walking, two (11.8%)
needed a cane only for long walks, two (11.8%) used a cane
full-time, and one of them (5.9%) was forced to use a walker.
The mean active range of motion of the knees was 97º
(15º to 130º). Flexion contracture less than 15º was seen in
five knees (24%). However, flexion less than 90º was observed in
five knees (24%) at follow-up evaluation.
Femorotibial alignment of 5.5º of valgus (range,
3.1º to 12º) was measured on the postoperative radiograph in the
standing position. The mean position of the components was 94º
(range, 79.5º-100.8º) for the femoral (alfa), and 87.9º (range,
84º-92º) for the tibial one (b).
Flexion of the femoral component (g)
was 5.9º (range, 0º-27.9º), and the slope of the tibial
component (d)
was 89.6º (range, 83.6º-94.5º) (Figure 2).
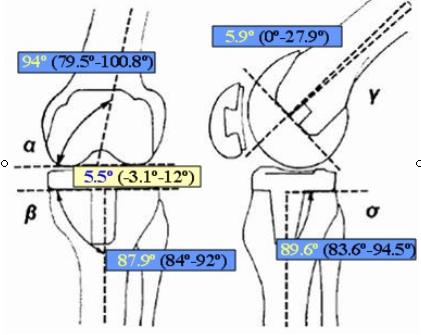
Fig.2. Roentgenographic evaluation. Measurements of knee
alignment (femorotibial angle) and position of components
(position -a-,
angle -g-
of the femoral component and position -b-,
angle -d-
of the tibial component).
Radiographs of 10 knees (48%) showed radiolucent
lines at the bone-cement interface during the follow-up. Nine
knees (43%) had radiolucent lines around the femoral component,
three in zone 1, six in zone 2, one in zone 3 and three knees in
zone 4. Ten knees (48%) had radiolucent lines related to the
tibial component. In the anteroposterior view of the tibial
implant we observed nine radiolucent lines in zone 1, eight in
zone 2, five in zone 3 and seven in zone 4 at the tibial
bone-cement interface while in the lateral view detected eight
knees with radiolucent lines in zone 1, five in zone 2 and one
in zone 3. No relationship was remarked between radiolucency and
variables such as age, body weight, type of component, and
alignment (Figure 3).

Fig.3. Radiographs showed radiolucencies at the
bone-cement interface in tibial and femoral components
Nine
knees (21.4%) underwent revision surgery performed 7.5 years
after the primary joint arthroplasty (range, 2-18 years). Two
knees were revised for clinical symptomatic instability after
three and four-years of follow-up being change to a modular
rotating hinge design. The other seven had revision for PE wear
14 years after surgery (range, 12 to 18 years) in four cases,
aseptic loosening in two cases (4 and 9 years after surgery) and
for pain of unknown source after 23 months of the surgery. There
were no revisions for septic loosening.
Survivorship was calculated using the method of Kaplan and
Meier.[10]
Removal or revision of a component for any reason was set up as
an endpoint. With these criteria, there was a survival rate of
81% at 8 years (Figure 4).
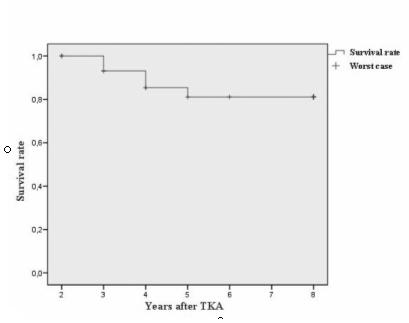
Fig.4. Survival curve with a revision as the end point shows
81% survival rate at 8 years follow-up.
Discussion :
Functional status of rheumatoid patients after total knee
arthroplasty remained far below that of patients with
osteoarthritis treated with knee arthroplasty.[11]
This was believed to be caused by polyarticular involvement of
the disease and the steadily declining functional status than
can occur in the long term.[12]
In our serie, 11 patients underwent surgery in other joints,
however excellent or good results in the Hospital for Special
Surgery score were achieved in 81% of our patients after a mean
follow-up of 7.5 years.
The
pain score and range of motion are usually beyond the influence
of other maladies. In our cases, 18 of 21 knees (85.7%) had no
pain or were slightly painful. Van Loon et al reported that 48
of 52 knees (92%) had no pain or occasional pain.[13]
Malkani et al stated no pain in 70% of knees
[14]
and Laskin warned that knees with low pain score had
malalignment or malpositioning of the components, mainly the
tibia.[15]
While debates within the orthopedic
community focus on issues as the value of preserving the
posterior cruciate ligament, recent studies support the fact
that with modern total knee designs, excellent functional
improvement and long-term prosthesis survivorship should be
expected. Schai et al evaluated 81 patients who had received a
posterior cruciate retaining implant and reported a prosthesis
survivorship of 93.7% after 11 years of follow-up with a mean of
95 points in the Knee Society score.[16]
On the other hand, Laskin and O´Flynn assessed 116 patients with
a posterior cruciate ligament retaining prosthesis and showed a
50% incidence of late posterior instability.[17]
Eleven patients underwent revision surgery because of
instability. In a large multicenter Swedish survey, reviewing
more than 1900 cruciate retaining knee replacements in patients
with rheumatoid arthritis, only 0.5% of revision surgeries were
performed for posterior instability.[18]
Scuderi et al studied cruciate sacrificing and posterior
stabilized total knee arthroplasties and found an overall
survivorship of 97.3% at 10 years and 90.6% at 15 years.[19]
Regarding long term component stability
in relation to the posterior cruciate ligament, an early
predictor of late implant loosening may be the presence of
radiolucencies at bone-cement interface. The prevalence of
radiolucent lines is reported to be between 20% and 60%, the
higher rates observed in studies with more than ten-year
follow-up.[14,20-22]
Uematsu et al studying 616 knees with a maximum follow-up period
of 7 years, reported 7% of radiolucent lines on the femoral side
and 20% on the tibial side.[20]
Eward et al reported that 18% of 124 consecutive cases had
radiolucent lines at the tibial bone-cement interface.[21]
Ito et al described a prevalence of 27.8% at 13 years or more
after surgery in 36 cases.[22]
Malkani et al had an incidence of 60% at a mean of 10 years
after surgery.[14]
Sharma et al for 63 cases informed of 32% of significant
radiolucent lines at 16 years after surgery. In our cases,
prevalence of radiolucent lines was 48% at a mean of 7.5 years
follow-up, similar to other reports in literature.[23]
Whether or not malalignment of the knees influences
clinical results or radiolucent lines are an important fact,
especially in the long term results, it is an evidence that the
prevalence of radiolucent lines was significantly higher in
cases with a varus-positioned tibial component than in those
with neutral placement. Conversely, the incidence of radiolucent
lines around the femoral component was not related with the
placement of the femoral component.[21]
In rheumatoid knees, Laskin indicated that varus positioning of
the tibial component was significantly correlated with
radiolucency at the bone-cement interface in a 10-year follow-up
study.[15]
Infection perhaps is the most important
complication after total knee replacement in patients with
rheumatoid arthritis. Rates of infection have been reported to
be about three times larger than in patients with
osteoarthritis.[24,25]
Reasons for these are multifactorial, but the use of
immunosuppressive drugs, mainly corticosteroids, is the main
factor. Steroids not only influence the immune response system
of the patients, but also have tendency to render the skin
atrophic and easily injured.
Other complication after total knee
arthroplasty apart from aseptic loosening and infection is
peri-prosthetic fracture.[22,26,27]
Restricted range of motion could be a risk factor for
supracondylar fracture of the knee. Nerve palsy, deep vein
thrombosis, skin necrosis, breakage of the metallic tray
[28]
and granulomatosis reaction are also complications that could
appear.[29]
Total knee prosthesis for rheumatoid arthritis and for
osteoarthritis are not similar in terms of the activity of
patients, osteoporosis around the implant, disorders of other
joints, and age of surgery. Hence, the data of follow-up results
and survival rate are not exactly comparable if prosthesis
designs, disease of the population and age at surgery are not
considered.
In
long term studies, the number of patients often decreases
because of death from natural causes. Higher mortality rates
have been registered in patients with rheumatoid arthritis than
in cases of osteoarthritis.[30]
Sharma informed of mortality rates of 23.4%
[23]
and Ito reported rates of 40.8% at 15 years.[22]
In our study four patients had died (14.2%) at the follow-up
evaluation.
Conclusion:
Rheumatoid arthritis concerns about 1% of the population. Most
of the patients with long-standing rheumatoid arthritis have at
least one, and often both knees affected.[31]
When there is joint deformity or cartilage destruction, total
knee replacement is the main therapeutic alternative.
Unycondilar prosthesis and osteotomy do not diminish
inflammation and the constant damage of the residual joint
cartilage of the knee joint. Despite the difficulties related to
the surgery in rheumatoid population, a well-timed,
well-executed total knee replacement has been proven to enhance
quality of life for people with disabling rheumatoid of the
knee.
Reference :
-
Poss R, Ewald FC, Thomas WH. Complications of
total hip replacement arthroplasty in patients with rheumatoid
arthritis. J Bone Joint Surg Am 1976; 58:1130-3
-
Garner RW, Mowat AG, Hazelman BL. Wound healing
after operations on patients with rheumatoid arthritis. J Bone
Joint Surg Br 1973; 55:134-44
-
Fleming A, Crown JM, Corbett M. Early rhematoid
disease. I. Onset. Ann Rheumatoid Dis 1976; 35: 357-60
-
Jacoby RK, Jayson MIB, Cosh JA. Onset, early
stages, and prognosis of rheumatoid arthritis: a clinical study
of 100 patients with an 11-year follow-up. Br Med J 1973; 2:
96-100
-
Chmell MJ, Scott RD. Total knee arthroplasty in
patients with rheumatoid arthritis: an overview. Clin Orthop
1999; 366: 54-60
-
Weinblatt ME. Antirheumatic drug therapy and the
surgical patient. In: Sledge CB, Ruddy S, Harris ED Jr, Kelley
WN, editors. Arthritis surgery. Philadelphia: W.B. Saunders;
1994:669-7
-
Barnes CL. Surgical treatment
of inflammatory arthritis. In: Pellicci PM,
Tria AJ, Garvin K, editors. Orthopaedic knowledge update. Hip
and knee reconstruction. 2. Rosemont: AAOS;2000:3-6
-
Insall J, Ranawat CS, Scott WN, Walker P. Total
condylar knee replacement: preliminary report. Clin Orthop 1976;
120:149-54
-
Ewald FC. The Knee Society total kneee
arthroplasty roentgenographic evaluation and scoring system.
Clin Orthop 1989; 248: 9-12
-
Kaplan EL, Meier R. Nonparametric estimation
from incomplete observations. J Am Statist Assoc, 1958; 53:
457-81
-
Wright J, Ewalds FC, Walker PS. Total knee
arthroplasty with the Kinematic prosthesis: results after five
to nine years: a follow-up note. J Bone Joint Surg Am 1990;
72:1003-09
-
Pincus T. The paradox of effective therapies but
poor long-term outcome in rheumatoid arthritis. Semin Arthritis
Rheum 1992; 21: 2-15
-
Van Loon CJ, Wisse MA, de Waal Malefijt MC. The
kinematic total knee arthroplasty: A 10- to 15 years follow-up
and survival analysis. Arch Orthop Trauma Surg 2000;120: 48-52
-
Malkani AL, Rand JA, Bryan RS, Wallrichs SL.
Total knee arthroplasty with the Kinematic condylar prosthesis:
a ten-year follow-up study. J Bone Joint Surg Am 1995; 77:
423-31
-
Laskin RS. Total condylar knee replacement in
patients who have rheumatoid arthritis: a ten-year follow-up
study. J Bone Joint Surg Am 1990; 72: 529-35
-
Schai PA, Scott RD, Thornhill TS. Total knee
arthroplasty with posterior cruciate retention in patients with
rheumatoid arthritis. Clin Orthop 1999; 367: 96-106
-
Laskin RS, O'Flynn HM. Total knee replacement
with posterior cruciate retention in rheumatoid arthritis.
Problems and complications. Clin Orthop 1997; 345: 24-28
-
Knutson K, Lindstrand A, Lidgren L. Survival of
knee arthroplasties. A nation-wide
multicenter investigation of 8000 cases. J Bone Joint Surg Br
1986; 68: 795-803
-
Scuderi GR, Insall JN, Windsor RE, Moran MC.
Survivorship of cemented knee replacements. J Bone Joint Surg Br
1989; 71: 798-803
-
Uematsu O, Hsu EP, Kelley KM. Radiographic study
of Kinematic total knee arthroplasty. J Arthroplasty 1987; 2:
317-26
-
Ewald FC, Jacobs MA, Miegel RE. Kinematic total
knee replacement. J Bone Joint Surg Am 1984; 66: 1032-40
-
Ito J, Koshino T, Okamoto R, Saito T. 15-year
follow-up study of total knee arthroplasty in patients with
rheumatoid arthritis. J Arthroplasthy 2003; 18: 984-92
-
Sharma S, Nicol F, Hullin MG, McCreath SW.
Long-term results of the uncemented Low Contact Stress total
knee replacement in patients with rheumatoid arthritis. J Bone
Joint Surg Br 2005; 87: 1077-80
-
Poss R, Thornhill T, Ewald FC, Thomas WH, Battle
NJ, Sledge CB. Factors influencing the incidence and outcome of
infection following total joint arthroplasty. Clin Orthop 1984;
182:117-26
-
Wilson M, Kelley K, Thornhill T. Infection as a
complication of total knee replacement arthroplasty. Risk
factors and treatment in sixty-seven cases. J Bone Joint Surg Am
1990; 72: 878-83
-
Figgie MP, Goldberg VM, Figgie 3rd HE, Sobel M.
The result of treatment of supracondylar fracture above total
knee arthroplasty. J Arthroplasty 1990; 5: 267-76
-
Merkel KD, Johnson EW Jr. Supracondylar fracture
of the femur after total knee arthroplasty. J Bone Joint Surg Am
1986; 68: 29-43
-
Scott RD, Ewald FC, Walker PS. Fracture of the
metallic tibial tray following total knee replacement: report of
two cases. J Bone Joint Surg Am 1984; 66: 780-82
-
Dannenmaier WC, Haynes DW, Nelson CL.
Granulomatous reaction and cystic bony destruction associated
with high wear rate in total knee prosthesis. Clin Orthop 1985;
198: 224-30
-
Bohm P, Holy T, Pietsch-Breitfeld B, Meisner C.
Mortality after toal knee arthroplasty in patinets with
osteoarthritis ans rheumatoid arthritis. Arch Orthop Trauma Surg
2000; 120: 75-8
-
Wolfe F, Zwillich SH. The long-term outcomes of
rheumatoid arthritis: a 23-year prospective, longitudinal study
of total joint replacement and its predictors in 1600 patients
with rheumatoid arthritis. Arthritis Rheum 1998; 41: 1072-82
|
|
This is a peer reviewed paper Please cite as
:
Almeida F :
Posterior-Stabilized Total Knee Replacement In Rheumatoid
Arthritis
J.Orthopaedics 2008;5(3)e3
URL:
http://www.jortho.org/2008/5/3/e3 |
|
|


