| CASE
REPORT |
|
Neuropathic Joint Following Spinal
Anaesthesia – A Case Report |
|
Gopakumar T S *, Rajanish R**, Kavitha
E*** Rejith Valsalan****
* Associate Professor in Orthopaedics,
Dept. of Orthopaedics
** DNB Trainee, Dept. of Orthopaedics
*** Post Graduate Trainee Dept. of Anaesthesia
**** Post Graduate Trainee Dept. of Orthopaedics, Medical College, Calicut 673008.
Address for Correspondence:
Dr. Rajanish R
“Sreerangam”,
Kizhuthally,
Kannur – 670018
Phone: +91 9846239349
E-Mail: dr_raj69@rediffmail.com
|
|
Abstract:
Adverse neurological sequelae following spinal
anaesthesia although not common, have been documented in a
number of cases.
We present a case of neuropathic knee joint in a
32 years old female who now presents with dissociative sensory
loss and areflexia on right lower limb, as a result of spinal
anaesthesia complication, leading to the development of syrinx
from T12 to conus.
J.Orthopaedics 2008;5(3)e2
Keywords:
Spinal anaesthesia, neuropathic joint, syrinx.
Introduction:
Neurological complications following spinal
anaesthesia are rare1. They range from anterior spinal artery
syndrome transverse myelitis cauda equina syndrome, chronic
arachnoiditis to complete flaccid paralysis2.
Postulated theories regarding causes of such
complications are direct trauma, chemical irritation and
sepsis3.
We report a case of Charcot’s joint right knee,
following spinal anaesthesia due to the development of secondary
syrinx.
Case Report :
32 years old second
gravida with a history of previous uneventful LSCS, underwent
elective LSCS for the second time under spinal anaesthesia 8
years ago in 1998. Patient was apparently normal before the
procedure. At the time of giving spinal anaesthesia, she
experienced local discomfort and brief shooting pain through
both lower limbs. But adequate analgesia was attained and
surgery was carried out uneventfully. In the post operative
period, the patient failed to regain motor and sensory
perception below the level of umbilicus. Bowel and bladder
functions were preserved. Motor power in both lower limbs
gradually recovered to normal over a period of two years.
Sensory perception over the left lower limb recovered completely
over a period of six months. However on the right side, pain
and temperature sensations did not recover below the T12 level.
Two years ago the patient developed painless, progressive
effusion and deformity of the right knee joint. She also
developed a trophic ulcer on the right foot.
On examination she
was found to have unstable right knee joint with gross effusion
and synovial thickening. Neurological examination of right
lower limb revealed near normal motor power, bilaterally
comparable bulk of muscles, hypotonia with areflexia and
dissociative sensory loss ( pain and temperature) below T12
level. Vibration and proprioception senses were preserved.
Plantar reflex was found to be equivocal on right side.

Investigations:
On investigating the patient haemogram, serum electrolytes,
blood sugar estimations and renal function tests revealed normal
values. Immunological marker for syphilis was found to be
negative. Cerebrospinal fluid study by lumbar puncture was
normal.
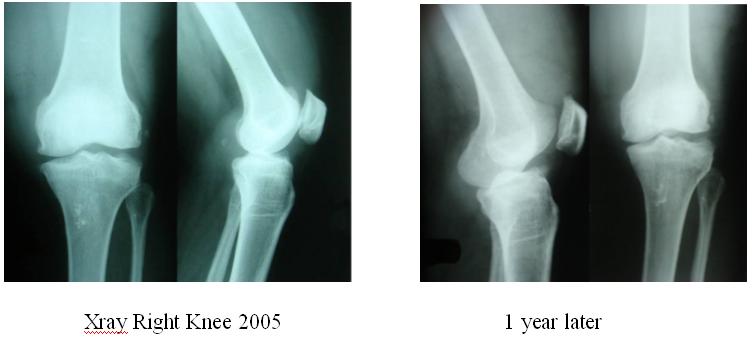
Radiological assessment of right knee joint showed
changes of osteoarthritis with joint space narrowing, subchondral bone sclerosis, large osteophytes and joint
effusion. There was marked destructive and hypertrophic
changes also.
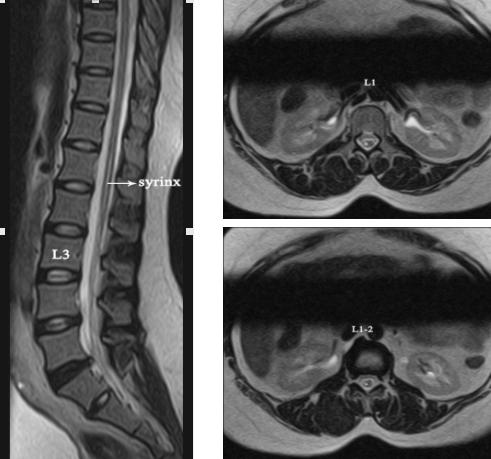
Magnetic resonance imaging of the dorsolumbar spine showed that
the spinal cord ends at the middle of the L2 vertebrae in this
patient; longitudinal hyperintense signals were noted
eccentrically in the cord parenchyma on the right side from T12
till the conus in T2 sequences, which are hypointense in T1
sequences - suggestive of syringomyelia. There was no evidence
of tumour or any other abnormality.
Diagnostic arthroscopy of right knee joint revealed gross
synovial thickening and erosion of articular cartilage.
Discussion :
Neurological complications, though rare, have been documented
following spinal anaesthesia. Serious neurological events like
anterior spinal artery syndrome, transverse myelitis, cauda
equine syndrome, complete flaccid paralysis have occurred.
In the above case scenario, we propose the mechanism
for neurological complications to be direct penetration4 and
consequent injury of the spinal cord leading to the production
of post traumatic synrix5,6,7. Post traumatic syrinx after
spinal anaesthesia can occur due to arachnoid scarring8.
Neuropathic arthropathy (Charcot Joint)9,10 develops
mostly in weight bearing joints. The predominant cause is
diabetes mellitus, but also associated with neuropathic
arthropathy are tabes dorsalis, leprosy, yaws, meningomylocele,
synringomyelia, spina bifida, spinal cord injury, congenital
insensitivity to pain, aerodystrophic neuropathy, amyloid
neuropathy, peripheral neuropathy, secondary to alcoholism and
avitaminosis, peripheral nerve injury, post renal transplant
arthropathy and intraarticular steroid injections.
Although the exact underlying mechanism in the pathogenesis of neuropathic arthropathy remains unclear it is generally believed
to be related to the destruction of afferent proprioceptive
fibres and or subsequent unrecognized trauma to the joint due to
dissociative sensory loss. The loss of sensation to the joint
is followed by severe degenerative changes, osteophyte
formation, articular and subchondral fractures and often
calcification in the surrounding soft tissues. The progression
of neuropathic arthropathy is extremely variable.
Patient is presently treated with orthosis, and
repeated aspirations are being done when joint effusions become
tense. We further plan for complete debridement of all
hypertrophic synovium and arthrodesis if necessary.
Reference :
-
Seigne TD. Aseptic meningitis following spinal analgesia
Anaesthesia 1970; 25: 402-407.
-
Ravindran RS, Bond VK, Tasch MD, Gupta CD, Luerssen TG.
Prolonged neural blockage following regional analgesia with 2-
Chloroprocaine. Anaes. Analg. 1980; 59: 447-451.
-
Usubiaga J. Neurological complications following epidural
anaesthesia. Int. Anaesthesiol Clin. 1975; 3: 69-75.
-
Kane RE. Neurological deficits following epidural or
spinal anaesthesia. Anesth Analg. 1981; 60: 150-161.
-
Umbachi, Heilporn A, Post spinal cord injury syringomyelia
paraplegia 1991; 29: 219- 221.
-
Schurch B, Wichmann W, Rossier AB. Post traumatic
syringomyelia (cystic myelopathy) A prospective study of 449
patients with spinal cord injury. J Neurol Neurosurg Psychiatry
1996; 60: 61.
-
Shannon N, Simon L, Logue V. Clinical features
investigation and treatment of post traumatic syringomyelia J.
Neurol Neurosurg Psychiatry 1981; 44; 35.
-
Youman’s Neurological surgery 4th edn. Vol 2. pg
1090-1092.
-
Campbell’s Operative Orthopaedics 10th edn. Vol 1 Pg 957 –
958.
-
Harrison’s Principles of Internal Medicine
|
|
This is a peer reviewed paper Please cite as
:
Gopakumar
T S : Neuropathic Joint Following Spinal
Anaesthesia – A Case Report
J.Orthopaedics 2008;5(3)e2
URL:
http://www.jortho.org/2008/5/3/e2 |
|
|


