| ORIGINAL
ARTICLE |
|
Pedicle Screw Placement Using
Computer Assisted Navigation |
|
Vikram Chatrath, Vinod Agrawal, Suryaprakash
Nagariya, Pritesh Vyas
Lilavati Hospital, Mumbai, India.
Address for Correspondence:
E- Mail: vchatrath@yahoo.com |
|
Abstract
Level of Evidence : IV Case Series
Aim: This study was done to see the accuracy of placing
lumbar pedicle screw fixation done using computer assisted
navigation.
Methods: Ten cases were of lumbar spine stabilization
were operated using computer assisted navigation surgery using
CT based navigation system. A total of 44 pedicle screws were
implanted in ten patients. All cases underwent post operative CT
scans and x-rays to assess any breach in the pedicle wall.
Results: We found a ninety seven percent accuracy rate in
placement of pedicle screws with regards to wall breach, length
and diameter of screws. Out of 44 pedicle screw insertions, 1
resulted in perforation. There were no intraoperative or
postoperative complications such as occurrence of neurological
symptoms, vascular injuries or wound infections. The average
time for registration and screw placement (4 screws) for one
motion segment was 44.6 (40-70) minutes. Our registration
achieved a mean error of 0.92 (0.7-1.4) mm.
Conclusions: Computer assisted navigation helps in
accurate placement of screws. It also helps in placing thicker
and longer screws with increased surgical confidence. It would
be very useful specially if there are associated deformities,
scoliosis, revision surgeries or for thoracic spine where the
pedicles are small and margin for error minimal. The average
time for registration and screw placement is longer than usual
because of the initial learning curve for this technique.
J.Orthopaedics 2008;5(3)e12
Introduction:
Pedicle screw fixation of the lumbar spine is a standard
procedure. There is still concern over the accurate placement of
pedicle screws 2, 7, 10, 14 with some authors
describing as high as 40% incidence of misplacement. Fluroscopy
guided placement of pedicle screws also increases the radiation
exposure 26, 27, 29 to both the surgical team and the
patient.
All pedicle screw systems share the risk of damage to
adjacent neural structures as a result of improper screw
placement. A computer-assisted system allowing real-time
intraoperative image localization has been used as an adjunctive
tool for instrumentation of lumbar spine posteriorly. This
system helps in accurate placement of pedicle screws and can be
implemented using either a pre-operative CT Scan or CT
free-computer assisted fluroscopy guided system.
Assessment of operative placement of pedicle screws is
typically performed using skiagrams in the posteroanterior (PA)
and lateral projections. It is generally believed that CT
imaging is more accurate than conventional radiography in
determining pedicle screw location, particularly for studying
medial and lateral pedicle perforation 4, 5, 19, 20, 31,
33. The purpose of this study is to assess position of
pedicle screw and pedicle perforation using CT Scans and
standard radiography post-operatively in surgeries performed
under computer assisted navigation.
Material and Methods :
Level of
evidence IV
Eleven patients underwent lumbar spine stabilization using
CT based computer assisted navigation system (Table 1). Of the
eleven patients, 1 died due to unrelated causes three months
after the surgery, so ten patients were available for follow-up.
The mean age of the patients was 49.5 (39-62) years. All the
patients were operated by a single surgeon and were informed
pre-operatively about the use of navigation system. Approval was
obtained by the ethics committee of the hospital.
Computerized tomography scans of the spine were obtained
pre-operatively in 1-mm slices, and the data were imported into
the computer workstations - Kolibri System (BrainLab, Inc.,
Munich
Germany). The indications for the surgery were Spondylolisthesis
with lumbar canal stenosis (4), prolapsed intervertebral disc
with degenerative disc (3), spinal metastasis (1) and
degenerative spondylolysthesis (2).
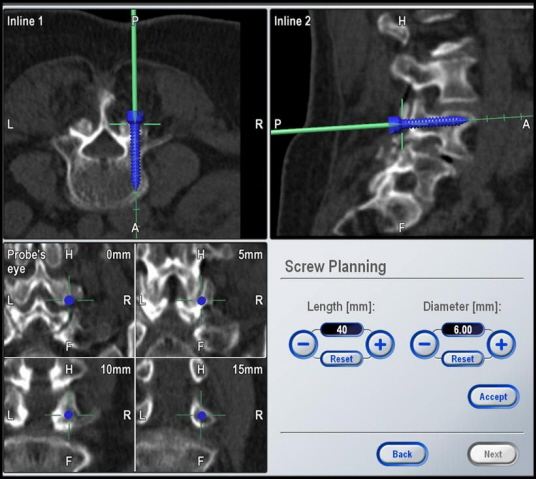
A total of 44 pedicle screws were implanted in ten
patients. The length and diameter of the screws was noted. A
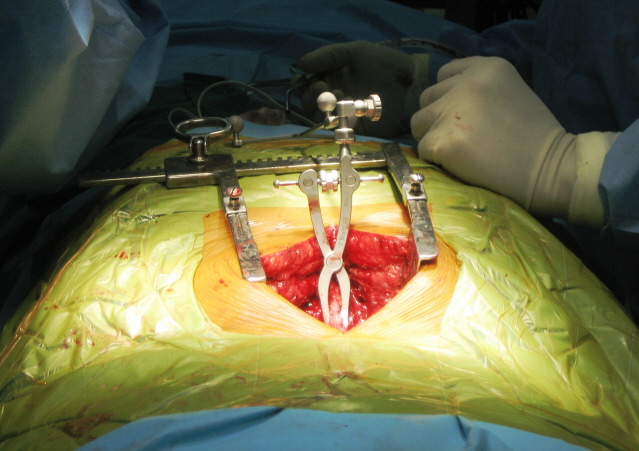
reference frame was attached to the spinous process of each
vertebra and virtual image of vertebra was obtained (Fig -1) and
the registration was performed using the standard techniques
1, 8, 11.
The accuracy of the pedicle screw placement was evaluated
postoperatively by anteroposterior and lateral radiography. All
patients underwent CT scan 3 months after the surgery. All scans
were obtained with a Siemens Sensation 16 Multislice CT (Siemens
Medical Systems Germany), using 3 × 3 mm axial imaging, matrix
520x520, field of view to fit, mA 300, 120 kVp. Windowing was
done to optimize visualization of the screws within the pedicles
(window width 2300 with a center of 600).
We used the system developed by Learch et al 20
to evaluate the position of pedicle screws and any perforations
caused. On the PA radiograph, the position of the tip of the
pedicle screw within the vertebral body was determined by
dividing the body into four equal vertical quadrants with the
center at the spinous process. Quadrant 2 on the PA radiograph
refers to those cases where the screws are correctly placed and
Quadrant 0 refers to screw tip placed lateral to the vertebral
body. On the lateral radiographs the pedicle was divided into 3
equal horizontal zones labeled 1 through 3 from superior to
inferior. All correctly placed screws showed the central portion
of the shaft within zone 2 of the pedicle on both the PA and the
lateral view (Fig-2).
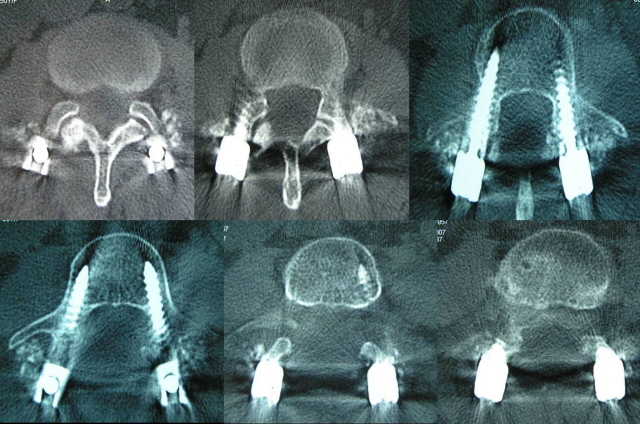
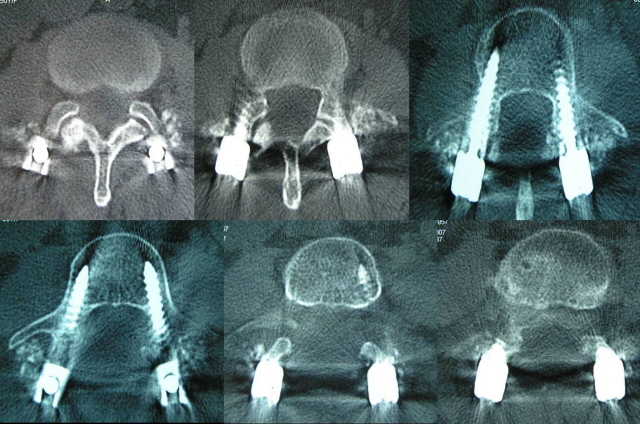
On the CT
scan, lumbar pedicles are imaged on 6 sequential sections. All
correct screw placements were positioned in the midportion of
the pedicle, in either the third or the fourth axial section
through the pedicle (Fig -3).
Results :
Of the 44
pedicle screw insertions, 1 resulted in perforation. (Table 1).
Thus the accuracy in placement of the screws was 97.7 %. The
perforation was seen on the left
lateral pedicle wall at L4 level, but the patient was
asymptomatic post-operatively. No medial or inferior walls were
penetrated in any case. There were no intraoperative or
postoperative complications such as occurrence of neurological
symptoms, vascular injuries or wound infections.
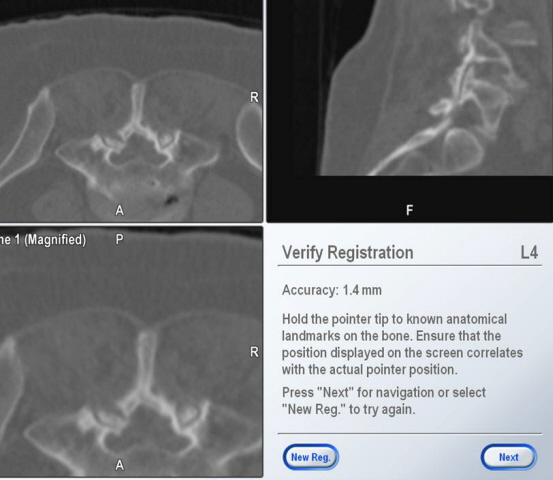
Registration was carried out 12 times.
Registration at one level would usually suffice for a level
above and below, except in 2 cases where the registration had to
be repeated. The average time for registration and screw
placement (4 screws) for one motion segment was 44.6 (40-70)
minutes. Our registration achieved a mean error of 0.92
(0.7-1.4) mm (Fig 4). The diameter of screw placement was 6 mm
(42), 7 mm (2). The length of the screws was 35 mm (5), 40 mm
(33) and 45 mm (6).
Discussion :
Traditionally
spinal instrumentation has been based on intraoperative
localization of anatomic landmarks in concert with the use of
fluroscopy. However, the transverse width and angle of the
pedicle, have revealed critical and significant variability
8, 13, 18, 25, 34. Consequently, faulty placement of
pedicle screw may cause perforation of the cortex and
impingement on adjacent neural structures 22, 23.
Pedicle screw malplacement rates of between 21.1 and 39.8% have
been reported in clinical studies with conventional insertion
techniques and an adequate postoperative CT assessment 2,
7, 19. Infect, in a comparison of different fixation
devices, the highest incidence of symptomatic impingement occurs
with pedicle screws, with nerve root injury or irritation
occurring in a reported 3.2% of cases 30.
Medially, the
pedicle cortex is separated from the dural sac by a thin layer
of epidural fat, which is typically 2 mm in thickness 28.
The nerve root of the corresponding vertebra passes inferiorly
to the pedicle. Because of this, the safest placement of pedicle
screws is within the cephalad portion of the pedicle. If the
superior cortex is violated, there is surrounding fat separating
the pedicle from the exiting nerve root of the vertebra above
10. The most common error is in the placement of the
screw in the saggital plane leading to either medial or lateral
wall perforation 7, 8. The choice of insertion in the
axial direction is variable and surgeon dependent.
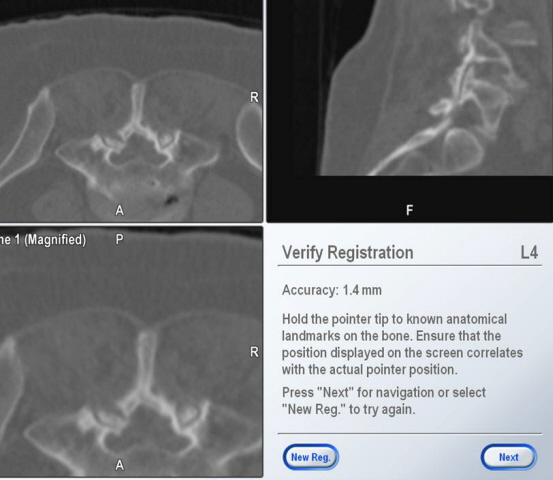
Fig.4
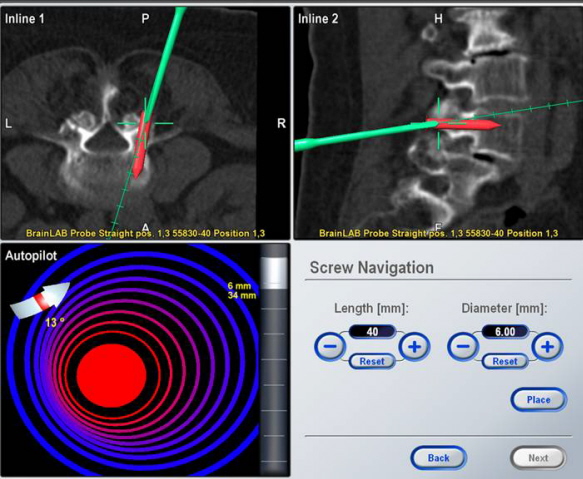
Fig.5
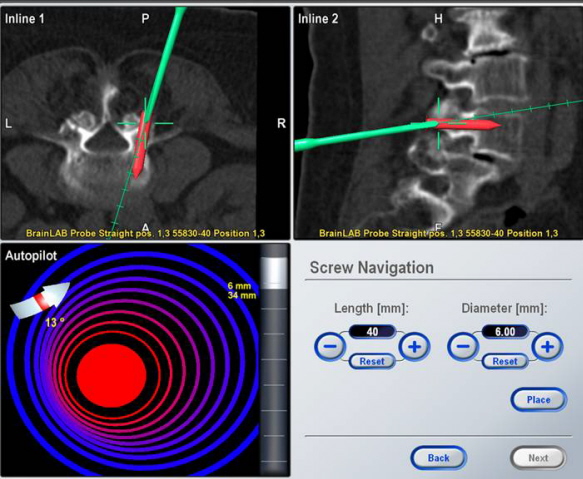
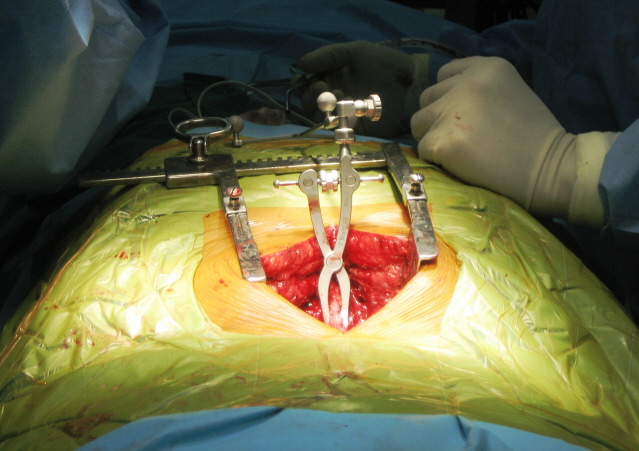
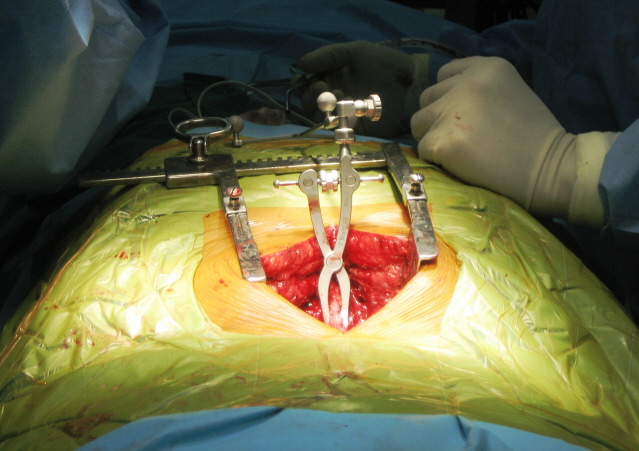
For pedicle screw placement in which minor deviation in the
screw trajectory may result in a pedicle perforation, a CT-based
image-guidance system provides the surgeon with a view of the
pedicle and surrounding structures in multiple planes (Fig 5).
For each pedicle, an ideal entry point and trajectory for screw
placement may be chosen. An image-guidance system is able to
track and provide updated information about the location of the
probe to avoid injury to the spinal cord 3, 15, 16.
Real time imaging also helps to place longer and thicker screws
without the fear of violating the anterior cortex and increased
surgical confidence (Fig 6).
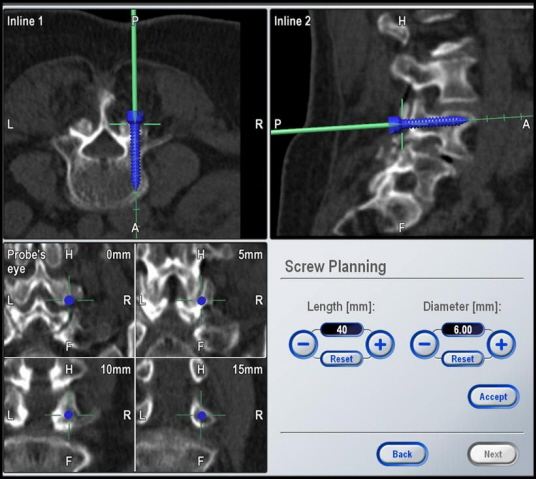
Fig.6
Not all cortex violations cause neurologic injury; minor
violations of the cortex are not uncommon and may be
asymptomatic. However this assumes significance if there are
associated deformities, scoliosis, revision surgeries or for
thoracic spine where the pedicles are small and margin for error
minimal 6, 17, 21, 24, 32.
Another
interesting aspect is the use of navigation in teaching. Hoelzl
et al 12 have evaluated the use of navigation in
training of young spine surgeons and have found it to be very
useful. The three-dimensional view offered by this system
provides a better orientation and also makes it safer to allow
placement of screws by a trainee under supervision. This helps
to eliminate risk and makes the surgical experience practice-
and patient-related. We found it very useful to teach the
residents of our institute in the operating theatre.
Conventionally radiography has been used to asses the
placement of pedicle screws post-operatively. Weinstein et al
31 evaluated the accuracy of pedicle screw placement using
fluoroscopic guided placement of 124 screws into 8 cadaver
thoracolumbar spines. An interobserver agreement rate of 74%
between radiographic assessment and dissection and visual
inspection of screws was obtained. In their study, the
sensitivity of the radiographic evaluation for screw perforation
was only 31%, whereas the specificity was 90%. Low sensitivity
of radiographs for determining screw perforation is unacceptable
because the majority of failed screw placements were classified
as correctly placed on the basis of conventional radiographic
assessment. The system developed by Learch et al 20
to evaluate the position of pedicle screws uses both
post-operative CT scans and radiography for assessment of
pedicle screw position.
The vital
link between achieving a zero perforation rate is registration.
This process helps us to correlate the pre-operative image with
the surgical anatomy. The quality of the preoperative image
needs to be defined more clearly by standardizing the CT scan
images and the methodology across different surgical systems.
This along with variability in registration by different
surgeons needs to be addressed and standardized.
The average
time for registration and screw placement (4 screws) for one
motion segment was 44.6 (40-70). This is longer than usual
because of several factors. Firstly, the initial cases involve a
learning curve for this technique. Secondly the registration
process increases surgical time. However with a CT based system
it is usually possible to use a single level registration for a
level above and below without compromising accuracy. The
unfamiliarity of the scrub nurse and other support staff with
the navigation system was also observed to be a contributory
factor. In a developing country the initial cost of purchasing
the navigation equipment is a deterrent. Moreover, the cost of
pre-operative CT scan further inflicts financial constraints.
Conclusion:
Computer
assisted surgery appears to decrease the risk of pedicle wall
perforation and provides the surgeon with a virtual track for
screw insertion and helps to determine the correct entry point
and trajectory. With further use and acceptance of this
technique it would definitely be of much aid in difficult spine
surgeries.
Reference :
-
Amiot LP, Labelle H, DeGuise JA, et al: Computer-assisted
pedicle screw fixation. A feasibility study. Spine 1995; 20:
1208-1212
-
Castro WHM, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S.
Accuracy of pedicle screw placement in lumbar spine. Spine 1996;
21: 1320-1324
-
Ebraheim NA, Jabaly G, Xu R, et al.
Anatomic
relations of the thoracic pedicle to the adjacent neural
structures. Spine 1997; 22: 1553-1557
-
Farber GL, Place HM, Mazur RA, et al. Accuracy of pedicle screw
placement in lumbar fusions by plain radiographs and computed
tomography. Spine 1995; 20: 1494-99.
-
Ferrick MR, Kowalski JM, Simmons ED. Reliability of
roentgenogram evaluation of pedicle screw position. Spine 1997;
22: 1249-1253.
-
Fras C, Fras M . Accuracy of
Pedicle Screw Placement in Adult Degenerative Lumbar Scoliosis.
Spine J.
2006; 6:5 Suppl 1:158S-159S.
-
Fuch M, Schmid A, Eiteljorge T, Modler M, Sturmer KM.
Exposure of the surgeon to radiation during surgery.
Int Orthop 1998; 22: 153-6
-
Fu TS, Chen LH et al.
Computer
assisted fluroscopic navigation of pedicle screw insertion. Acta
Orthop Scand 2004; 75(6): 730-735
-
Georgis T Jr, Rydevik B, Weinstein J, et al.
Complications
of pedicle screw fixation. In: Garfin SR, ed. Complications of
Spine Surgery. Baltimore, Williams and Wilkins; 1989: 200-210.
-
Gertzbein SD, Robbins SE. Accuracy of pedicle screw placement in
vivo. Spine 1990; 15: 11-14
-
Glossop ND, Hu RW, Randle JA: Computer-aided pedicle screw
placement using frameless stereotaxis. Spine 1996; 21: 2026-2034
-
Hoelzl A, Fischer M, et al.
Navigation of
the spine—a new chance for education and training. International
Congress Series 2003;1256:472–475
-
Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and
lumbar spine in a Chinese population. Spine. 1993;18:1850-1855.
-
Hynes DE, Conere T, Mee MB, Cashman WF. Ionising radiation and
orthopaedic surgeon. J Bone Joint Surg 1992; 74-B; 332-334
-
Kaus M, Steinmeier R, Sporer T, et al.
Technical
accuracy of a neuronavigation system measured with a
high-precision mechanical micromanipulator. Neurosurgery 1997;
41:1431-1437
-
Kim KD, Babbitz JD, Mimbs J. Imaging-guided costotransversectomy
for thoracic disc herniation. Neurosurg Focus 2000; 9 (4): 1-5
-
Kotani, Y, Abumi K ,et al.
Accuracy
Analysis of Pedicle Screw Placement in Posterior Scoliosis
Surgery: Comparison Between Conventional Fluoroscopic and
Computer-Assisted Technique. Spine. 2007;32;1543-1550
-
Krag MH, Weaver DL, Beynnon BD, et al. Morphometry of the
thoracic and lumbar spine related to transpedicular screw
placement for surgical spinal fixation. Spine. 1988;13:27-32.
-
Laine T, Makitalo K, Schenzka D, et al.
Accuracy of pedicle screw insertion: a prospective CT study
in 30 low back patients. Eur Spine J 1997; 6: 402-405.
-
Learch TJ, Massie JB, et al.
Assessment of
Pedicle Screw Placement Utilizing Conventional Radiography and
Computed Tomography: A Proposed Systematic Approach to Improve
Accuracy of Interpretation. Spine 2004; 29(7):767-773
-
Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation
of the thoracic spine in idiopathic scoliosis.
Spine 1997;19:2239-2245.
-
Ludwig SC, Kramer DL, Vaccaro AR, et al.
Transpedicle screw fixation of the cervical spine. Clin
Orthop 1999;359:77-88.
-
Nolte LP, Zamorano LJ, Jiang Z, et al.
Image-guided
insertion of transpedicular screws. A laboratory set-up. Spine
1995;20:497-500.
-
O'Brien MF, Lenke LG, Mardjetko S, et al.
Pedicle
morphology in thoracic adolescent idiopathic scoliosis: is
pedicle fixation an anatomically viable technique?
Spine 2000;25:228-93.
-
Olsewski JM, Simmons EH, Kallen FC, et al.
Morphometry of the lumbar spine: Anatomical perspectives
related to transpedicular fixation. J Bone Joint Surg Am.
1990;72:541-549.
-
Pihlajamaki H, Myllynen P, Bostmon O. Complications of
transpedicular lumbosacral fixation for non-traumatic disorders.
J Bone Joint Surg 1997; 79-B; 183-9
-
Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M.
Radiation exposure to the spine surgeon during fluroscopically
assisted pedicle screw insertion. Spine 2000; 25: 2637-2645
-
Roy-Camille R, Saillant G, Mazel C. Internal fixation of the
lumbar spine with pedicle screw plating. Clin Orthop 1986; 203:
7-17.
-
Schwarzenbach O, Berlemann U, Jost B, Visarius H, Arm E,
Langoltz F, et al.
Accuracy of
computer-assisted pedicle screw placement. An in vivo
computerized tomography analysis. Spine 1997; 22: 452-458
-
Scoliosis Research Society Morbity, Mortality Committee. Member
Survey, 1987.
-
Weinstein JN, Spratt KF, Spenegler D, et al.
Spinal pedicle fixation: reliability and validity of
roentgenogram-based assessment and surgical factors on
successful screw placement. Spine 1998; 13: 1012-1018.
-
Xiong B, Sevastik B, Willers U, et al. Structural vertebral
changes in the horizontal plane in idiopathic scoliosis and the
long-term corrective effect of spine instrumentation. Eur
Spine J 1995;4:11-14
-
Yoo JU, Ghanayem A, Petersilge C. Accuracy of using computed
tomography to identify pedicle screw placement in cadaveric
human lumbar spine. Spine 1997; 22: 2668-2671.
-
Zindrick MR, Wiltse LL, Doornik A, et al. Analysis of the
morphometric characteristics of the thoracic and lumbar
pedicles. Spine. 1987;12:160-166.
|
|
This is a peer reviewed paper Please cite as
:
Vikram
Chatrath :
Pedicle Screw Placement Using Computer Assisted Navigation
J.Orthopaedics 2008;5(3)e12
URL:
http://www.jortho.org/2008/5/3/e12 |
|
|