|
Abstract:
We report a very rare case of bilateral
idiopathic avascular necrosis (AVN) of the hallux metatarsal
heads in a child. This condition is not described in any
previous literature and as such presented an interesting
challenge for management. She was successfully treated
conservatively and at two years of follow-up, the patient
reported that her symptoms had resolved.
J.Orthopaedics 2008;5(2)e6
Keywords:
Avascular necrosis, metatarsal head, children
Case Report:
A
13-year-old girl was referred by her general practitioner with a
two-month history of pain in both big toes. This pain caused her
a great deal of discomfort, was aggravated by walking and
prevented her from undertaking any sporting activities. She was
otherwise fit and well with no significant past medical history
and no report of any similar problems in her family.
Examination revealed hallux rigidus affecting both big toes,
worse on the left. Dorsiflexion is about 15 degrees on the left
and 20 degrees on the right with discomfort at the extreme range
of passive movements. All other joints of the feet were normal
on examination.
Radiographs of the feet showed findings consistent with
avascular necrosis, namely, flattening of the metatarsal heads
(being more pronounced on the left), with two small subchondral
cysts and dorsal osteophytes (Figures 1a&b). Haematological
investigations were normal. No further imaging was planned, as
the diagnosis was conclusive on the radiographs 1,2

Figure 1a Radiographs of both feet at presentation

Figure 1b – Lateral views at
presentation
She
was treated conservatively with medial arch support by foot
orthoses, non-steroidal anti-inflammatory drugs and was reviewed
on a regular basis for two years. The symptoms gradually
improved, as did the appearance of the radiographs (Figure 2).
The osteophyte on the left was thought be limiting the full
range of dorsiflexion and cheilectomy was offered to the
patient. However, as her symptoms had improved significantly
she opted to defer surgery at that time.

Figure 2 at six months follow up

Figure 3 at one year follow up

Figure 4a
at two years follow up AP views
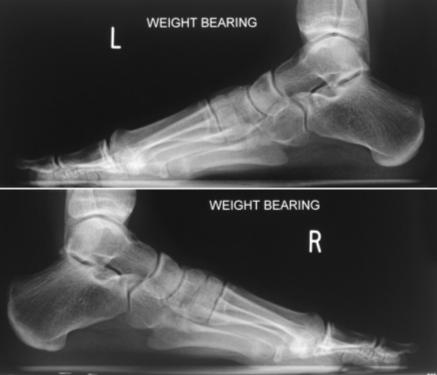
Figure 4b two years follow up lateral
views
At one year of
follow up her symptoms had improved although she had persistent
limitation in dorsiflexion to about 10 degrees (Figure 3).
X-rays at that time showed radiological improvement, however the
osteophyte and cyst remained. At two years of follow up she is
asymptomatic with minimal limitation in dorsiflexion. The
osteophytes persisted but given the fact that she was
asymptomatic, she declined cheilectomy (Figures 4a&b).
Discussion:
A
wide range of aetiologies including trauma, medications,
iatrogenic, infection and idiopathic can cause avascular
necrosis of the metatarsal heads3. It most commonly
occurs in the talus, navicular bones and also the second and
third metatarsal heads. It occurs more frequently in adults,
being extremely rare in children. It has only been described
once in the first metatarsal of a child 4. A Medline
search revealed no cases of bilateral avascular necrosis of the
first metatarsal heads in children.
Symptomatic AVN of the first metatarsal head is an extremely
infrequent condition. Its rarity makes standardisation of the
treatment impossible. Easley and
Kelly suggested that shoe
modification and change in activity may suffice, but in severe
cases joint debridement and metatarsal head decompression may be
indicated. In extremis with severe head collapse, joint
arthrodesis may be an option5. Fortunately, this
patient improved with medial arch support and we hypothesise
that the orthoses acted by relieving pressure on the metatarsal
heads, preventing further collapse and allowed bone remodelling.
Reference :
- Brody AS, Strong M, Babikian G, et
al: Avascular necrosis: early MR imaging and histologic findings
in a canine model, AJR 157:341-345, 1991.
-
Berquist TH, Welch TJ, Brown ML, et al : Bone and soft
tissue ischaemia. In Berquist TH editor: Radilogy of the
foot and ankle, New York,1989 Raven Press, pp 316-348.
-
Easley ME, Kelly IP: Avascular necrosis of the hallux
metatarsal head. Foot and ankle clinics, Foot-Ankle-Clin, Sep
2000, vol. 5, no. 3, p. 591-608
-
Souverijns G, Peene P, Cleeren P, Raes M, Steenwerckx A:
Avascular necrosis of the epiphysis of the first metatarsal
bone. Skeletal Radiol (2002) 31:366-368.
-
Easley ME, Kelly IP Avascular necrosis of the hallux
metatarsal head Foot Ankle Clin. 2000 Sep;5(3):591-608.
|




