| ORIGINAL
ARTICLE |
|
Biologic Distraction and Maintenance Of Disc Height In Lumbar Disc
Disease With A Different Technique: A Clinical and Technical
Study. |
|
Gopinathan Patinharayil*, Anwar Marthya*,
Chathoth Meethal Kumaran*, Chang Whan Han*, Dinesh SunnyVeliath*,
Sibin Surendran*, C V Krishnakumar*
*
Department of Orthopedics, Medical College, Calicut,Kerala,
India
Address for Correspondence:
Dr Gopinathan P
Department of Orthopedics, Medical College,
Calicut,Kerala, India |
|
Abstract:
Improvements in spinal instrumentation system has been the
rule of current practice, recently interspinous spacers has been
used to treat lumbar disc disease. This sytem relies on the
principle of distraction in the interspinous area with indirect
decompression of the roots by enlarging the intervertebral
neural foramen.
We studied the results of a similar principle but using a
different system. We analyzed the role of biologic distraction
and global fusion, with maintenance of the disc space using
Modified Quasi-Claw technique, in lumbar spine for the treatment
of chronic lumbar disc pathology. The modified Quasi-Claw makes
use of a distraction claw with supralaminar hooks below and
infralaminar hooks above with biologic distraction applied
between them. We conducted a prospective study in a series
comprising 70 patients (142 segments) with lumbar disc pathology
with an average follow up of 2.5yrs. Average preoperative
Oswestry disability index was 74.22 and Visual analogue
scale(VAS) score was 68.12. Biological distraction was achieved
using the principle of Modified Quasi-claw and fusion achieved
using posterior lumbar interbody fusion (PLIF) with minced iliac
crest graft along with posterolateral fusion (global fusion -
360˚ fusion). Average post operative Oswestry disability index
was 26.64 and VAS score was 14.32 respectively which was found
to be statistically significant (p<0.01 ). Biological
distraction restores disc height, helps in root canal
decompression by increasing the size of intervertebral foramen,
improves the load bearing ability of anterior ligaments and
muscles and helps in maintaining the spinal balance. It also
stabilizes the spine by avoiding the abnormal intrinsic
instability between the motion segments. The authors consider
that biological distraction using the principle of Modified
Quasi-Claw with PLIF and posterolateral fusion in the treatment
of chronic lumbar disc pathology is a novel concept with a good
outcome.
J.Orthopaedics 2008;5(2)e5
Keywords:
Biologic distraction; Modified Quasi Claw; Posterior
lumbar interbody fusion (PLIF); Lumbar segmental instability;
functional spinal unit.
Introduction:
The management of chronic disabling low back pain due to lumbar
disc disease has always been a controversy in modern
orthopedics. Several treatment methods have been described but
none of them have given satisfactory results. Hence there has
always been a quest for newer techniques in this field. We
describe a new technique with good and reproducible outcome in
the treatment of Lumbar disc disease.
Crock H V1 described internal disc disruption. The
abnormality in the internal architecture of the disc could cause
mechanical back pain and referred pain. The outer third of the
annulus of the intervertebral disc has nociceptive capability
and this could account for discogenic back pain due to internal
disc disruption 2, 3, 4.
Pedicular screws used to achieve posterior lumbar interbody
fusion (PLIF) has the disadvantage that the graft should be
locked in compression. The compression further narrows the
intervertebral neural foramen and the patient may still be
symptomatic. So distraction is more biologic in the lumbar
spine. The pedicular screw introduction invariably needs
radiologic imaging. In this technique biologic distraction is
applied to the posterior complex which is more physiologic since
the tension surface of the spine is anterior complex when the
spine is considered as a single unit. The Quasi-claw does not
need imaging for introduction and is quick with minimum
operating time. This study attempts to delineate an easier and
more biologic method of achieving PLIF with out imaging.
Several articles 5,6,7 describe treatments using
anterior lumbar interbody fusion (ALIF) and posterior lumbar
inter body fusion(PLIF) with instrumentation. Posterior lumbar
interbody fusion (PLIF) 5,8,9 offers several
advantages – it restores disc height, maintains root canal
dimensions by increasing the size of the intervertebral neural
foramen. It also restores the load bearing ability of anterior
ligaments and muscles, helps in maintaining the spinal balance
and in maintaining lumbar lordosis. But with traditional method
of compressing the graft in the disc space there is an inherent
risk of narrowing of the disc space and the intervertebral
foramen especially when the graft collapses.
PLIF also helps in stabilization of unstable functional spinal
unit. The results of PLIF with instrumentation has been good.7,10,11,12,13,14.The
transverse diameter of neural foramen at the disc level of L5-S1
motion segment is around 7 mm. The diameter of the L5 root is
around 7mm 15. This creates a critical area through
which the root escapes. Any reduction in disc height further
reduces the transverse diameter and results in compressive
radiculopathy. So the only method to address this problem is by
maintaining the disc height and increasing the transverse
diameter of the intervertebral neural foramen to decompress the
root. This can be achieved by a constant biologic distraction
using Quasi-claw.
The currently available segmental instrumentation and bone
grafting have helped in achieving posterior intertransverse and
posterolateral fusion with results comparable to that of PLIF
16, 17, 18. But these studies were done on patients
with different pathologies and different methods of treatment.
Facetectomy was always a part of PLIF with the use of
tricortical grafts. But in this study no facetectomy was done,
and minced iliac crest graft were used instead of tricortical
iliac crest graft. The disc space was maintained by posterior
biological distraction and instrumentation.
Quasi Claw technique for spinal segmental stabilization is
achieved by all hook instrumentation. The supralaminar hook is
inserted over the inferior lamina and the infralaminar hook is
inserted under the superior lamina of the adjacent vertebra.
This technique stabilizes a single motion segment. In modified
Quasi Claw technique two motion segments are stabilized instead
of one. In modified Quasi Claw technique supralaminar hook is
inserted over the inferior lamina and infralaminar hook is
inserted under the superior lamina of the vertebra one level
above the adjacent vertebra.
Aim:
To determine the effectiveness and evaluate the outcome of PLIF
with biological distraction and posterolateral fusion (global
fusion) in the treatment of lumbar disc disease using a
different technique.
Material and Methods :
The study was approved by the institutional ethics
committee. Informed consent was obtained from all the patients.
We studied seventy cases of
symptomatic Lumbar disc disease operated between June 2000 and
December 2005. All the selected cases were in the age group of
30 to 73 years, irrespective of the gender. Average age at the
time of operation was 59 ± 7.6yrs. All the cases
underwent PLIF with biological distraction using posterior
instrumentation and posterolateral fusion. They were followed up
for an average period of 2.5 years. A total of 142 segments were
fused (Table1,). All the cases were performed by the same
senior surgeon (PGN).
Radiological involvement of intervertebral disc were classified
according to Saraste’s classification 19
Stage IA: Normal disc height without dehydration
Stage IB: Normal disc height with dehydration
Stage II: Disc height decrease by less than 50%
Stage III: Disc height decreased by at least 50%
Stage IV: Disc height obliterated (with or without instability)
Potential risk factors for achieving fusion like previous failed
fusion, heavy smokers (more than 1 packets of cigarette per
day), heavy manual laborers, fusion of more than two motion
segments, instability, listhesis, excess weight (more than 40 Kg
in excess of predicted weight) were specifically noted. Patient
data about age, sex, walking distance, working capacity, current
employment, smoking, VAS(visual analogue scale) and Oswestry
disability index were collected before and after surgery.
Preoperative investigations included plain X-rays, stress X-rays
and MRI in all patients. . Lumbar segmental instability was
defined as a motion greater than 4 degree of sagittal rotation
or angulation and translation of more than 4 mm 15
The inclusion criteria for the patients were:
-
Patients with
grade III and grade IV stages of Saraste19 of symptomatic
lumbar disc disease in whom conservative treatment has failed.
-
Only patients
with minimum two adjacent motion segments are included.
-
Patients with
grade I listhesis (degenerative).
-
Patients with
symptoms of lumbar segmental instability confirmed
radiologically.
-
Previously
operated symptomatic patients, who had undergone spinal
fusion, decompression and discectomy without significant
symptomatic relief.
-
Patients with
symptomatic psuedo-arthrosis, from previous un-instrumented
surgery.
Exclusion criteria
were,
-
Severe spinal
canal stenosis.
-
Single level Disc
disease irrespective of grade of disc degeneration.
-
Infection.
-
Trauma.
-
Tumour.
-
Previously
instrumented fusion.
The union was probable when bony trabecular continuity was not
clear, and there was less than 4-degree mobility between
adjacent fused segments. Nonunion was defined as clear gap and
motion greater than 4 degree of sagital rotation or angulations
and translation of more than 4 mm 15. But the presence of
instruments will definitely hinder this interpretation. The
preoperative and postoperative disc height was measured in all
cases in lateral view midway between the anterior and posterior
longitudinal ligaments.
Patient data about
age, sex, walking distance, working capacity, current
employment, smoking, VAS and Oswestry disability index were
collected before and after surgery.
Clinical improvements were noted on the basis of improvement of
back pain and working capacity. Follow up was done at 3 months
and there after at regular intervals of 6 months
Clinical improvements were noted on the basis of improvement of
back pain and working capacity. Follow up was done at 3 months
and thereafter at regular intervals of 6 months.
Out of 142 segments fused, 100
segments had grade IV and remainder had grade III degeneration.
Disc involvement according to the spinal levels is shown in
Table2. 68 patients had adjacent one level disc disease and two
had three level disc disease. Single level disc diseases were
not selected.
Adjacent segments, which were abnormal in the form of Grade III
or IV disc disease,
were included in the fusion mass to prevent post fusion
symptoms. Four patients had Grade IV disc degeneration with
grade I listhesis, all were at L4-L5.In all these patients
reduction could be achieved with the method described. Two
patients were previously operated cases for grade IV disc
degeneration at L4-L5. Thirty two patients had paraesthesia or
sensory deficit. Radiculopathy was present in 10 patients in
the form of L5 or S1 root lesion. Tone and reflexes were normal.
The average follow up period was two and half years (between two
to three years). Out of 142 segments, 132 levels had clinico-radiological
correlation. 10 segments (in the double level group) had
atypical pain, which had grade IV disc degeneration changes at
adjacent segments and so adjacent levels were included in the
fusion mass. All segments with grade IV degeneration had
radiological signs of Lumbar segmental instability (LSI).
Table:1
|
|
L3-L4
|
L4-L5
|
L5-S1
|
Total
|
|
Grade III |
0 |
27 |
15 |
42 |
|
Grade IV
|
2 |
36 |
62 |
100 |
Total
|
2 |
63 |
77 |
142 |
On doing the Chi square test, a significant relationship (at 5%
level) was seen between grade IV disc degeneration and L5-S1
level.
Table 2:
Statistical
analysis
Statistical analysis was performed by using Paired t-test with
using SPSS for Windows (version 12.0, SPSS, Chicago, IL).
Comparisons between preoperative and postoperative disc
height,VAS, Oswestry score and grade of degeneration and spinal
level measurements were made using the Paired t-test. The values
were summarized as mean ± standard deviation. A p value of <
0.05 was considered significant.
Surgical Technique:
Posterior lumbar interbody fusion (PLIF) was done through a
midline posterior approach under general anaesthesia in the
lateral decubitus position. Laminectomy was performed, but
facetectomy was not done in any case. Discectomy was done in
all cases and end plates prepared till bleeding subchondral bone
was exposed. The nerve roots were retracted and protected. All
hook system was used in all the patients. Posterior
instrumentation with Modified Quasi Claw with short segment
stabilization was done using indigenously made supralaminar and
infralaminar claw.. The instrumentation consisted of
supralaminar and infralaminar narrow hooks, positioned in the
superior and inferior laminae after decompression.. The rods
were contoured to maintain the lumbar lordosis. Instead of
tricortical iliac crest grafts, minced iliac crest grafts were
packed through the hole made for removal of the disc. Disc
height was maintained by biological distraction and packing the
disc space with bone grafts. Autologous iliac crest grafts were
used in all patients. Maintenance of the disc space increased
the size of the intervertebral foramen and this indirectly
decompresses the nerve root (Fig1,2). Posterolateral fusion was
done through subperiosteal approach, and the bed of the graft,
prepared by subperiosteal dissection through the transverse
process and through the remaining lamina and spinous processes.
Inter facetal fusion was achieved without facetectomy, by
exposing the subperiosteal region of superior and inferior
facets and bridging them with autologous iliac crest graft.
Radiologic assessment for integrity and placement on the
implants were done on the table before closure of the wound.
Postoperatively all patients were mobilized on the 3rd
day on a Knight Taylor’s brace. Postoperative stress x-rays
where taken in all patients after 8 weeks. The criteria for
fusion was trabecular continuity8.All the levels
fused when there was less than 4 degree mobility as measured by
sagittal rotation angle or less than 4 mm translation as
measured as sagittal translation distance.
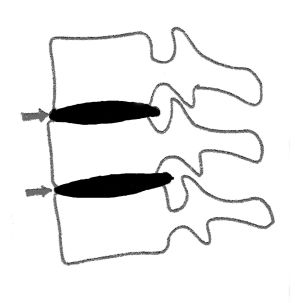
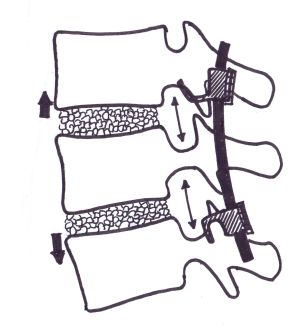
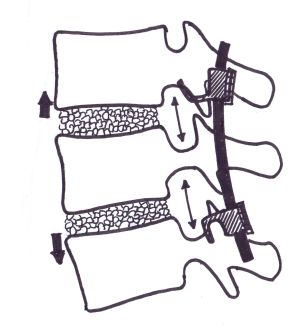
Fig1 and Fig2 :Diagrammatic representation of biologic
distraction with maintenance of disc height and indirect
decompression of the nerve root by the enlargement of the
intevertebral neural foramen.

Fig 3 : Preoperative radiogram showing Grade 1 lumbar
spondylolisthesis at L4-L5 with unequal and also reduced disc
height at L4-L5.

Fig 4 :Post operative radiogram showing normal disc
height and parallel end plates with reduction of
spondylolisthesis.
Results :
Mean VAS was improved from 68.12 to 14.33 in this study. The
range of VAS was 15-80 preoperatively , while post operatively
it was 10-20. The average reduction in VAS was 48.5 % (Table 3).
Average preoperative Oswestry disability index was 74.22 and
post operatively was
26.64 (Table 4). The range was from 60-88 preoperative and
20-36 post operative so the reduction in disability was 49%.
Since the intervention involved a single variable with paired
measurements in each subject the paired students t test
was used as the test of statistical significance. This was
statistically significant with the p-value <0.01 .So there was
significant statistical improvement in Oswestry score (p<0.05%).
There was 4-fold increase in walking distance. Age at the time
of operation was 59 ± 7.6 yrs. The range being 30 to 73 yrs. The
average operation time was 101.8 ± 50 mts and the average blood
loss was 633 ± 25.4 gms.
Excellent correction of disc
height could be achieved post-operatively (Fig3,4). Average
preoperative disc height was 4.72 ± 1.49mm and post operative
was 9.81 ± 2.19mm with an average increase of 5.12mm.(Table 5)
Table 3: VAS Score (n=70)
|
|
Preoperative |
Postoperative |
|
Mean |
68.12 |
14.33 |
|
Std. Deviation |
9.89 |
2.49 |
p value < 0.01
Table 4 : Oswestry Score(n=70)
|
|
Preoperative |
Postoperative |
|
Mean |
74.22 |
26.64 |
p
value < 0.01
Table5 : Disc Height (n=142)
|
|
Preoperative(mm) |
Postoperative(mm) |
|
Mean |
4.72 ±
1.49mm |
9.81 ±
2.19mm |
Twelve patients were symptomatic even after surgery. Of these
twelve, eight patients had low back pain, 4 patients had leg
pain at latest follow up. Out of these 12 patients,10 patients
said their symptoms improved after surgery, but 2 patients had
same symptoms even after surgery.
None of the patients had nonunion. 4 patients had doubtful
interbody fusion but had demonstrable posterolateral union and
the sagital translation less than 4mm, sagital angulation less 4
degree. 32 patients returned to their original duties. Twenty
two patients returned to light duties after surgery. There was
an improvement of 77% in working ability according to Oswestry
scale.
Four patients developed urinary tract infection, treated
successfully with antibiotics. Two patients had delayed wound
healing and persistent iliac crest pain for six months, both
were known diabetic patients. Two cases had paralytic ileus,
which responded to treatment.
Discussion:
It is always desired that a comprehensive approach is a must in
the management of chronic disc disease with low backache (LBA).
But the complexity of the problem puts the treating surgeon in
a difficult situation. Morgan FP et al 20 drew
attention to the association between annular tears, radiographic
instability and LBA and the use of flexion extension views in
diagnosing lumbar segmental instability. Kirkady Willis21
et al defined stages of instability and focused on
anteroposterior and lateral bending radiographs in chronic
lumbar disc disease. They described three stages of disc
degeneration.
-
Stage I:
circumferential and radial tears in the disc annulus and
localized synovitis with hypermobility of facet joints.
-
Stage II:
characterized by internal disruption of disc, progressive disc
resorption, degeneration of facet joints with capsular laxity,
subluxation and joint erosion leading to instability.
-
Stage III :
marked by osteophytosis and spinal stenosis, where the body
tries for stabilization.
Frymoyer
JW22 et al defined the basis of mechanical
instability in chronic lumbar disc disease and described that
the disc degeneration can result due to aging.
Leufven 23 et al reported 93% fusion and 73 %
satisfactory outcome using circumferential fusion and 62%
patients had returned to original work. Some other authors
5,6,7,8,10 have reported 70% satisfactory outcome when
PLIF was combined with posterolateral fusion and
instrumentation. Degenerative lumbar segmental instability is a
concern for spinal surgeons even today. Accurate pre operative
identification of each component of the problem, which produces
a particular symptom, should be addressed individually for the
complete relief. PLIF is commonly advocated as a method of
treating mechanical low back pain including LSI (Lumbar
Segmental instability) with 70-80 % fusion rate and patient
satisfaction are reported in literature 1,5,24 and 75
– 90% return to work is also reported. Accelerated degeneration
of the adjacent segments was described in literature.25,26,27,28
Once a particular functional spinal unit is fused, more stress
occurs at the adjacent spinal unit, accelerating degeneration
and Lumbar Segmental Instability.27 Instability in a
particular functional spinal unit starts as sclerosis of the end
plates with disk space narrowing, (Figure 1).
It causes hypertrophy of the ligamentum flavum and posterior
longitudinal ligament. Later on there is translation listhesis
and angulations that indirectly narrows the intervertebral
foramen and compresses the root. This will result in spinal
canal stenosis, facet joint arthritis, capsular ligament laxity
of the facet joint with facetal instability resulting in facet
induced pain and discogenic pain. It can also lead to
claudication and neurological deficit (Table 1) from global
spinal instability in a particular functional spinal unit.It is
the surgeon’s duty to intervene at any of these stages to
reverse this cascade of processes, so that the symptoms can be
reversed. Instability should be addressed by instrumentation,
which later on should be taken over by interbody and
posterolateral fusion . Otherwise, the implant will fail in the
long run. Canal compromise should be addressed by
decompression.In this study, stress is given to maintain the
disk height by the technique of jacking up the disk space so
that this will indirectly increase the size of the
intervertebral foramen and decompressing the root, thus
relieving the radiculopathy. Adjacent functional spinal units
are usually abnormal and should be included in the fusion mass
to avoid re operation for LSI at the adjacent functional spinal
unit.The etiology of low backache is often multifactorial,
including organic and nonorganic causes. This study was not
intended to address all of the manifestations of low back pain,
but it was directed at evaluating the efficacy and safety of the
technique of fusion and instrumentations. Chronic low backache
cause prolonged disability, anxiety and discomfort. It is often
difficult to treat such patients because of difficulties in
diagnosis and interpretations of investigations. There is also
an important factor of psychosomatic elements.
Clinicoradiological correlation revealed high intensity zone in
MRI, loss of disc height, end plate changes and grade one
listhesis, which were addressed during treatment14.
Fusion rate was 100%. The assessment was prospective. The work
ability out come was good probably because of better restoration
of disc height, maintenance of lumbar lordosis and better load
distribution through the spine. Nachemson et al 30
discussed the psychological factors in this particular
condition. In this study no attempt was made to assess the
psychological status of patients. Psychological factors do
affect pain, hence patient selection is important. 83% patients
had good outcome in this study. Usually posterolateral fusion
has been advocated for this condition to avoid morbidity
associated with PLIF.17. In this study 100% fusion
rate could be achieved by disc excision and instrumented PLIF
and posterolateral fusion. This eliminates chemical and
mechanical sources of pain associated with internal disc
disruption. If the disc is not removed, it remains as a source
of continuous pain. Correction of instability and removal of
biological substances from degenerated disc eliminates the
nociceptive stimulation of outer annulus 2,3,4
The motion segment is a three joint structure with two facet
joints and the intervertebral disc 30. PLIF should be
supported by posterior instrumentation. PL fusion will enhance
fusion at PLIF. The current study shows 4 patients with doubtful
PLIF, but had good PL fusion.
This novel technique has the advantage of extreme technical
simplicity, it does not need imaging for placement. In
degenerative lumbar disc disease, the traditional method of
pedicular screw fixation carries risk of implant failure due to
osteoporosis and lack of adequate screw purchase. The severity
of osteoporosis is most marked initially in the vertebral
bodies. The posterior complex is spared from osteoporosis. This
technique makes use of posterior complex for implant fixation
which is more biomechanical stable. The traditional method of
pedicular screw involved compression using pedicular screws
.This will result in narrowing of intervertebral foramen and
results in radicular pain. This technique uses the technique of
biologic distraction which widens intervertebral foramen and
reduces the chances of radicular pains. If the lumbar spine is
considered as a single unit, the anterior complexes form the
tension surface and the posterior complex forms the compression
surface. Compression of the tension surface is the well accepted
method of stabilization of any bone. So compression of the
posterior complex with pedicular screws is biomechanically
incorrect. Biologic distraction of the posterior complex
indirectly leads to compression of the tension surface i.e the
anterior complexes and is more physiologic. Screw breakage is a
known complication with the traditional method but not a problem
with this technique. The disadvantage of this technique is that
over distraction and lack of proper contouring of the rod leads
to flat back syndrome but adherence of the correct technique
negates this problem. Hook dislodgement could be a problem but
correct selection of hooks and their perfect placement avoids
such complication.
The traditional method of pedicular screw fixation with
compression to lock the interbody graft has the disadvantage of
narrowing the disc space and intervertebral foramen especially
when there is graft collapse 31. The primary concern
of LSI is radicular pain and pain due to instability. Radicular
pain can be addressed to a certain extent by foraminotomy but
the basic disease process is not corrected. So maintaining the
disc height is of great importance which can be achieved by
biologic distraction and PLIF.
The transverse diameter (from the ligamentum flavum to the
vertebral body and disc) of intervertebral foramen at L4 disc
level is around 7mm. Diameter of L4 root is around 7mm
15,31. So there is a critical area through which root
escapes 12,32. Measuring the cross sectional area of
the canal seems pointless unless only the minimal area is
considered 32 Narrowing of the intervertebral
foramen will further reduce this transverse diameter and result
in radiculopathy.
Tandon etal 13 reported mean reduction in Oswestry
disability index from 51 preoperative to 39-post operative so
there is reduction of disability by 12%. This series shows an
improvement by 25%.
Biologic distraction with instrumentation helps to maintain the
disc height resulting in prevention of compression of nerve
roots in the intervertebral foramen. By maintaining the disc
space transverse diameter can be increased and the root can be
indirectly decompressed. The traditional 31 method
of pedicular screws used to compress the vertebrae together may
reduce the disc height especially when there is tricortical
graft collapse. This will lead to foraminal narrowing and
radiculopathy resulting in radicular pain even after solid
fusion. The good outcome in this study could also be either due
to decompression of the roots or dural sac, or could be due to
short-term nature of this study.
The current study shows that maintenance of disc height (Figure
2) and PLIF along with posterolateral fusion had produced good
clinical outcome. More patients returned to their original work.
PLIF improved the dynamics of lumbar spine and restores lordosis,
reduces biochemical and mechanical factors of pain (Table 2).
PLIF also restores the disc height, which is critical in
achieving good outcome. Thus stability achieved at the end of
fusion aids in good outcome. The facet joints and the annulus
fibrosus, which are the main stabilizers in the axial plane1,14
are only disturbed to the minimum.
Suk et al 33 reported a mean pre-op disc height
of 7.4 ± 5.6 mm which was improved to 9.8 ± 2.6mm. We
obtained a comparable result of average preoperative disc height
as 4.72 ± 1.49mm and post operative as 9.81 ± 2.19mm with an
average increase of 5.12mm.
The global fusion of 100% in this study does not correlate with
the 80% recovery by Oswestry (Table 3) probably due to the
psychosomatic status and multifactorial 30 nature of
the particular problem. Appropriate patient selection after
psychosomatic assessment could further improve the result.
Posterior distraction and instrumentation apply distraction to
the posterior lordotic (concave) side of the lumbar spine, which
is more physiologic than compression of the posterior aspect of
the lumbar spine. Since the rods are contoured to the exact
lumbar lordosis, there is less chance of flat back syndrome.
As long as the amount of distraction is just to maintain the
disc height and within physiological limits it does not seem to
affect the biomechanics of the spine. To the best of our
knowledge, there are no reported studies with use of such an
instrumentation technique to treat the particular group of
patients. But considering the short term nature of the study,
further studies with long term follow up are needed to have for
a more clear-cut analysis.
Conclusion:
The present study has demonstrated that rigid instrumentation
with biologic distraction, using the principle of Modified Quasi
claw; with a short segment stabilization produces good clinical
results in the type of patients with chronic lumbar disc lesions
as detailed in this study. This is achieved by maintenance of
disc height, with indirect decompression of roots along with
global fusion. PLIF, posterior instrumentation and
posterolateral fusion (global fusion) is effective in producing
solid satisfactory fusion rate. Good clinical outcome is
obtained is based on reduction in pain, return to work or
comparable activities. There was significant improvement in
Oswestry score (p < 0.01). The maintenance of disc height is
probably the single most important factor in improving outcome
in such patients.
Reference :
- Crock HV. Observations on the management of failed spinal
operations. J Bone Joint Surg Br.1976;58:193-9.
- Kuslich SD, Ulstrom CL, Michael CJ. The tissue origin of low
back pain and sciatica: a report of pain response to tissue
stimulation during operations on the lumbar spine using local
anesthesia. Orthop Clin North Am.1991;22:181-7.
- Mooney V. Where is the lumbar pain coming from? Ann
Med.1989;21:373-9.
- Yoshizawa H, O’Brien JP, Smith WT, Trumper M: The
neuropathology of intervertebral disc removed for low back pain.
J Pathol.1980;132:95-104.
- Enker P, Steffee AD. Interbody fusion and instrumentation.
Clin Orthop Relat Res. 1994;300:90-101.
- Gertzbein SD, Betz R, Clements D, et al. Semirigid
instrumentation in the management of lumbar spinal conditions
combined with circumferential fusion. A multicenter study.
Spine.1996;21:1918-25.
- Tullberg T, Brandt B, Rydberg J, et al. Fusion rate after
posterior lumbar interbody fusion with carbon fiber implant:
1-year follow-up of 51 patients. Eur Spine J.1996;5:178-82.
- Brantigan JW, Steffee AD, Geiger JM . A carbon fiber implant
to aid interbody lumbar fusion. Mechanical testing.
Spine.1991;16:S277-82.
- Zdeblick TA. A prospective, randomized study of lumbar
fusion. Preliminary results. Spine.1993;18:983-91.
- Brantigan JW, Steffee AD. A carbon fiber implant to aid
interbody lumbar fusion. Two-year clinical results in the first
26 patients. Spine.1993;18:2106-7.
- Franklin GM, Haug J, Heyer NJ, et al. Outcome of lumbar
fusion in Washington State workers' compensation.
Spine.1994;19:1897-903.
- Lee CK, Vessa P, Lee JK Chronic disabling low back pain
syndrome caused by internal disc derangements. The results of
disc excision and posterior lumbar interbody fusion.
Spine.1995;20:356-61.
- Tandon V, Campbell F, Ross ER. Posterior lumbar interbody
fusion. Association between disability and psychological
disturbance in noncompensation patients. Spine. 1999;24:1833-8.
- Vamvanij V, Fredrickson BE, Thorpe JM, et al. Surgical
treatment of internal disc disruption: an outcome study of four
fusion techniques. J Spinal Disord.1998;11:375-82.
- Wesley W. Pake. Applied Anatomy of the spine. Chapter 2. The
spine 4th edition volume 1 W B saunders company 1999 :43-44)
- Lorenz M, Zindrick M, Schwaegler P, et al. A comparison of
single-level fusions with and without hardware.
Spine.1991;16:S455-8.
- Wetzel FT, LaRocca H. The failed posterior lumbar interbody
fusion. Spine.1991;16:839-45.
- Leong JC, Chun SY, Grange WJ, et al. Long-term results of
lumbar intervertebral disc prolapse. Spine.1983;8:793-9.
- Saraste H, Brostrom LA, Aparisi T, et al. Radiographic
measurement of the lumbar spine. A clinical and experimental
study in man. Spine.1985;10:236-41.
- Morgan FP,King T. Primary instability of lumbar vertebrae as
common cause for low back pain. J Bone Joint Surg Br.1957;39:6
- Kirkaldy-Willis WH, Hill RJ. A more precise diagnosis for
low-back pain. Spine.1979;4:102-9
- Frymoyer JW. Low back pain. The role of spine fusion.
Neurosurg Clin N Am.1991;2:933-54..
- Leufven C, Nordwall A. Management of chronic disabling low
back pain with 360 degrees fusion. Results from pain provocation
test and concurrent posterior lumbar interbody fusion,
posterolateral fusion, and pedicle screw instrumentation in
patients with chronic disabling low back pain.
Spine.1999;24:2042-5.
- Agazzi S, Reverdin A, May D. Posterior lumbar interbody
fusion with cages: an independent review of 71 cases. J
Neurosurg.1999;91:186-92.
- Brodsky AE. Post-laminectomy and post-fusion stenosis of the
lumbar spine. Clin Orthop Relat Res.1976;115:130-9.
- Lehmann TR, Spratt KF, Tozzi JE, et al.Long-term follow-up
of lower lumbar fusion patients. Spine.1987;12:97-104.
- Zucherman J, Hsu K, Picetti G 3rd, et al.Clinical efficacy
of spinal instrumentation in lumbar degenerative disc disease.
Spine.1992;17:834-7.
- Whitecloud TS 3rd, Davis JM, Olive PM. Operative treatment
of the degenerated segment adjacent to a lumbar fusion.
Spine.1994;19:531-6.
- Miyakoshi N, Abe E, Shimada Y, et al. Outcome of one-level
posterior lumbar interbody fusion for spondylolisthesis and
postoperative intervertebral disc degeneration adjacent to the
fusion. Spine.2000;25:1837-42.
- Nachemson A, Zdeblick TA, O'Brien JP. Lumbar disc disease
with discogenic pain. What surgical treatment is most effective?
Spine.1996; 21:1835-8.
- Brantigan JW, Steffee AD, Lewis ML, et al. Lumbar interbody
fusion using the Brantigan I/F cage for posterior lumbar
interbody fusion and the variable pedicle screw placement
system: two-year results from a Food and Drug Administration
investigational device exemption clinical trial.
Spine.2000;25:1437-46.
- Farfan.H.F. Mechanical disorders of low back 1973 First
Edition Lea and Friebger Philadelphia page:22-23
- Suk SI, Lee CK, Kim WJ,et al. Adding posterior lumbar
interbody fusion to pedicle screw fixation and posterolateral
fusion after decompression in spondylolytic spondylolisthesis.
Spine.1997;22:210-9.
|
|
This is a peer reviewed paper Please cite as
:
Gopinathan Patinharayil: Biologic Distraction and
Maintenance Of Disc Height In Lumbar Disc Disease With A
Different Technique: A Clinical and Technical Study.
J.Orthopaedics 2008;5(2)e5
URL:
http://www.jortho.org/2008/5/2/e5 |
|
|