|
J.Orthopaedics 2008;5(2)e17
Introduction:
Tubercular arthritis has been reported following prosthetic
joint in the literature1-5 but tubercular osteomylitis around
fracture fixation implants is extremely rare. We are reporting a
case of tubercular osteomylitis of femur after subtrochentric
fracture fixation.
Case Report :
A
38yrs male reported to us with discharging wound over an exposed
plate on lateral aspect of proximal thigh [figure-1]. He had
subtrochentric fracture of femur, which was fixed 2 months back.
The postoperative period was uneventful up to one month, after
which patient developed pain and sinus at operative site. The
size of sinus increased despite multiple antibiotics.
All routine blood investigations including erythrocyte
sedimentation rate was normal. Gram’ staining and acid fast
bacilli staining were negative. Chest x-ray was normal. The
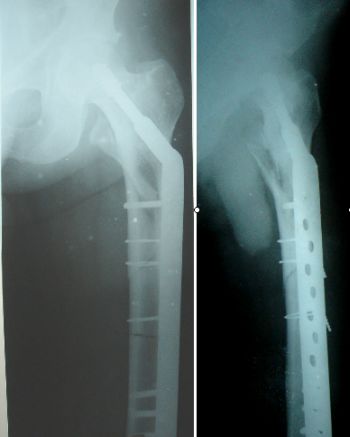
x-ray of femur with hip joint showed subtrochentric fracture
with dynamic hip screw plate fixation with no sign of union and
normal bony architecture [figure-2]. The polymerase chain
reaction [PCR] test for mycobecterial tuberculosis was
positive.
After considering endemicity of tuberculosis along with
clinical evidences and positive PCR for mycobecterial
tuberculosis, the diagnosis of tuberculosis was made. Standard
multidrug antitubercular therapy was given. After 6 weeks, size
of wound decreased with no discharge [figure-3]. After 12 weeks,
the wound was completely healed [figure-4]. At this stage signs
of union were present in x-ray. After 18 weeks, the fracture
line was invisible. Antitubercular therapy was continued for one
year. Recent follow up at 3 years revealed no recurrence of the
infection.

Fig 1: Clinical
photograph at the time of presentation.
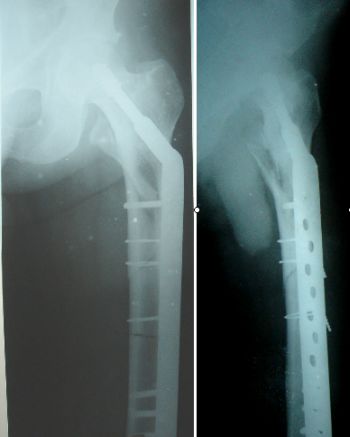
Fig 2:
X-rays, at the time of
presentation.

Fig 3:
After 6 weeks of starting of
antitubercular therapy

Fig 4:
After 12 weeks of starting of
antitubercular therapy.
Discussion:
It is extremely
rare to find tuberculosis causing deep infection around implants
following open reduction and internal fixation of closed
fractures. Very few reports have been published in the
literature6.
Tubercular bacteria can involve
an implant site by hematogenous spread from activation of a
latent distant focus or local reactivation of dormant bacteria
in a previously exposed individual. Major trauma can cause
lowering of both humeral and cellular immunity in its initial
stages7-9. Under such circumstances, reactivation of
a mycobacterium can occur at a latent site, such as lung,
kidney, or mesenteric lymph nodes, resulting in subsequent
seeding at the implant site.1 Local reactivation can be
precipitated by trauma or surgery and has been described as
occurring as long as forty-two years after the initial surgery10.
It seems that any factor that alters the local tissue response
can potentially precipitate this phenomenon. We speculate that
decreased immunity in response to trauma allowed reactivation of
latent bacteria at a distant focus, with subsequent seeding at
the implant site in these patients.
The modern antitubercular
drugs isoniazid, rifampicin, pyrazinamide, and ethambutol are
very effective and safe. There is no osseous barrier in
osteoarticular tuberculosis to penetration of antitubercular
drugs11.
While osseous
tuberculosis as a late complication of the surgical treatment of
closed fracture is atypical and rare, we believe that
tuberculosis should be kept in mind as a possible cause of deep
infection, especially in zones endemic for tuberculosis. In
zones in which tuberculosis is not endemic, patients with
persistent, recalcitrant or atypical infection should undergo
laboratory investigations for mycobacterial infection.
Reference :
McCullough CJ. Tuberculosis as a
late complication of total hip replacement. Acta Orthop Scand.
1977;48:508-10.
-
Spinner RJ, Sexton DJ, Goldner
RD, Levin LS. Periprosthetic infections
due
to mycobacterium tuberculosis in patients with no prior history
of tuberculosis. J Arthroplasty. 1996;11:217-22.
-
Lusk RH, Wienke EC, Milligan TW,
Albus TE. Tuberculosis and foreign body granulomatous reaction
involving total knee prosthesis. Arthritis Rheum. 1995;38:1325-7
-
Wolfgang GL. Tuberculosis joint
infection following total knee arthroplasty. Clin Orthop Relat
Res. 1985;201:162-6.
-
Berbari EF, Hanssen AD, Duffy
MC, Stecklberg JM, Osmon DR. Prosthetic joint infection due to
Mycobacterium Tuberculosis: a case series and review of the
literature. Am J Orthop. 1998;27:219-27.
-
Kumar S, Aggarwal A, Arora A.
Skeletal tuberculosis following fracture fixation. A report of
five cases. J Bone Joint Surg Am. 2006;88:1101-6.
-
Rodrick ML, Wood JJ, O’Manony
JB, Devis CF, Grbic JT, Dermling RH, Moss NM, Saporoschetz I,
Jordon A, D’eon P, Mannick JA. Mechanisms of immunosuppression
associated with severe nonthermal traumatic injuries in man:
production of interleukin 1 and 2. J Clin Imunol 1986;6:310-8.
-
Lyons A, Kelly JL, Rodrick ML,
Mannick JA, Lederer JA. Major injury induces increased
production of interleukin-10 by cells of the immune system with
a negative impact on resistance to infection. Ann Surg.
1997;226:450-60.
-
Browder W, Williams D, Pretus
H, Olivero G, Enrichens F, Vao P, Franchello A. Beneficial
effect of enhanced macrophage function in the trauma patient.
Ann Surg 1990;211:605-13.
-
Johnson R, Barness KL, Owen R.
Reactivation of tuberculosis after total hip replacement. J Bone
Joint Surg Br. 1979;61:148-50.
-
Barclay WR, Ebert RH, Le Roy GV,
Manthei RW, Roth LJ. Distribution and excretion of radioactive
isoniazid in tuberculosis patient. J Am Med
Assoc.1953;151:1384-8.
|