|
Abstract:
Objective: To develop a new method of treating fractures
and nonunion of humeral shaft.
Methods: A nitinol connector named swan-like memory
compressive connector (SMC) was designed. The biomechanics test
included photoelasticity, electrometric method and three
dimensional finite element analysis were employed. In clinical
application, 105 cases of nonunion of a humeral shaft fracture
between 1990 to 2001 were analyzed retrospectively. Among the 95
patients, there were 56 males and 39 females with an average age
of 46.2 years (range from 17 to 71 years). All the nonunions
were managed by open reduction and internal fixation with SMC
and cancellous bone graft. The mean follow-up period was was an
average of 38 months (range from 25 to 81 months).
Results: All nonunion fractures united within an average
of 16 weeks (range 10-26 weeks) and the nonunion sites were
substituted by plate-like bone. At the final follow-up, shoulder
and elbow functions of the operated limbs were all satisfactory.
Conclusions: The SMC provided a new method for fracture
fixation and treatment of bone nonunion for upper limb diaphysis,
and maybe develop a new way to prompt bone healing.
J.Orthopaedics 2008;5(2)e16
Keywords:
Humeral shaft; Fracture; Nonunion; internal fixation;
Introduction:
The incidence of nonunion after humeral shaft fractures is
generally reported as low because of the favorable results of
nonoperative 1 and, on strict indication, surgical treatment
2.Nonunion of the humeral shaft occurs in 2% to 10% of
nonsurgically treated fractures and in up to 15% of fractures
treated by primary open reduction and internal fixation (ORIF)
3-6.Despite advances in the initial management of upper limb
fractures, some result in nonunion, requiring further
intervention. Because the treatment of nonunion is time
consuming and difficult, successful initial fracture management
is important. The treatment of nonunion of a humeral shaft
fractures was considered difficult by Watson-Jones7,and several
operative options have been reported in recent decades 8-12,
including dynamic compression plate (DCP) with cancellous bone
grafting, intramedullary nailing (IM), external fixation,
vascularized bone graft, and on-lay bone-plate augmentation.
Different success rates and complications have been reported for
these options. There are some reports of managing nonunion of a
humeral shaft fracture with DCP and cancellous bone grafting.
Fracture healing is related to its local stress enviroment.
According to wolff’s theory, bones have functional adaptability
to external load and bone structures relate to corresponding
stress. Humerus don’t belong to weight-bearing bone, so how to
provide the shaft an axial anti-shearing, anti-bending and
anti-torsion fixation and at the same time provide stable
biomechanic enviroment adaptive to anatomy and physiology at the
fracture site until bone healing? In August 1990 we designed
nitinol shape memory connector (I、II type), looking like a swan,
and was named Swan-like Memory-pressure Connector(SMC). Untill
August 2001, SMC had been used in the treatment of humeral
nonunion with 105 cases and we got high union rates.
Material and Methods :
Design of SMC
An image of a wet humeral sample was formed with a constant axis
by CT, the thickness of layer was 2 mm with 160 layers. The
pictures were fed to the computer to form the cross section
picture of each layer. Both three dimentional model
establishment and finite element (FE) analysis were based on
Windows XP platform and the major software for FE analysis was
Simpleware2.0 (Exeter, UK). The model was described as a mesh of
three-dimensional ten-node tetrahedral solid elements the whole
humerus were divided into 2729 nodes including 49041 units.In
this research, we presumed that the humeral material was
continuous, well distributed, linearly elastic and same in all
directions, the elasticity modulus was 13400 Mpa when compressed
and Poisson’s ratio was 0.30.
According to the anatomic morphology and biomechanic features of
humerus, we combine the material nickel (50-53%) and
titanium(47-50%), 1.5 to 2.5mm in thickness, producing the SMC.
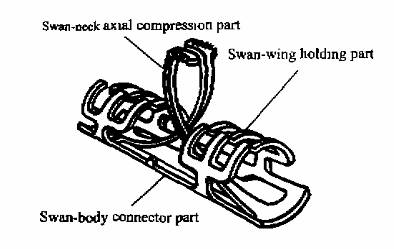
This device consists three parts: swan body, swan neck (axial
compression part), swan wing (holding part). (Fig. 1)The inside
diameter of SMC was 6 to 23mm, inside and diameter length ratio
was about 1:6. Reverting temperature was 33±2.
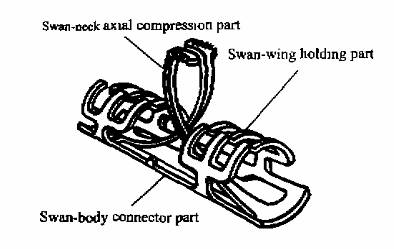
Fig. 1 Diagram of Swan-like Memory Connector used to
treat fracture and nonunion of the humerus
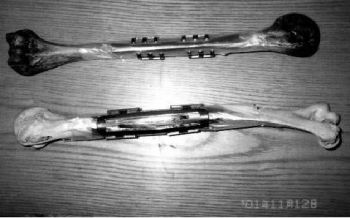
An oversized working model of the initial design idea was
manufactured by one of the authors (Chuncai Zhang) and the
mechanism was shown to work well. However, there was much
development to be undertaken to produce a design of SMC small
enough and strong enough for use in the humerus of a human.
(Fig.2)
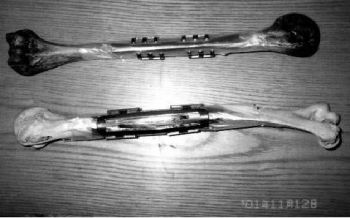
Figure 2:schematic diagram of humerus fixated with SMC
We tested this new fixator with electrical measurment,
biomechanical experiment, photo-elastic and computer simulation
three dimensional finite element analysis 13.
Twenty wet copse adult humerus from a man dying of acute cranial
brain injury were used to make fracture models. The fracture
humerus was fixated with SMC surrounded by prescale to find out
the stress of holding part and compression part. The stress
range of holding part contacting with humerus was 2.42-22.68N,
and the stress in the fracture surface produced by compression
part was about 13.6 Mpa. Axial holding stress of SMC is 98.40N
to 125.05N and longitidual dynamic compressive stress is
152~196N 16.
Principle
of application
At a lower temperature after soaking in cold water, we could
find transformation of SMC, then symmetrily put this fixator to
fracture or nonunion site. Temperature drives transformation
back and develop mechanics action: The memorial reverting stress
of swan body, wing, neck develop axial express stress. The
memorial reverting stress of swan neck develop axial stress at
fracture or nonunion site. All the parts of SMC contribute to a
three dimensional memorial fixation.
Surgical Technique
The nonunion site is exposed and debrided to healthy, bleeding,
viable bone. Any synovial tissue at the nonunion site must be
resected. The intramedullary canal also should be reestablished
because it is an excellent source of osteoprogenitor cells.
Putting SMC into the nonunion site to correct deformity and to
obtain apposition of the bone ends. Liberal use of autogenous
bone graft or another osteoinductive agent is imperative in
atrophic, biologically inactive situations.
For SMC, sterility ice box and 500ml saline of 40-50℃ will be
prepared. First, elastic transformation happened in 0 to 4℃ ice
box and then we outspread swan wing, longer than fracture bone
diameter, outspread swan neck as compression part and swan body
collimating middle point to the fracture position, putting swan
wing together back to fix the fracture stably. According to the
position of swan claw we bore in cortical bone and insert the
swan claw. SMC is reverting at 40 to 50℃ saline and fixation is
finished.
Clinical application
From 1990 to 2001, complete records from 95 patients with
nonunion of humeral shaft were reviewed and analyzed. Nine
patients were excluded before analysis because they were lost to
follow-up. In this study, no bilateral fractures were
encountered, and nonunion was defined as failure to unite the
fracture within 8 months of the initial injury. Among the 95
patients, there were 56 males and 39 females with an average age
of 46.5 years (range from 17 to 71 years). The causes of initial
injury were traffic accidents (n=65), falls (n=20), and direct
contusion by miscellaneous materials (n=10). The initial state
of injury showed that 45 fractures were of transverse type, 39
of oblique type, and 11 of comminuted type. Fifty-five were
mid-shaft fractures, 22 distal-third fractures, and 18
proximal-third fractures. At the acute stage, 25 fractures were
fixed conservatively, 25 with DCP alone, 27 with IM nailing, 12
with external fixation, and 6 with screws. Primary treatment
were done at other institutions in all cases.
Radiographic evaluation of the nonunion found 57 fractures to be
atrophic, and 20 to be hypertrophic, whereas 18 could not be
defined clearly. The timing of treatment was an average of 9
months (range from 7 to 20 months) from the initial trauma. All
patients received the same surgical protocol for treatment of
the nonunion, consisting of removal of the previous implant (in
patients with a previous implant in situ), decortication of the
fracture site, refreshing the fracture site, recanalization of
the intramedullary canal, reduction of the fracture, internal
fixation with SMC, and application of a cancellous bone graft
harvested form the ipsilateral anterior iliac crest. All
procedures were done under general anesthesia by senior staff.
All fractures were reduced as anatomically as possible. Arm
slings were used and range-of-motion exercises were started
immediately after the operation. Any labor with the injured limb
was not allowed until the appearance of bridging callus or
union. No other supplemental fixation, such as cast or brace,
was used after operation. (typical case as Fig.3)
 
Figure 3. Preoperative plain radiograhps of a 50 year-old
man with an nonunion of the humerus and radiograph of the same
patient after appolication of a SMC internal fixation.
After the operation, each case was followed once every 2 weeks
in the first month and once every month thereafter. Each patient
had a special chart with a detailed record of personal data,
mechanism and associated condition of the injury, type and
classification of the fracture and nonunion, management course,
condition and course of fracture healing, and functional
recovery, until the final follow-up. An X-ray check-up was done
at every follow-up visit, and all evaluations were done by
senior staff. Normal union was defined as the appearance of
bridging callus and partial obliteration of the fracture site
within 5 months, delayed union as union evident in 6 to 8
months, and nonunion as no evidence of union in 8 months.
Malunion was defined as varus or valgus deformity ≥15°,anterior
or posterior angulation ≥15°, rotational deformity ≥15°, or
shortening ≥15 mm, compared with the contralateral side. The
follow-up period was an average of 38 months (range from 25 to
81 months).
Results :
All fractures united solidly, and thus, no case needed revision.
The mean operation time was 107 minutes (range from 90 to 160
minutes), and the union time was 16 weeks (range 10-26 weeks).
Based on preoperative and intraoperative findings, the causes of
nonunion in these 95 fractures were soft-tissue interposition
(n=25), poor reduction (n=26), inadequate fixation (n=15),
secondary traumatic insult (n=10), multiple causes (n=10), and
no significant cause (n=9).
The
overall complication rate was 6.7 (7/95) in this series. Three
episodes of superficial infection were noted 1, and all
developed in the upper arm. All infections healed after debredement and antibiotic therapy. No deep infection developed
in this series, transient sensory deficit of the radial nerve
developed in 4 patients 1, all of whom had distal-third
fractures. The injuries seemed to be neuroplaxia due to
inappropriate stretch, and unrelated to the approach itself. All
4 patients recovered completely in 2 to 6 months without any
functional impairment at the final follow-up visit.1No malunion
was noted in this series.
All patients had satisfactory functional results, with neatly
normal shoulder and elbow function, without noticeable pain, and
a full return to pre-injury activities, without pain at the
final follow-up visit.
Discussion :
The
incidence of nonunion of the humeral shaft after operative and
nonoperative treatment ranges between 0.3 and 2.5 percent, with
the exception of two reports with 13 and 14 percent of nonunion
of the humeral shaft after operative stabilization 14. There are
no data on prospective trials of the treatment of humeral shaft
nonunion. Most studies deal with their view of different
surgical techniques, even in rather modest numbers. Studies on
nonunion treatment best documented for compressive plate.
Compression plating of the humeral shaft has been said to cause
stress shielding with compromise of the blood supply and a high
incidence of radial nerve injury, especially with secondary
interventions as nonunion repair after previous osteosynthesis.
Radial
nerve injury after compression plating of the humeral shaft
literature is reported as more than 10 percent 15, with other
studies reporting less than 3 percent 20.In our opinion, an
anteriolateral approach with routine identification and ample
release of the radial nerve well beyond the nonunion ensures an
acceptable rate of radial nerve injury. Preoperatively, several
cases in our series had a combined medial and lateral
positioning of plates, which devitalized the bone and obstructed
union. There were only four cases of a transient sensory deficit
of the radial nerve after surgery.
The mechanical and biologic features of the fracture and
nonunion have a direct bearing on the optimal surgical
treatment. Although a variety of techniques has been described,
including locking intramedullary nails, unilateral external
fixation, compression plate, the preferred treatment is SMC with
the addition of autogenous iliac crest bone graft, and the
success rate has been high. The indication for SMC can be as
follows: upper limb diaphysis open or close transverse and
comminuted fracture, upper limb diaphysis nonunion. The limit of
SMC: the transformation variance of SMC is 8%,it’s the character
of SMC, if break out, SMC will lose its memorial character.
In our opinion, SMC with frequent autogeneous bone grafting
provide consolidation in one operation without serious
complications. The advantages of this new internal fixed
apparatus were as follows: one was the multi-point fixation
which can enhance the stability, keeping the relative stability
of the fracture or nonunion site at early stage, reducing the
motion of the fracture and was good to bone healing. Second was
persistent stable compression at the bone surface. Compression
part can solve the stress shielding effect that existed at the
routine steel plate fixation after the fracture line was
absorbed and promote the healing of the late stage of the
fracture or nonunion.
A point of consideration from bone healing character by SMC
internal fixation: Two months after SMC fixation, fracture
segment were replaced by “anatomic type”-plate bone. We consider
that this bone healing phenomenon of no-solid no-micro, maybe
have something related to the shape memory material and its
dynamic stress or there maybe another unknown bone healing
model?It even requires more explorations.
Reference :
-
D.M.W. Pugh and M.D. McKee, Advances in the management of
humeral nonunion, J Am Acad Orthop Surg 2003; 11: 48–59.
- Atalar AC, Kocaoglu M, Demirhan M, Bilsel K, Eralp L.
Comparison of three different treatment modalities in the
management of humeral shaft nonunions (plates, unilateral, and
circular external fixators). J Orthop Trauma 2008;22:248-257.
-
Ward EF, Savoie FH, Hughes JL Jr:Fractures of the diaphyseal
humerus in Browner BD, Jupiter JB, Levine AM, Trafton PG (eds):Skeletal
Trauma: Fractures, Dislovations, Ligamentous Injuries, ed 2.
Philadelphia, PA:WB Saunders,1998,vol 2,pp 1523-1547.
-
Sarmiento A, Zagorski JB, Zych GA, Latta LL,Capps
CA:Functional bracing for the treatment of fractures of the
humeral diaphysis. J Bone Joint Surg (Am) 2000 ;82,478-486.
-
King AR, Moran SL, Steinmann SP. Humeral nonunion. Hand Clin
2007 ;23:449-56.
-
Tomić S, Bumbasirević M, Lesić A, Mitković M, Atkinson HD.
Ilizarov frame fixation without bone graft for atrophic humeral
shaft nonunion: 28 patients with a minimum 2-year follow-up. J
Orthop Trauma 2007;21:549-556.
-
Watson-Jones R. Fracture and Joint Injuries,6th edition New Yourk Churchill Livingstone,1982,578.
-
Pullen C, Manzotti A, Catagni MA, Guerreschi F. Treatment
of post-traumatic humeral diaphyseal. nonunion with bone loss. J
Shoulder Elbow Surg 2003;12:436-441.
-
Rubel IF,
Kloen P,
Campbell D,
Schwartz M,
Liew A,
Myers E,
et al. Open reduction and internal fixation of
humeral nonunions : a biomechanical and clinical study.
J Bone Joint Surg (Am) 2002;84:1315-1322.
-
Patel VR, Menon DK, Pool RD, Simonis RB. Nonunion of the
humerus after failure of surgical treatment.Management using
Ilizarov circular fixator.J Bone Joint Surg (Br) 2000; 82:
977-83.
-
Chapman JR, Henley MB, Agel J, Benca PJ. Randomized
prospective study of humeral shaft fracture fixation:
intramedullary nails versus plates. J Orthop Trauma
2000;14:162-166.
-
Hormcek FJ, Zych GA, Hurson JJ, Malmin TI. Salvage of
humeral nonunion with onlay bone plate allograft augmentation.
Clin Orthop 2001; 386: 203-209.
- Su jiacan,Cao honghai, Wang Ruiguan,Zhang Chuncai.
Biomechanical feature measurement of Swan-like memory
compression connector.Chinese Journal of Clinical Rehabilitation
2003; 20 :182-184.
- Heim D, Herkert F, Hess P, et al. Surgical treatment of
humeral shaft fractures: the Basel experience. J Trauma
1993;35:226-232.
- Treatment of nonunion of humeral shaft fracture with dynamic
compression plate and cancellous bone graft. J Chin Med Assoc
2005; 68:73-76.
|