|
Abstract:
The
incidence of primary non-hodgkin’s lymphoma or simply known as
primary bone lymphoma (PBL) is so rare that many of its aspects
remain unknown. Till date only a few reports are available
especially from
Asia
.
Primary lymphoma of bone is uncommon, and because of
its unusual presentation patterns in bone, it can be difficult
to diagnose. According to literature, even though it can occur
at any age,
the
peak incidence is in the fifth decade of life and it is more
common in males. But we report a twenty one year old young
female, who was diagnosed to have primary B-cell bone lymphoma
of the lower end of left femur.
J.Orthopaedics 2008;5(1)e22
Introduction:
Primary bone lymphoma is a rare disease, first described by
Oberling in 1928.[1]. But it was first acknowledged as a
clinico-pathologic entity in 1939 when Parker and Jackson [2]
reported the results of 17 cases of primary reticulum cell
carcinoma of bone.
Primary lymphoma of bone, constitutes approximately 2% of
all bone tumors and 5% of all extra-nodal lymphomas.[3,4].
Primary lymphoma of bone occurs predominantly in males, a male
to female ratio of 1.8:1. [5]. It may occur at any age and the
reported average age of onset varies considerably in the
literature
[5] Peak incidence is in the fifth decade, with a median age of
44. The male to female ratio is 1.8:1. The femur is the
most commonly involved site(29%), followed by the pelvis(19%),
humerus(13%), head/neck(11%), and tibia(10%). Usually patients
present with localized pain, with approximately 50% having a
palpable mass at initial evaluation. [2,6,7, 8,9,10,11,12,13].
Primary lymphoma of bone has been described as a malignant
lymphoid infiltrate within bone with or without cortical
invasion or soft tissue extension and without concurrent
involvement of regional lymph nodes or distant viscera.[9,14].
This entity must be differentiated from other small round
cell tumors originating in bone as well as osseous
manifestations of primary extra-skeletal lymphomas.[12]
An accurate diagnosis requires obtaining a specimen
without crush artifact, as this can alter the cellular
morphologic features and make the diagnosis more
challenging.[15,16,17,18]. Also, lymphoma and osteomyelitis can
coexist.[19,20].
Case
Report :
Twenty
one year old young female presented to our institute in 2007
with history of pain and swelling left knee for three months
duration. Initially she had gradually increasing pain aggravated
by activities like walking and running. Two weeks later she
developed swelling on the medial aspect of left knee. There was
no history of fever, chills or night sweats. There was a history
of weight loss during these three months.
On clinical examination, she had a diffuse swelling on the
medial aspect of the lower end of left femur.with mild effusion
in the left knee joint. Swelling was bony hard, tender, arising
from medial condyle of left femur. Skin was free from the
swelling. She had a decreased range of movements in the left
knee. She had no other masses or lymphadenopathy.
General and systemic examination revealed no abnormalities. Haematological examination was within normal limits. Ultrasound
examination of abdomen was normal. Mantuox test was negative.
Plain roentgenogram of lower end of left femur showed a diffuse lytic lesion just above the medial femoral condyle.(figure-1).
Magnetic resonance imaging of left femur with knee showed
abnormal signal changes with areas of left femur, predominantly
involving the medial condyle.(figure-2). 99Tc MDP whole
body bone scan showed expansile non uniform intense uptake in
lower end of left femur. Rest of the skeleton showed normal
tracer activity and kidneys were normally visualized.


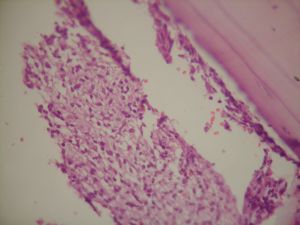
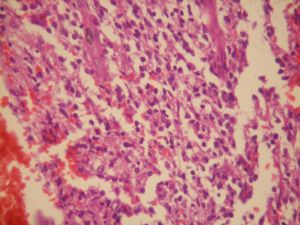
Incisional biopsy was done and the histopathological report
showed immature appearing mononuclear cells with mature
lymphocytes. (figure-3) and (figure-4).
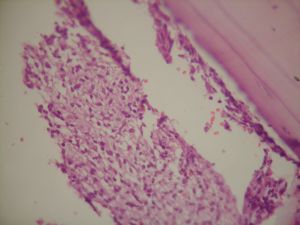
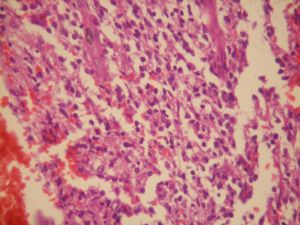
Gross
appearance of the specimen was specimen - grayish , firm
with fragments of bone and soft tissue, and small areas of
haemorrhage with the cortex being thinned out and distended.
Microscopic
appearance was Sections showing bone and soft tissue with
sheets of cells with pale cytoplasm and large nuclei- immature
appearing mononuclear cells with mature lymphocytes.The cells
possessed slightly basophilic cytoplasm with poorly defined
borders, and the nuclei were large, oval to reniform and were
poor in chromatin.
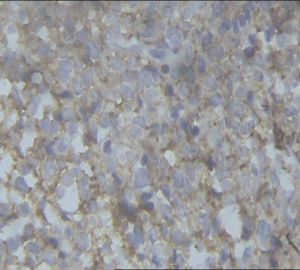
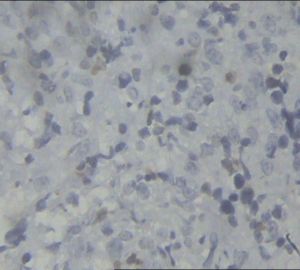
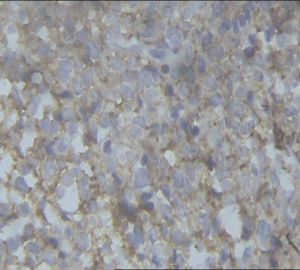
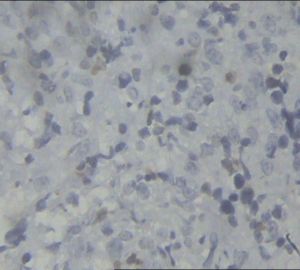
Immunohistochemistry showed CD20: diffusely positive in large
cells. CD3: negative in large cells, thus confirming the
diagnosis of diffuse large B cell lymphoma of lower end of left
femur.(figure-5) and (figure-6). There was sympathetic effusion
in the left knee joint, since the aspirated synovial fluid was
sterile on culture.The patient was treated with CHOP
regime(Cyclophosphamide,Hydroxyl
–Doxorubicin,Oncovin,Prednisolone)i.e: Cyclophosphomide- 600
mg/ m2 ,Hydroxyl-doxorubicin [Adriamycin]- 50 mg/m2 ,Oncovin
[Vincristine]- 1.4 mg/m2 and Prednisolone- 60 mg/m2 .
First
three drugs were given on day 1 and prednisolone is given
from day 1 to day 5. This is repeated every 3 weeks. Six
cycles of chemotherapy (each cycle lasting for three weeks) is
followed by radiotherapy, the dose being 400 cGy units in 20
fractions for a period of 4 weeks.
At
the time writing this report after eight months of first
detection there is no recurrence or evidence of
disease elsewhere in the body as followed up by Technitium 99
MDP Bone scan.
Discussion :
Even though it was first described by Oberling in 1928 [1],
primary bone lymphoma (PBL) was considered as a separate
clinicopathologic entity in 1939 when Parker and Jackson [2]
reported results of 17 cases of primary reticulum cell carcinoma
of bone.
Even after five to six decades of its description, the reports
of PBL are so rare that many aspects remain controversial,
particularly the definition of PBL, appropriate treatment
strategies, response criteria and prognostic factors.[ 5,21].
PBL is notorious for presenting diagnostic difficulties and
mimics other disease processes, especially infection. Tumors
diagnosed and treated as infections are not uncommon. [22] .
Blum et al reported cases of malignant lymphoma, presenting as
infection and treated as such thereby delaying the true
diagnosis and appropriate treatment.[22] . According to a study
by Marshall et al, earlier detection and treatment can effect a
better prognosis.[23] .
Primary lymphoma of bone is uncommon, comprising from 0.2 to 5%
of primary bone tumors.[15,16] . By reviewing the literature, PBL predominantly affects the males, and the femur has been
reported to be the most commonly involved location as a single
site [21] and the peak incidence is in the fifth decade [5] with
median age of forty four. The patient we reported was a
twenty one year old, young female. To the best of our knowledge,
the incidence of primary bone lymphoma in children and young
adults is very rare [5] . The site of involvement was medial
condyle of left femur, with femur being the most common site of
involvement as per the previous case reports in the literature.[
2,6,7,8,9,10,11,12,13]
According
to the WHO classification [24] , lymphoma involving bone can be
classified into four groups: Group 1, lymphoma with a single
bone site with or without regional lymph-node involvement; Group
2, lymphoma with multiple bones involved, but no visceral or
lymph-node involvement; Group 3, bone tumor with involvement of
other visceral sites or lymph nodes at multiple sites; and Group
4, lymphoma involving any other sites and found by bone biopsy
which was done to rule out possible involvement.
The WHO classification and some previous reports have
indicated that Groups 1 and 2 should be
considered as PBL, but Group 3 should be excluded from
PBL and considered to be systemic lymphoma regardless of the
bone lesion size. An appropriate definition has not been
established by verification, and hence, the subject continues to
be controversial.[21] .
Histopathologically , the previous studies reported
that majority of patients with PBL were Diffuse Large B Cell
Lymphoma (DLBCL) [14,24,25,26,27]. Immunohistochemical staining
showed CD20,CD79a, and bcl-2 positive and CD3,CD5,CD10 and CD23,
cyclin D1 and
terminal deoxynucleotidyl tranferase negative.[21] . In the
patient we reported, the histopathology revealed a diagnosis of Diffuse
Large B Cell lymphoma [DLBCL] (figure-4),(figure-5) and
immunohistochemistry revealed CD3 negative and CD20 positive.
(figure-6) and (figure-7) confirming the diagnosis of DLBCL.
Regarding treatment of primary bone lymphomas, there is
no universally accepted therapeutic approach to the management
of PBL. [28] . Even though the literature recommends combined
modality therapy with both chemotherapy and radiotherapy, a
formal treatment guideline
have not been developed. [5] . Although no formal
treatment guidelines have been established, combined modality
therapy has been shown to yield better prognosis and results
superior to those of radiation therapy alone for primary bone
lymphoma [25,29,30,31,32] . Recent studies have suggested that a
combination of chemotherapy and radiotherapy was the best
treatment for patients with primary bone lymphoma.[33,34] .
Hence, our patient was treated with six cycles ( each cycle
lasting for three weeks) of chemotherapy followed by
radiotherapy.
Conclusion:
Primary
lymphoma of bone is rare and uncommon, especially in young
individuals and in females. To the best of our knowledge, the
case we reported is a rare occurrence as per the review of
literature . This condition being rare and could mimic other
diseases especially infection, it should be included in the
differential diagnosis, so that the pathologist will be prepared
in handling biopsied specimen appropriately. If not considered
in the differential diagnosis, the possibility is not raised and
the patient may end up with a wrong diagnosis and inadequate
treatment.
Reference :
-
Oberling
C. Les Reticulosarcomes et les reticuloendotheliosarcomes de la
moelle osseuse (sarcomas d’Ewing). Bull
Assoc Fr Etude Cancer 1928;17:259–96 (in French).
-
Parker
F, Jackson H. primary reticulum cell sarcoma of bone. Surg
Gynecol Obstet 1939;68:45-53.
-
Freeman C, Berg JW, Cutler SJ: Occurrence and prognosis of
extranodal lymphomas. Cancer
29:252– 260, 1972.
-
Rudders RA, Ross ME, DeLellis RA: Primary extranodal lymphoma:
Response to treatment and factors influencing prognosis. Cancer
42:406–416, 1978.
-
Valerae O. Lewis, MD, Gregory Primus, MD, Oncologic
Outcomes of Primary Lymphoma of Bone in Adults. Clinical
Orthopaedics And Related Research 415, Pp. 90 – 97.
-
Mendenhall
NP,Jones JJ, Kramer BS, et al. the management of primary
lymphoma of bone. Radiother
Oncol 1987;9:137-45.
-
Parvinen LM, Jereb B, Nisce L. Primary non-hodgkin’s lymphoma(
reticulum cell sarcoma) of bone in adults. ACT
A Radiol Oncol 1983;22:449-54.
-
Bacci
G, Jaffe N, Emiliani E, et al. Therapy for primary
no-hodgkin’s lymphoma of bone and a comparison of results with
Ewing’s sarcoma. Cancer
1986;57:1468-72.
-
Boston
HC,
Dahlin
DC
, Ivins JC, Cupps RE. Malignant lymphoma ( so called reticulum
cell sarcoma) of bone.
Cancer 1974;34:1131-7.
-
Dosoretz
DE, Raymond AK, Murphy GF, et al. Primary lymphoma of bone.
Cancer 1982;50:1009-14.
-
Reimer
RR, Chabner BA, Young RC, et al. lymphoma presenting in bone.
Ann intern Med 1977;87(1):50-5.
-
Shoji
H, Miller TR. Primary reticulum cell sarcoma of bone. Cancer
1971;28:1234-44.
-
Wang
CC, Fleischli DJ. Primary reticulum cell sarcoma of bone. Cancer
1968;22:994-8.
-
Pettit CK, Zukerberg LR, Gray MH, et al: Primary lymphoma of
bone. Am
J Surg Pathol 14:329–334, 1990.
-
Lewis SJ, Bell RS, Fernandes BJ, et al: Malignant
lymphoma of bone.
Can J Surg 37:43–49, 1994.
-
Mirra JM: Bone Tumors: Clinical, Radiologic, and Pathologic
Correlation.
Philadelphia
, Lea and Febiger 1989.
-
Ostrowski ML, Unni KK, Banks PM, et al: Malignant lymphoma of
bone. Cancer
58:2646–2655, 1986.
-
Postovsky S, Bialik V, Keidar Z, et al: Large cell lymphoma of
bone presented by limp. J
Pediatr Orthop B 10:81–84, 2001.
-
Eismont FJ, Green BA, Brown MD, et al: Coexistent infection and
tumor of the spine: A report of three cases. J
Bone Joint Surg 69A:452–457, 1987.
-
McGrory JE, Pritchard DJ, Unni KK, et al: Malignant lesions
arising in chronic osteomyelitis. Clin
Orthop 362:181–189, 1999.
-
Dai Maruyama, Takashi Watanabe. Primary Bone Lymphoma: A New and
Detailed Characterization of 28 Patients in a Single-Institution
Study Jpn
J Clin Oncol 2007;37(3)216–223.
-
Y. C. Blum, MD, J. L. Esterhai, MD. Case Report: Lymphoma
Masquerading as Infection .Clinical
Orthopaedics And Related Research , 432, pp. 267–271.
-
Marshall DT, Amdur RJ,
Scarborough
MT
, et al: Stage 1E primary nonHodgkin’s lymphoma of bone. Clin
Orthop 405:216–222, 2002.
-
Fletcher C, Unni K, Mertens F. Pathology and Genetics of Tumours
of Soft Tissue and Bone: World Health Organization
Classification of Tumours.
Lyon
,
France
: International
Agency for Research on Cancer; 2002; 306–8.
-
Heyning FH, Hogendoorn PC, Kramer MH, Hermans J, Kluin-Nelemans
JC, Noordijk EM, et al. Primary non-Hodgkin’s lymphoma
of bone: a clinicopathological investigation of 60 cases. Leukemia
1999;13:2094–8.
-
Leval L, Braaten KM, Ancukiewicz M, Kiggundu E, Delaney T,
Mankin HJ, et al. Diffuse large B-cell lymphoma of bone. An
analysis of differentiation-associated antigens with clinical
correlation. Am
J Surg Pathol 2003;27:1269–77.
-
Radaszkiewcz T, Hansmann ML. primary high grade malignant
lymphomas of bone. Virch
Arch[A] 1988;413:269-74.
-
M.Salter, M.D.,R. J.Sollaccio,M.D. primary lymphoma of bone: the
use of MRi in pretreatment evaluation.
Am J Clin Oncol(CCT)12(2):101-105. 1989.
-
Baar
J, Burkes R, Gospodarowicz M: Primary non- Hodgkin’s lymphoma
of bone.
Semin Oncol 26: 270–275, 1999.
-
Dubey P, Ha CS, Besa PC, et al: Localized primary
malignant lymphoma of bone. Int
J Radiat Oncol Biol Phys 37:1087–1093, 1997.
-
Fidias P, Spiro I, Sobczak ML, et al: Long-term results of
combined modality therapy in primary bone lymphomas. Int
J Radiat Oncol Biol Phys 45: 1213–1218, 1999
-
Loeffler JS,
Tarbell
NJ
, Kozakewich H, et al: Primary lymphoma of bone in children:
Analysis of treatment results with adriamycin, prednisone,
Oncovin (
APO
), and local radiation therapy.
J Clin Oncol 4:496–501, 1986.
-
Barbieri E, Cammelli S, Mauro F, Perini F, Cazzola A, Neri S, et
al. Primary non-Hodgkin’s lymphoma of the bone: treatment and
analysis of prognostic factors for stage I and stage II. Int
J Radiat Oncol Biol Phys 2004;59:760–4.
-
Beal K, Allen L, Yahalom J. Primary bone lymphoma:
treatment results and prognostic factors with long-term
follow-up of 82 patients. Cancer
2006;106:2652–6.
|