|
Abstract:
Objective: A
prospective comparative evaluation of the commonly accepted
radiologic techniques including supine lateral
bending(SB),suspension traction(Tr), and fulcrum bending
radiographs(fulcrum) to determine curve flexibility and predict
surgical correction in adolescent idiopathic scoliosis (AIS).
Methods:A
total of 68 consecutive patients with AIS according to inclusion
and exclusion criteria who had surgical treatment were studied.
Preoperative X-ray evaluation consisted of standing
anteroposterior (AP) and lateral, Tr, SB, fulcrum radiographs.
All curve types were single-curve and the PUMC classification
were
I a/
I b/
I c. These patients were divided
into 4 groups according to the location and magnitude of the
curves: moderate thoracic curve (19
cases, 400<COBB≤60°),severe thoracic
curve (13
cases, COBB>60°), moderate
lumbar curve (28 cases, 35°<COBB≤60°) and severe
lumbar curve (8 cases, COBB>60°). The COBB angles were measured and the
flexibility ratio was determined on each radiograph. The amount
of correction obtained by all radiographic methods was compared
with the amount of surgical correction by evaluating the
differences from surgery as absolute values. Statistical
differences were calculated with the comparison of the exact 95%
confidence intervals for the mean.
Results:For
the moderate thoracic curves, fulcrum provided the best amount
of flexibility with significant difference from SB and
Tr and no significant difference between %flexibility determined
on fulcrum and surgical %correction was found. There were
significant differences between %flexibility determined on each
radiographs and surgical %correction in the remaining three
groups. For the severe thoracic curves, fulcrum provided clearly
better flexibility compared to Tr and SB, however
with no significant difference between Tr and SB. For the
moderate and severe lumbar curves, %flexibility obtained by
fulcrum and SB were significantly different from Tr, but with no
significant difference between fulcrum and SB.
Conclusions:Fulcrum
can better assess flexibility and correction of thoracic curves
in AIS but only predict those in moderate thoracic curves.
Fulcrum and SB are similar with analyzing flexibility in lumbar
curves.
J.Orthopaedics 2008;5(1)e2
Keywords:
Idiopathic
scoliosis; Flexibility; Radiography
Introduction:
Optimal balance over pelvis and the least
number of fused segments have always been the major goal of
surgical treatment for adolescent idiopathic scoliosis (AIS)
1-2. To achieve this goal, analysis and differentiation of
various curve types and their response to corrective forces have
been a source of concern to spine surgeons. Thus, preoperative
evaluation of curve flexibility has become a crucial component
of curve analysis, fusion level selection, correction
prediction, and surgical decision making. There are three
commonly used X-ray techniques including suspension traction
radiograph (Tr)3,
supine lateral bending radiograph (SB)3
and fulcrum bending radiograph (fulcrum)4 to determine curve
flexibility and predict surgical correction in AIS. However,
fewer prospective study results were reported. What’s more,
the improved design of new generation implants and capacity to
obtain more and more correction led spine surgeons to suspect
the value of these accepted methods for assessing curve
flexibility.
The
purpose of this prospective study was to explore the value of
three commonly accepted X-ray methods in flexibility evaluation
and surgical correction prediction of AIS.
Material and Methods :
Patients
General data:From October 2003 to August
2006, 68 adolescent idiopathic scoliosis (AIS) patients according to the
inclusion and exclusion criteria were enrolled in this
prospective clinical study at the Spine Center of Peking Union
Medical College Hospital in
Beijing
,
China
. The inclusion criteria were designed as: a.) Diagnosed
as AIS
with aged from 11-18 years old; b.)
Curve types were single-curve and the PUMC5 classification were
I a/
I b/
I c; c.)
Patients were divided into 4 groups according to the location
and magnitude of
COBB angles oon standing
anteroposterior (AP) films: moderate thoracic curve(40°<COBB≤60°), severe thoracic curve(COBB>60°), moderate
lumbar curve(35°<COBB≤60°), and severe lumbar curve(COBB>60°); d.)
The third-generation spinal segmental instrumentation systems were used during surgery; e.) All patients in thoracic
curve group and severe lumbar curve group underwent posterior
spinal fusion (PSF) with segmental pedicle screws as the sole
anchor, and patients in moderate lumbar curve group underwent
anterior short-segmental anterior
spinal fusion (ASF) with single solid rod and single vertebral
screw constructs; f.) The criteria to determine the levels
to be included in the arthrodesis in each group was identical
according to PUMC classification5. The exclusion
criteria were designed as: a.) Age
younger than 10 years old;b.) Risser sign 0°; c.) A positive
history of spinal surgery; d.)Patients suffered from surgery
related complications or postoperative radiologic decompensation; e). Patients with moderate
lumbar curve underwent PSF; f.)
Lumbar/thoracolumbar kyphosis; g.) Patients with dissatisfied preoperative radiological
data.
All patients were divided into the following 4 groups.
1.
Moderate thoracic curve group(40°<COBB≤60°): All
19 cases were females with the mean age of 14.6 years old
(ranged from 11 to 17).The mean preoperative COBB angle on
standing AP film was 44.79±4.65° (ranged from 40 to 50°).
All curves were single-thoracic-curve (diagnosed as PUMC
I
a type) and underwent a PSF with segmental pedicle screws
as the sole anchor. The distal instrumented level in all cases
was 1 level proximal to stable vertebrae. The implants included
5 Mossmiami, 2 Isola,
3 CDH, 8 TSRH and 1 SSE.
2. Severe thoracic
curve group(COBB>60°):There
were 9 females and 4 males in this group with the mean age of 14.7 years old (ranged
from 13 to 18). All curve types were PUMC
I
a. The mean preoperative COBB angle on
standing AP film was 87.62±16.58° (ranged from 65 to 110°).
The implants included 1 Mossmiami, 8 Isola, and 4 TSRH. The surgical technique and fusion
level selection principle were similar to moderate thoracic curve group.
3. Moderate lumbar curve group (35°<COBB≤60°):There were 18 cases of PUMC
I
b type (4 males and 14 females) and 10 cases of PUMC
I
c type (1 male and 9 females) in this group with the
mean age of 15.5 years old (ranged from 12 to 18). All curve
types were single-lumbar/thoracolumbar-cuvre.
The mean preoperative COBB angle on standing AP film was 43.29±7.32° (range from 35to 58°).
Short-segmental anterior fusion level selection principle
recommended by PUMC classification system5 was in
reference to Hall's criteria5: a.)
If the apex is a vertebra on the standing AP film, instrument
one vertebral body above and below; if
the apex is a disc, instrument 2 vertebral bodies above and
below. b.) On convex bending film, the first disc space above
and below the apex that opens up can be left unfused; on
concave bending film, vertebral bodies below the apex should be
parallel to the sacrum. If there is a discrepancy among the
levels indicated in the aforementioned methods, the longest
segment of instrumentation should always be selected. The
implants included 4 Isola and 24 CDH.
4. Severe
lumbar curve group(COBB>60°):There were 3 males and 5 females in this group with
the mean age of 16.4 years old (ranged from 14 to 18). All curve
types were PUMC
I
b. The mean preoperative COBB
angle on standing anteroposterior film was 69.50±9.80° (ranged from 61 to 88°).
The surgical technique and fusion level selection principle were
similar to thoracic curve
group. The implants included 1
CDH, 2 Mossmiami, 2 Isola, and
3 TSRH.
Methods
All patients were
eventually diagnosed as adolescent
idiopathic scoliosis (AIS) through preoperative detailed case
history collection, thorough physical and auxiliary examination.
All patients received X-ray, myelography or simultaneous
CTM, and MRI et al. The preoperative X-ray examination included standing AP and lateral
radiographs, suspension traction radiographs (Tr), supine
lateral bending radiographs (SB), fulcrum bending radiograph (fulcrum). Curves were identified as
thoracic or lumbar/thoracolumbar, depending on the location of the apex of the deformity. All patients were
single-curve. All structural curves were measured using the Cobb
method, and flexibility ratio was determined on each radiograph
(Tr/SB/fulcrum).
%Flexibility on each radiograph= (preoperative COBB angle on
standing AP film - preoperative COBB angle on Tr/SB/fulcrum film)/preoperative COBB angle
on standing AP film. These radiographs were compared with the
postoperative radiograph, which was made with the patient
standing AP approximately 1 weeks postoperatively. The
experienced surgeon (Qi Fei) measured the radiographs. The flexibility% determined on
each radiograph was compared with the amount of surgical
correction% by evaluating the differences from surgery as
absolute values. Percentage
surgical correction
was calculated using the formula: %Correction = (preoperative
COBB angle on standing AP film - postoperative COBB angle on
standing AP film)/preoperative COBB angle on standing AP film.
All patients in each study group were operated on by the same
surgical team (Gui-xing Qiu and Yi-peng
WANG), undergoing
the same surgical procedures. The specific radiologic methods
about Tr/SB/fulcrum were in reference to pertinent
literature3-4.
Statistical
methods
Patients’
preoperative and postoperative COBB angle on different X-ray
methods, the flexibility% on each radiographic methods (Tr/SB/fulcrum)
and surgical correction%,
and respective COBB angle on three X-ray methods (Tr/SB/fulcrum)were
compared and analyzed using SPSS 13.0 (SPSS, Inc.,
Chicago
,
IL
). A P value less than 0.05 would be considered
statistically significant.
COBB
angles after operation (Table 1).
In
moderate
thoracic curve group, the mean postoperative COBB angle on standing AP film was 9.11±5.83°,
a statistical t test demonstrated no significant
difference (p=0.076) compared to preoperative COBB angle on fulcrum
film, but significant difference (p<0.01) compared
to preoperative Tr/SB and standing AP film. In severe thoracic curve group,
the mean postoperative COBB angle was 39.92±22.09° and
there were significant differences (p<0.01) when compared to all preoperative
films. In moderate
lumbar curve group, the mean postoperative COBB angle was 6.18±4.52° and there were significant difference
(p<0.01) when compared to preoperative Tr/fulcrum and
standing AP film, also difference (p=0.013) compared to SB film. In severe lumbar curve group,
the mean postoperative COBB angle was 24.0±5.33° and a
statistical t test showed significant difference (p<0.01) when compared to preoperative Tr and
standing AP film, also difference compared to fulcrum (p=0.021) or SB film(p=0.011
).
Table
1. Preoperative
and postoperative COBB angle (x±s°)
in 4 groups
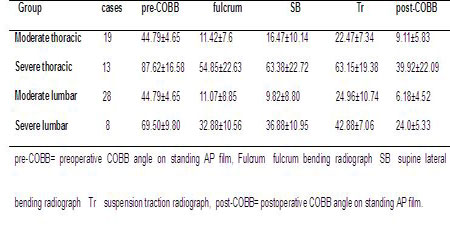
Table 2
.%Flexibility
determined on Tr/SB/fulcrum
film and surgical %correction
In moderate thoracic curve group,
a statistical t test demonstrated no significant
difference (p=0.111) between %flexibility on fulcrum (75%) and surgical
%correction(80%), however significant difference (p=0.000) between %flexibility
on Tr and %correction, and difference (p=0.011) between %flexibility
on SB and %correction. The amount of
%flexibility on fulcrum was larger than that on SB and Tr (p<0.01),
%Flexibility on SB was larger than that on Tr (p<0.01).
In severe thoracic
curve group, there were significant differences (p<0.01) between %flexibility
on Tr/SB/fulcrum and %correction (57%), but no significant difference of
%flexibility (p=0.999) between SB and Tr.
The amount of %flexibility on fulcrum was larger than that on SB (p=0.027) and Tr (p=0.003). In moderate lumbar curve group, a
statistical t test demonstrated significant difference
between %flexibility on Tr (44%,
p<0.01)/fulcrum (76%,
p<0.01)/SB (79%,
p=0.019) and surgical %correction (86%).
The amount of %flexibility on fulcrum and SB were larger than
that on Tr (p<0.01), but no significant difference between fulcrum and SB (p=0.105). In severe lumbar curve group, there were significant
difference between %flexibility on Tr (38%, p<0.01)/SB (47%,
p<0.01)/fulcrum (53%,
p=0.017) and %correction (67%). However,
The amount of %flexibility on fulcrum was similar to that
on SB (p=0.086), and %flexibility on SB was also similar to Tr (p=0.101).
|
Group
cases
Flexibility(%)
Correction(%)
|
|
Moderate
thoracic
19
fulcrum(75%)>SB(63%)>Tr(50%)
80%
Severe thoracic
13
fulcrum(39%)>Tr(29.13%)>SB(29.12%)
57%
Moderate
lumbar
28
SB(79%)>fulcrum(76%)>Tr(44%)
86%
Severe
lumbar
8
fulcrum(53%)>SB(47%)>Tr(38%)
67%
|
|
Fulcrum=fulcrum bending
radiograph,
SB=supine lateral
bending radiograph,
Tr=suspension
traction radiograph.
Table
3. Comparison of preoperative COBB angle on different
X-ray(x±s°)
|
Group
cases
X-ray
COBB angle,95%CI
p value
|
|
Moderate thoracic
19
fulcrum
11.42±7.6, 7.76-15.09
fulcrum-SB
0.012×
(40°<COBB≤60°)
SB
16.47±10.14,
11.59-21.36
fulcrum-Tr
0.000×
Tr
22.47±7.34,
18.94-26.01
SB-Tr
0.035×
Severe
thoracic
13
fulcrum
54.85±22.63, 41.17-68.25
fulcrum-SB
0.011×
(COBB>60°)
SB
63.38±22.72,
49.65-77.12
fulcrum-Tr
0.004×
Tr
63.15±19.38, 51.44-74.87
SB-Tr
0.945
Moderate lumbar
28
fulcrum
11.07±8.85, 7.64-14.5
fulcrum-SB
0.083
(35°<COBB≤60°)
SB
9.82±8.80,
6.41-13.23
fulcrum-Tr 0.000×
Tr
24.96±10.74,
20.8-29.13
SB-Tr
0.000×
Severe lumbar
8
fulcrum
32.88±10.56, 24.05-41.70
fulcrum-SB
0.091
(COBB>60°)
SB
36.88±10.95,
27.72-46.03
fulcrum-Tr
0.002×
Tr
42.88±7.06,
36.97-48.78
SB-Tr
0.115
|
|
Fulcrum=fulcrum bending
radiograph,SB=supine
lateral bending radiograph,Tr=suspension traction radiograph, CI=confidence interval.
|
Discussion:
Preoperative
assessment of spine flexibility in adolescent idiopathic
scoliosis (AIS) is important to determine the levels to be
included in the arthrodesis and the expected postoperative
correction. There are many clinic accepted X-ray methods such as traction radiograph (Tr), supine side-bending radiograph (SB), fulcrum bending radiograph (fulcrum), push-prone radiograph6 (pushing), standing
side-bending radiograph7, and supine traction radiographs under
general anesthesia8 to be used for assessing flexibility and
predicting surgical correction of AIS.
As
the King classification theory for AIS was known and
accepted, supine side-bending radiographs (SB) had been widely used to help in the
preoperative evaluation, especially for selection of the
fusion area. However, the development of current segmental
spinal instrumentation systems, especially segmental
pedicle screw constructs, have achieved more correction
than would be expected from evaluation of traditional
side-bending radiographs made with the patient supine9.So supine side-bending radiographs (SB) may
fail to predict surgical correction. Although less
frequently used than side-bending radiographs (SB), traction radiographs are also being
used by some surgeons and centers for predicting the
amount of postoperative correction, especially in patients
who are less able to perform the side-bending radiographs
(i.e., in patients with neuromuscular scoliosis or
mental retardation). Winter and Lonstein10 reported
that a traction view is more accurate for determining
flexibility in curves more than 60°. However, whether
traction shows higher flexibility in AIS curves is unknown
or debatable.
Cheung
and Luk4 first described “the fulcrum bending radiograph”
for the assessment of spinal flexibility and compared the
predictive value of the fulcrum bending radiograph with
that of the supine lateral bending radiograph. They
concluded that the fulcrum bending radiograph was always
more predictive of the final correction. But few
prospective comparative studies about fulcrum bending
radiograph for assessing flexibility of AIS were reported.
Push-prone radiograph8 (pushing)were
also used by some scholars to assess flexibility of AIS. But the disadvantages included
the difficulty in standardizing the force exerted on the
apex of the curve and the physician’s excess exposure to
radiation. The reproducibility of pushing
is also not known. Recently Hamzaoglu A8 reported traction radiographs with the
patient under general anesthesia may show much better
flexibility, especially in more than 65° and rigid AIS
curves. But in their study, the number of rigid and severe
AIS cases were very small, and the surgeon were not be
able to give the patient a definitive plan before surgery
because the decision can only be finalized after seeing
the traction radiographs with the patient under general
anesthesia. What’s
more, they used manual traction with maximum effort, which
should be replaced by a more standard technique or method
of traction to standardize the amount of force applied.
Now traction radiograph (Tr),
supine
side-bending radiograph(SB),and fulcrum bending radiograph(fulcrum)were best commonly used to assess the
flexibility of AIS. However, these methods have been
evaluated in relation to correction obtained with the
Harrington distraction system and not with the newer,
especially more rigid segmental pedical screws spinal
instrumentation systems. To compare the value of the three
X-ray methods and search an optimal method to analyze
thoracic or lumbar curve flexibility and the curve
response to surgical correction, we have started this
prospective comparative study from 2003. We also want to
know whether the three X-ray methods can predict surgical
correction after the use of new segmental spinal
instrumentation system especially including total pedicle
screw instrumentation.
In our study, all AIS patients were single-curve and
divided into moderate and severe thoracic/lumbar curve
group according to PUMC classification system5 and the magnitude of COBB angle on
preoperative AP films at the first time. Our goals were to
standardize study object, discuss the value of Tr/SB/fulcrum radiographs for assessing
thoracic or lumbar curve respectively, and avoid the
interaction of double curves(PUMC
II type) or three curves(PUMC
III type) during preoperative X-ray
examination.
Our
practice in this study showed curve %flexibility and
postoperative COBB angle were best assessed by
fulcrum radiograph in moderate or severe thoracic curve
group (Table 1-3). Especially in moderate thoracic curve
group, there was no significant difference of the COBB
angle between fulcrum
radiographs and postoperative AP films (p=0.076), and also no significant
difference between %flexibility determined on fulcrum
radiographs and surgical %correction (p=0.111).
These results indicated that the fulcrum radiograph for assessing flexibility of
thoracic curve in AIS was superior to Tr/SB radiographs,
and it even could predict surgical correction of
moderate thoracic curve in AIS after undergoing a PSF with segmental pedicle screws as the sole anchor. Some reasons
were considered to contributing to these results: a.) We
found it was easy to center the fulcrum under the rib
corresponding to the apex of the thoracic curve through
identifying the position of “razor back deformity”; b.) It was easy to check that the
shoulder is lifted off the X-ray table;
c.) The fulcrum radiograph was easy to make and the
bending force was passive and reproducible; d.)
The amount of passive corrective force through the
conduction of ribs was so powerful that it seemed to
correspond well with the degree of correction that was
obtained in thoracic curve with good flexibility(moderate
thoracic curve) of AIS underwent a PSF with segmental pedicle screws as the
sole anchor.
However, in moderate/severe lumbar curve group, no
significant differences of the %flexibility and COBB angle
measured between fulcrum
and SB radiographs were found (Table
2-3, p>0.05).
We considered the following reasons may result to the poor
results of fulcrum radiograph for assessing
flexibility and predicting %correction in lumbar curve
group: a.) There are wide individual difference of fat and muscles distribution
among children,and
the “razor back deformity” in lumbar curves was often
not easy to be identified especially in moderate lumbar
curves, so
it was not easy to find the apex of the lumbar curve; b.)
It was not easy to center the fulcrum under the apex of
the lumbar curve because of the short size of lumbar
vertebrae in children; c.)
The passive corrective force was relatively poor because
of lacking of the conduction of ribs.
The
role of Tr radiograph for predicting flexibility and
surgical correction demonstrated in this study was
inferior to fulcrum/SB radiographs except no significant
difference between Tr and SB (p=0.999,
Table 2) in severe thoracic curve group. The suspension traction
radiograph could not predict surgical %correction in all
groups (p<0.01). The traction radiograph made with the
patient suspending required active cooperation and effort
by the patient, and the traction time had wide individual
difference. Additionally, it also did not remove the
muscle factor that affects clinical curve flexibility.
These factors may result in the poor value of traction radiograph for analyzing curve
flexibility and, at the same time, the curve response to
surgical correction in AIS.
Moderate thoracolumbar/lumbar AIS
was traditionally considered to be best indicated for
instrumented anterior spinal fusion (ASF). ASF offered the
benefit of improved curve correction and derotation while
preserving more distal motion segments compared to the
posterior approach. Our practice in this study
demonstrated that the mean surgical %correction in
moderate lumbar curve group was up to 86%, superior to
%flexibility measured on Tr/SB/fulcrum radiographs (Table
2). The results showed all three traditional X-ray methods
did not predict surgical correction of moderate lumbar AIS
undergoing ASF.
Current
segmental spinal instrumentation systems, especially
segmental pedicle screw constructs, have been widely used
and achieved more correction than the Harrington
distraction system and previous third-degeneration spinal
hook instrumentation systems11 12 13, especially in severe curves. In
severe thoracic/lumbar curve group of this study, surgical
%correction was 57% and 67% respectively, with significant
difference from %flexibility measured on Tr/SB/fulcrum
radiographs (Table 2, p<0.01). It indicates that better
analysis of curve flexibility and consistent predictions
of correction result require the development of new
radiologic methods or techniques.
All
above from this prospective study suggest that the fulcrum
bending radiograph (Fulcrum) can better analyze curve
flexibility and correction of thoracic curves in AIS
compared to Tr/SB radiographs, but only predict surgical
%correction in moderate thoracic curves. Fulcrum and SB
are similar with predicting flexibility in lumbar curves.
The new techniques are expected to emerge for adapting the development of new spinal instrumentation.
References:
-
Kirk KL, Kuklo TR, Polly DW Jr. Traction versus side-bending
radiographs: is the proximal thoracic curve the stiffer
curve in double thoracic curves? Am J Orthop 2003;32: 284–288.
-
Lenke
LG,
Betz
RR,
Harms
J,
Bridwell
KH,
Clements
DH,
Lowe
TG, et al. Adolescent idiopathic scoliosis: a
new classification to determine extent of spinal
arthrodesis. J Bone Joint Surg(Am) 2001;83:1169-1181.
-
Yu Zhao,Gui-Xing
Qiu, Jian-Xiong Shen. Evaluatian of imaging methods for
predicting the correction of scoliosis. Clinical Journal
of Rehabilitation 2004;26,5692-5694(In Chinese).
-
Luk KD,Lu
DS,Cheung KM,
Wong
YW. A prospective
comparison of the coronal deformity correction in thoracic
scoliosis using four different instrumentations and the
fulcrum-bending radiograph. Spine 2004;29:560-563.
-
Qiu
G,
Zhang
J,
Wang
Y,
Xu
H,
Zhang
J,
Weng
X, et al. A new operative classification of idiopathic scoliosis:a
Peking
Union
Medical
College
method. Spine 2005;30:1419-1426.
-
Vedantam
R,
Lenke
LG,
Bridwell
KH,
Linville
DL. Comparison of pushprone and lateral-bending
radiographs for predicting postoperative coronal aligmnent
in thoracolumbar and lumbar scoliotic curvel. Spine 2000;25:76-81.
-
Klepps SJ, Lenke LG, Bridwell KH, Bassett GS, Whorton
J. Prospective
comparison of flexibility radiographs in adolescent
idiopathic scoliosis. Spine 2001;26:E74-79.
-
Hamzaoglu A, Talu U, Tezer M, Mirzanli C, Domanic U,
Goksan SB. Assessment of curve flexibility in adolescent
idiopathic scoliosis. Spine 2005;30:1637-1642.
-
Suk SI,
Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in
the treatment of thoracic idiopathic scoliosis. Spine 1995;20:1399–1405.
-
Winter RB, Lonstein JE.
Idiopathic scoliosis. In: Rothman RH,
Simeone FA,eds. The Spine.
3rd ed.
Philadelphia
,
PA
: Saunders;1992:411.
-
Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a
new technique of three-dimensional deformity correction
with segmental pedicle screw fixation in adolescent
idiopathic scoliosis. Spine 2004;29:560–563.
-
Suk
SI,
Lee
SM,
Chung
ER,
Kim
JH,
Kim
SS. Selective thoracic fusion with segmental
pedicle screw fixation in the treatment of thoracic
idiopathic scoliosis: more than 5-year follow-up.
Spine 2005;30:1602–1609.
-
Storer
SK, Vitale MG, Hyman JE, Lee FY, Choe JC, Roye DP Jr.
Correction of adolescent idiopathic scoliosis using
thoracic pedicle screw fixation versus hook constructs. J
Ped Orthop 2005;25:415–419.
|
|


