|
Abstract:
Odontoid
fractures are the most common cervical spine fractures for
patients aged >70 years and are the most common of all spinal
fractures for patients aged >80 years. Type II fracture is
the most common type of odontoid fracture and considered
relatively unstable. It occurs at the base
of the odontoid, between the level of the transverse ligament
and the C2 vertebral body. In
geriatric population, is important to look for any associated
clinical comorbidities that may affect management.
Treatment options for displaced odontoid fractures
can be conservative or surgical. Conservative management
includes immobilization in a cervical collar or halo vest.
External immobilization with a cervical collar has led to
inconsistent results. Halo vest immobilization in elderly is
associated with a significant nonunion rate and several
complications. Well agreed upon surgical indications are the
poly-trauma patient, the presence of a neurologic deficit, an
associated unstable subaxial spine injuries that requires
surgical fixation and a symptomatic nonunion. Surgical
management includes either anterior odontoid screw fixation or
posterior C1-2 instrumentation and fusion.
J.Orthopaedics 2008;5(1)e17
Epidemiology:
Odontoid fractures represent 9% to 15% of adult cervical
spine fractures.13
They commonly occur as a result of low-energy impacts such as
falls in the elderly.4,
5 Odontoid fractures are the most common cervical spine
fractures for patients aged >70 years and are the most common
of all spinal fractures for patients aged >80 years.6
There are equal male-to-female distributions in both
populations. The frequency of associated neurologic injury is
variable among multiple studies, ranging from 2% to 27%.7,
8, 9 However, when present, it is usually catastrophic
because of the high level of spinal cord injury. Odontoid
fracture combined with subaxial cervical spine injury is
uncommon and rarely reported in the literature. Misdiagnosis or
inappropriate management of such combined injuries may result in
further neurologic deficit or late spinal instability. The
mechanism of odontoid fracture can be either hyperextension that
often results into posterior displacement of the odontoid or
hyperflexion that often results in anterior displacement.
It is difficult to explain the reasons for the increased
incidence of odontoid fractures in elderly compared to younger
age groups. This may reflect the propensity for accidental
falling in the elderly and its associated mechanism of trauma.
Lakshmanan et al,10 suggested an explanation for such
increased incidence based on their study of CT-scan images of
the cervical spine in 23 patients who were over the age of 70
years and had odontoid fractures. In each patient, the type of
odontoid fracture and the characteristics of the degenerative
changes in each joint were analysed. Twenty-one of 23 patients
had Type-II odontoid fractures. The incidence of significant
atlanto-odontoid degeneration in these individuals was very high
(90.48%), with relative sparing of the lateral atlantoaxial
joints. Osteoporosis was found in 13 of 23 patients at the
dens-body junction and in seven of 23 patients involving the
odontoid body. With ageing, progressively more advanced
degenerative changes develop in the atlanto-odontoid joint.
These eventually may, in some people, obliterate the joint space
and fix the odontoid to the anterior arch of the atlas. In
contrast, the lateral atlantoaxial joints are hardly affected by
osteoarthritis. Thus, atlantoaxial movements including
atlantoaxial rotation are markedly limited by osteoarthritis of
the atlanto-odontoid joint. However, there is still potential
for movement in the lateral atlantoaxial joints, as they remain
relatively free of degenerative change. The vulnerability of the
atlantoaxial segment is further increased by markedly limited
rotation below the axis vertebra due to advanced facet-joint
degeneration. As a consequence, a relatively low-energy trauma
to the lateral part of the face, for instance by a fall, will
induce forced atlantoaxial rotation. This, with the marked
limitation of movement at the atlanto-odontoid joint, will
produce a torque force at the base of the odontoid process
potentially leading to a Type II fracture.
Classification:
In the 1970s Anderson and DAlonzo,11
proposed the most widely used classification system for odontoid
fractures. Type I fracture is infrequent and occurs near the tip
of the odontoid process, above the transverse ligament. It
occurs by avulsion of the apical and/or alar ligaments and it
considered relatively stable. However, this fracture type also
may be associated with an unstable occipital-cervical
dislocation that can result from bilateral avulsion of the alar
ligaments or a contralateral occipital condyle fracture. Type II
fracture is the most common type of odontoid fracture and
considered relatively unstable. It occurs
at the base of the odontoid, between the level of the transverse
ligament and the C2 vertebral body. Type III fracture extends
into the vertebral body and are relatively stable.
Anderson and DAlonzo,11 suggested treatment
algorithms based on the relative stability of each fracture
type. Type I and type III fractures are usually treated
conservatively with external immobilization either in a collar
or a halo vest. However, there is ongoing debate on the best way
to manage type II fractures; options include cervical collar,
halo vest, anterior odontoid screw fixation or C1-2 posterior
instrumentation and fusion. 1,
2, 3, 11, 12, 13, 14, 15, 16
It is often difficult to differentiate between type II
and type III fractures. Grauer et al,17
have suggested a more precise definition to differentiate type
II from type III fractures. Type II fractures were defined as
fractures located caudal to the inferior border of the anterior
C1 ring, with no extension into the superior articular facets of
C2. If the fracture extends into one of the superior articular
facets of C2, the fracture was classified as a type III
fracture. To further define the personality of Type II fractures regarding
fracture line obliquity, displacement, and comminution that
clearly affect treatment recommendations, Grauer et
al,17 have also suggested a subclassification
of type II fractures.Type IIA describes
a minimally or nondisplaced fracture with no comminution. These
fractures are generally treated with external immobilization. A
Type IIB fracture is a displaced fracture extending from
anterior-superior to posterior-inferior, or a transverse
fracture. These fractures can be treated with anterior screw
fixation following fracture reduction, assuming adequate bone
density. Type IIC was defined as a fracture line extending from
anterior-inferior to posterior superior or a fracture with
significant comminution. These fractures are generally treated
with posterior C1-2 instrumentation and fusion.
Clinical
Assessment
In
geriatric population, is important to look for any associated
clinical comorbidities that may affect management. A full neurologic assessment is obtained and the entire spine should be
imaged to rule out any noncontiguous spinal injuries. There
is 34% risk of noncontiguous spine fractures associated with the
presence of an odontoid fracture,.24
Imaging Studies
In some centers a computerized tomography (CT) of the
cervical spine is currently done as the primary modality to
assess for cervical spine injury due to the inherit limitation
of the plain radiographs in evaluating the upper cervical spine
and cervicothoracic junction.18, 19, 20 Furthermore,
a recent report suggested that CT imaging should be used to
obtain rapid, efficient cervical spine evaluation and negate the
need for plain radiographic imaging.21 However, the
authors still recommend the traditional three plain x-ray
cervical spine series (anteroposterior, cross table lateral and
open mouth view) for the initial assessment of patients with a
suspected odontoid injury. .22,
23 The rational for obtaining plain radiographs is for the surgeons to get familiar
with the personality of
the fracture on plain radiographs which is the modality that
will be used intraoperatively in case of surgical management.
A
transverse fracture line may be missed on a CT
scan axial cut. Therefore, it is important to evaluate carefully
the reformatted (sagittal, coronal) CT images. Magnetic
resonance imaging (MRI) should be obtained if there is a
neurologic deficit or to evaluate for suspected ligamentous
injury.
Management:
Several important factors should be considered when
deciding on the best management plan for displaced type II
odontoid fractures in elderly patients. These factors include
decreased bone density that interferes with adequate fixation
with anterior odontoid screw, the fact that the elderly do not
tolerate halo immobilization well and most importantly
associated medical comorbidities. The
literature has shown that, when comparing fractures in persons
younger than 40 years to those older than 65 years, there was a
35% earlier mortality following treatment in the elderly
population.4,
5, 6, 25, 26
Treatment options for displaced odontoid fractures can be
conservative or surgical. Conservative management includes
immobilization in a cervical collar or halo vest. Surgical
management includes odontoid screws fixation, or C1-2 posterior
instrumentation and fusion that can be achieved with either C1-2
transarticular screws or C1 lateral mass screw and C2 pars
screws. 1,
2, 3, 11, 12, 13, 14, 15, 16
Conservative Management
through External Immobilization with Cervical Collar or Halo
Vest
External immobilization with a cervical collar has led to
inconsistent results. The associated nonunion rate is believed
to be caused by the high degree of instability of this fracture
pattern.27, 28, 29
This nonunion rate may also be related to a decreased
vascularity at the watershed region at the odontoid base, thus
producing a decreased healing potential. Consequently, some
surgeons have recommended halo vest immobilization for type II
odontoid fractures.28
However, halo vest immobilization is still associated with a
significant nonunion rate in a number of series, ranging from
26% to 80%.5, 8, 9, 27, 30 Furthermore, halo vest use
in the elderly has been associated with complications in the
range of 26%, including poor reduction maintenance, pneumonia,
pin site infection, cerebral spinal fluid leakage, and even
death.30-, 31
Some surgeons believe that a stable nonunion
achieved after external immobilization with a cervical collar in
the elderly population is an acceptable risk when considered
against the potential morbidity of surgical intervention. Often
times a semi-rigid cervical collar is the treatment of choice
(figure 1).
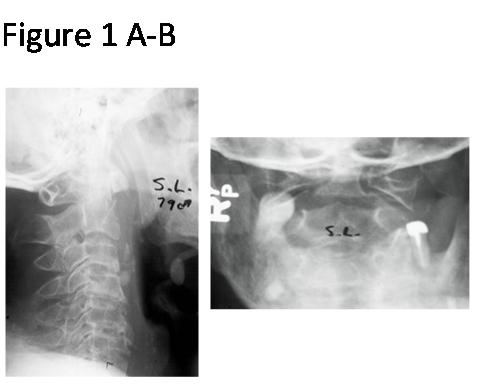
Figure 1 A-B. Lateral and open mouth views of 79
year old male showed Type II odontoid fracture which was
sustained after a fall while walking. Patient was treated in
Miami J collar for 3 months.
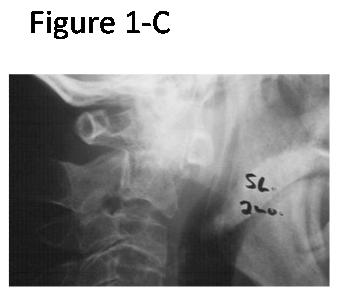
Figure 1-C Two months follow up lateral view
showed maintenance of acceptable alignment
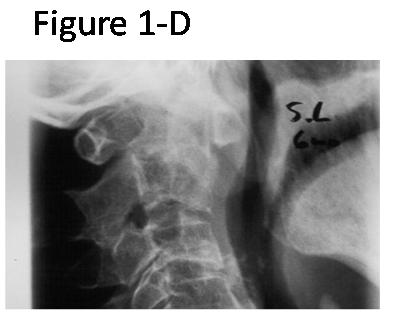
Figure 1-D Six months follow up lateral view
showed bridging callus across the fracture site.
Surgical Management
Due to the concerning high incidence of nonunion with
external immobilization, multiple studies have suggested primary
surgical management in elderly patients that include either
anterior odontoid screw fixation or posterior C1-2
instrumentation and fusion.26, 28,
Well agreed upon indications for surgical management in
displaced type II odontoid fractures include; poly-trauma
patient, neurologic deficit, and associated unstable subaxial
spine injuries that require surgical fixation. In these cases
the surgeons can use either anterior odontoid screw fixation or
posterior C1-2 instrumentation and fusion depending on
patient s body habit, presence of osteoporosis, the obliquity
of the fracture line, and the ability to achieve successful
anatomic reduction of the fracture. One has to elect posterior
C1-2 fusion rather than anterior odontoid screw in displaced
type II odontoid fractures that are associated with C1-2
instability secondary to transverse ligament injury and
symptomatic nonunion that develops after either external
immobilization or anterior odontoid screw fixation. 26,
28
Odontoid fracture combined with subaxial unstable
cervical spine injury is uncommon and rarely reported in the
literature. Closed reduction should be tried first and then both
fractures can be fixed, if possible, under the same anesthesia.
The priority in the surgical management should be given
for the fracture that causes spinal cord injury in patient with
neurologic deficit. If the patient is neurologically intact then
the priority is given for the fracture that could not be
successfully reduced with preoperative traction. If the patient
is neurologically intact and both fractures are successfully
reduced with preoperative traction, one has to consider the
extend of instability between the odontoid fracture and the
subaxial cervical spine injury and the risk of surgical
intervention involving each injury. Many would choose to
surgically stabilize both injuries while others would prioritize
stabilizing the subaxial cervical spine when the odontoid
fracture is successfully anatomically reduced with preoperative
traction.
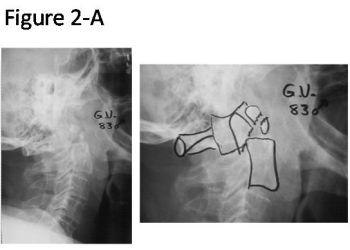
Figure 2 A Lateral
view of 83 year old male showed comminuted Type II odontoid
fracture with posterior displacement and posterior angulation
which he sustained after a motor vehicle accident.
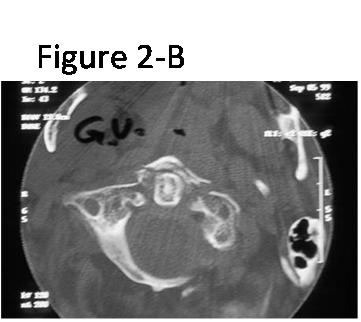
Figure 2 B Axial
CT scan showed associated C 1 anterior arch fracture

Figure 2 C
Lateral view showed C1-2 posterior fusion with transarticular
screws and sublaminar wire.
Anterior Odontoid Screw Fixation
To
avoid loss of 50% of cervical rotation with C1-C2 fusion Bohler
in 1982,32
described anterior odontoid screw fixation. Specifically
designed retractors and biplanar fluoroscopy are important for
this procedure. After adequate fracture reduction following
patient positioning on the operative table and ensuring
appropriate trajectory for screw placement with the help of
fluoroscopy, a low cervical approach is made around the
C5-C6 level. The prevertebral plane is then developed, allowing
access to the C2-C3 disk space. The entry site for the screw is
at the anterior-inferior corner of the C2 endplate and although
preservation of the C2-C3 disk space is important, most surgeons
apply the screw through the C2-C3 disk space to ensure an
adequate screw trajectory. Two screws have been initially used
with this technique. However, most surgeons are currently using
a single screw as studies have shown no significant difference
between the biomechanical stability or nonunion rates of 1 or 2
screws. Furthermore, it is often not safe to place 2 screws.33,
34
The reported fusion rates with anterior odontoid screw
have ranged from 83% to 100%.12, 33, 35, 36 However,
Anterior odontoid screw fixation is not suitable for each type
II odontoid fracture. This method is only appropriate for type
II fractures that could be adequacy reduced. Patients with
cervical or thoracic kyphosis and short, thick necks may also
not allow for appropriate trajectory for screw placement.
Furthermore, the fracture should have right obliquity to allow
compression across the fracture site and avoid displacement with
lag screw fixation. The ideal fracture geometry is a Grauer type
IIB fracture which is a displaced fracture extending from
anterior-superior to posterior-inferior, or a transverse
fracture.17 In addition, this method of fixation
should be avoided in osteoporotic bone, pathologic fracture, or
nonunion where fracture fixation and subsequent healing are
impaired. Based on the previous facts one would not expect to
use anterior odontoid screw fixation in the elderly population
in which osteoporosis is prevalent.
Posterior C1-C2 Fusion
Several surgical techniques have been
described to achieve posterior C1-2 fusion. These include
sublaminar wiring, C1-C2 transarticular screws, and Harms
posterior C1 lateral mass and C2 pars screws. 12,
13, 14, 37 Gallie13 described the first
posterior C1-C2 wiring technique. This technique used a single
central wire placed in a sublaminar position, under the ring of
C1 and around the C2 spinous process. The wire provided
stability and also served to secure a structural autograft in
place. Brooks and Jenkins 14
later introduced an alternative wiring technique using bilateral
sublaminar C1-C2 wires with 2 structural autograft blocks. A
major disadvantage of sublaminar wiring technique is the
potential risk of spinal cord injury while passing the wires.
Furthermore, sublaminar wires cannot be used with concomitant C1
posterior arch fracture.
An alternative method of C1-C2
stabilization is that of transarticular screws (figure 2).15
An appropriate screw trajectory should be confirmed with
fluoroscopy after patient positioning on the operative table.
The procedure should be abandoned and an alternative method of
fixation should be used if an appropriate screw trajectory
cannot be achieved due to the patients body habit such as
with morbid obesity and advanced thoracic or cervical kyphosis.
After open posterior exposure of the upper cervical spine
that usually extends from C1 to C 3 the starting point for the
screw insertion on the C 2 lateral mass is identified. The
screws are then inserted in a percutaneous fashion through two
small stab incisions at the cervicothoracic junction. The screw
is then advanced along the isthmus of C2 and into the C1 lateral
mass. In the original description of this technique the authors
used adjuvant sublaminar wiring and structural bone graft
applied over the posterior arch of C 1 and C2 lamina. The
reported fusion rates with this technique have approached 100%.15,
16, 38
However, recently some surgeons started to use C1-2
transarticular screws without adjunctive sublaminar wiring and
elect to decorticate and apply bone graft within the C1-2 joint
and over the C1 posterior arch and C2 lamina. However,
elimination of the posterior wiring produces only 2-point
fixation, which has been associated with increased flexion and
extension motion.39
There are limitations to C 1-2
transarticular screw technique that include the required
reduction of C1 on C2 before screw placement, risk of vertebral
artery injury, and potential bleeding from dissection
surrounding the C2 pedicle.37
If transarticular screws are considered, preoperative CT should
be evaluated to make sure that an appropriate and safe screw
trajectory exists.
To avoid the limitations of transarticular fixation,
Harms and Melcher have introduced a technique for screw fixation
using posterior C1 lateral mass and C2 pars screws.
Once the screws are placed, the reduction of C1 relative
to C2 can be adjusted if necessary before securing the screws
with a short rod construct. This technique produced 100% fusion
in all 37 patients at 1 year and had no neurologic, vascular, or
implant complications.
37
Biomechanical studies showed that the Brooks and Jenkins
wiring technique was 2.5 times more stable than the Gallie
wiring technique and C1-2 transarticular screw constructs have
had a 10-fold increased rotational stiffness and similar lateral
bending stiffness when compared to that of posterior wiring
techniques.40, 41, 42 Biomechanical
comparison of Harms posterior C1 lateral mass and C2 pars screws
to bilateral C1-C2 transarticular screws with Gallie wiring
showed significantly decreased motion in lateral bending and
axial rotation with both the Harms and transarticular screw
constructs. Furthermore, no significant difference was
documented between the transarticular and Harms methods. 43
Nonunion
Type II odontoid fractures are less stable, and
associated with higher nonunion rates when compared with type I
and III odontoid fractures. Factors associated with an increased
incidence of nonunion for type II odontoid fractures include
posterior fracture displacement, displacement > 5 mm, >10°
of angulation, fracture comminution, delayed treatment, and
patients older than 40 years.7,
44, 45, 46
Asymptomatic nonunions are often observed without any
active surgical intervention although this often spurs debate.
Patients with a symptomatic nonunion often present with
persistent neck pain,
myelopathy, or both. In such a case surgical management
should be considered. Several factors should be looked at
carefully before deciding on the best surgical option. These
factors include associated medical comorbidities, whether the
presenting symptom is pain only or associated with myelopathy,
and finally the status of the subaxial spine. In patients with
severe medical comorbidities that render surgical management
risky, one may elect to continue with conservative management.
Posterior C1-2 fusion is the procedure of choice for patients
presenting with a chief complaint of pain. Patients presenting
with myelopathy may require decompression that may be achieved
by resection of the posterior C1 arch and possibly a portion of
the C2 lamina.47
One may also choose to extend the instrumentation and
fusion to the subaxial spine in patients with advanced subaxial
spondylosis and spinal canal stenosis. In these cases, it will
be very difficult to know if myelopathy is related to the
odontoid nonunion or the subaxial spinal canal stenosis.
Summary
:
Despite
the frequency of odontoid fractures in elderly, there is still
lack of consensus on the best treatment option for displaced
type II odontoid fractures. This reflects the reality that there
is not yet any single ideal solution for this clinical problem.
Odontoid fractures should be evaluated with appropriate imaging
to assess the fracture itself as well as exclude other
contiguous or noncontiguous fractures.
External immobilization with a cervical collar has led to
inconsistent results. Halo vest immobilization in elderly is
associated with a significant nonunion rate and several
complications. However, some surgeons believe that a
stable nonunion achieved after external immobilization with a
cervical collar in the elderly population is an acceptable risk
when considered against the potential morbidity of surgical
intervention. Well agreed upon surgical indications are the
poly-trauma patient, the presence of a neurologic deficit, an
associated unstable subaxial spine injuries that requires
surgical fixation and a symptomatic nonunion. Surgical
management includes either anterior odontoid screw fixation or
posterior C1-2 instrumentation and fusion.
Reference :
-
Vaccaro AR, Madigan L, Ehrler DM. Contemporary management of
adult cervical odontoid fractures. Orthopedics
2000;23:110913.
-
Subach BR, Morone MA, Haid RW Jr, et al. Management of acute
odontoid fractures with single-screw anterior fixation.
Neurosurgery 1999;45:8129.
-
The contemporary treatment of odontoid injuries.
Spine. 2006 May 15;31(11 Suppl):S53-60.
-
Hanigan WC, Powell FC, Elwood PW, et al. Odontoid fractures in
elderly patients. J Neurosurg 1993;78:325.
-
Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with
special reference to the elderly patient. Clin Orthop Relat Res
1985;193:17883.
-
Ryan MD, Henderson JJ. The epidemiology of fractures and
fracture-dislocations of the cervical spine. Injury
1992;23:3840.
-
Clark CR, White AA III. Fractures of the dens. A multicenter
study. J Bone Joint Surg Am 1985;67:13408.
-
Hanssen AD, Cabanela ME. Fractures of the dens in adult
patients. J Trauma 1987;27:92834.
-
Schweigel JF. Management of the fractured odontoid with
halo-thoracic bracing. Spine 1987;12:8389.
-
CT evaluation of the pattern of odontoid fractures in the
elderly--relationship to upper cervical spine osteoarthritis.Eur
Spine J. 2005 Feb;14(1):78-83.
-
Anderson LD, DAlonzo RT. Fractures of the odontoid process of
the axis. J Bone Joint Surg Am 1974;56:166374.
-
Geisler FH, Cheng C, Poka A, et al. Anterior screw
fixation of posteriorly displaced type II odontoid fractures.
Neurosurgery 1989;25:307.
-
Gallie WE. Fractures and dislocations of the cervical spine. Am
J Surg 1939;3:4959.
-
Brooks AL, Jenkins EB. Atlanto-axial arthrodesis by the wedge
compression method. J Bone Joint Surg Am 1978;60:27984.
-
Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid
fractures: Indications, technique, and results of transarticular
screw fixation. J Spinal Disord 1992;5:46475.
-
Coyne TJ, Fehlings MG, Wallace MC, et al. C1-C2 posterior
cervical fusion: Long-term evaluation of results and efficacy.
Neurosurgery 1995;37:68892.
-
Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified,
treatment-oriented classification of odontoid fractures. Spine J
2005;5:1239
-
Shaffer MA, Doris PE. Limitation of the cross table lateral view
in detecting cervical spine injuries: A retrospective analysis.
Ann Emerg Med 1981;10:50813.
-
Diaz JJ Jr, Gillman C, Morris JA Jr, et al. Are five-view plain
films of the cervical spine unreliable? A prospective evaluation
in blunt trauma patients with altered mental status. J Trauma
2003;55:65863.
-
Reliability and reproducibility of dens fracture classification
with use of plain radiography and reformatted computer-aided
tomography. J Bone Joint Surg Am. 2006 Jan;88(1):106-12.
-
Sanchez B, Waxman K, Jones T, et al. Cervical spine clearance in
blunt trauma: Evaluation of a computed tomography-based
protocol. J Trauma 2005;59:17983.
-
Pasquale M, Fabian TC. Practice management guidelines for trauma
from the Eastern Association for the Surgery of Trauma. J Trauma
1998;44:94156.
-
Keats TE, Dalinka MK, Alazraki N, et al. Cervical spine
trauma. American College of Radiology. ACR Appropriateness
Criteria. Radiology 2000;215(suppl):2436.
-
Green RA, Saifuddin A. Whole spine MRI in the assessment of
acute vertebral body trauma. Skeletal Radiol 2004;33:12935.
-
Bednar DA, Parikh J, Hummel J. Management of type II odontoid
process fractures in geriatric patients; a prospective study of
sequential cohorts with attention to survivorship. J Spinal
Disord 1995;8:1669.
-
Muller EJ, Wick M, Russe O, et al. Management of odontoid
fractures in the elderly. Eur Spine J 1999;8:3605.
-
Dunn ME, Seljeskog EL. Experience in the management of odontoid
process injuries: An analysis of 128 cases. Neurosurgery
1986;18:30610.
-
Ziai WC, Hurlbert RJ. A six year review of odontoid fractures:
The emerging role of surgical intervention. Can J Neurol Sci
2000;27:297301
-
Type II odontoid fractures in the elderly: early failure of
nonsurgical treatment.
Neurosurg Focus. 2000 Jun 15;8(6):e7.
-
Halo-vest immobilization increases early morbidity and mortality
in elderly odontoid fractures.J Trauma. 2006 Jan;60(1):199-203.
-
Glaser JA, Whitehill R, Stamp WG, et al. Complications
associated with the halo-vest. A review of 245 cases. J
Neurosurg 1986;65:7629.
-
Bohler J. Anterior stabilization for acute fractures and
nonunions of the dens. J Bone Joint Surg Am 1982;64:1827.
-
Sasso R, Doherty BJ, Crawford MJ, et al. Biomechanics of
odontoid fracture fixation. Comparison of the one- and two-screw
technique. Spine 1993;18:19503.
-
Jenkins JD, Coric D, Branch CL Jr. A clinical comparison of one-
and two-screw odontoid fixation. J Neurosurg 1998;89:36670.
-
Aebi M, Etter C, Coscia M. Fractures of the odontoid process.
Treatment with anterior screw fixation. Spine 1989;14:106570.
-
Dickman CA, Foley KT, Sonntag VK, et al. Cannulated screws for
odontoid screw fixation and atlantoaxial transarticular screw
fixation. Technical note. J Neurosurg 1995;83:1095100.
-
Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw
and rod fixation. Spine 2001;26:246771.
-
Dickman CA, Sonntag VK. Posterior C1-C2 transarticular screw
fixation for atlantoaxial arthrodesis. Neurosurgery
1998;43:27580.
-
Henriques T, Cunningham BW, Olerud C, et al. Biomechanical
comparison of five different atlantoaxial posterior fixation
techniques. Spine 2000;25:287783
-
Hanley EN Jr, Harvell JC Jr. Immediate postoperative stability
of the atlantoaxial articulation: A biomechanical study
comparing simple midline wiring, and the Gallie and Brooks
procedures. J Spinal Disord 1992;5:30610.
-
Montesano PX, Juach EC, Anderson PA, et al. Biomechanics of
cervical spine internal fixation. Spine 1991;16:S106.
-
Grob D, Crisco JJ III, Panjabi MM, et al. Biomechanical
evaluation of four different posterior atlantoaxial fixation
techniques. Spine 1992;17:48090.
-
Melcher RP, Puttlitz CM, Kleinstueck FS, et al. Biomechanical
testing of posterior atlantoaxial fixation techniques. Spine
2002;27:243540.
-
Hadley MN, Dickman CA, Browner CM, et al. Acute axis fractures:
A review of 229 cases. J Neurosurg 1989;71:6427.
-
Hadley MN, Browner C, Sonntag VK. Axis fractures: A
comprehensive review of management and treatment in 107 cases.
Neurosurgery 1985;17:28190.
-
Factors associated with nonunion in conservatively-treated
type-II fractures of the odontoid process. J Bone Joint Surg Br.
2004 Nov;86(8):1146-51
-
Effectiveness of multiple-level decompression in laminoplasty
and simultaneous C1 laminectomy for patients with cervical
myelopathy. Eur Spine J. 2006;15(9):1367-74.
|


