|
Abstract:
Tibial plateau fractures involve the articular surface and
condylar portion of the proximal tibia. These fractures occur as
a result of severe trauma on the knee joint; therefore, the
associated soft tissue injuries are frequently seen with these
fractures in popliteal fossa. Neuro-vascular injury is one of
the complicated damages that contain popliteal artery thrombosis
in the form of direct intimal injury or arterial disruption.
Possible plantar arc thrombosis as an embolic complication of
popliteal artey intimal flap in the form of “traumatic blue toe
syndrome” is a rare concomitant clinical entity with this
fracture which has not been reported in our experience. This is
a report of a minimal displaced fracture of the tibial plateau
in a young patient who was admitted for driving injuries with
cyanosis of four toes and severe plantar pain due to ischemic
foot. He had normal symmetrical pedal pulses, but developed
gangrene of toes leads to distal foot amputation.
Keywords: Tibial plateau fracture,
popliteal artery, foot gangrene, blue toe Syndrome.
J.Orthopaedics 2007;4(4)e17
index.htm
Introduction:
Vascular injuries coexisting with fractures are detected in
nearly 50% of traffic accidents (1) in about young age males
(mean 23-33.2) (2, 3, 4, 5, 6). Lower extremity arteries are
more affected and damaged due to knee dislocation, distal
femoral or proximal tibial fractures (1, 2, 5, 6, and 7).
Clinical signs have insidious presentation or may be overwhelmed
by the severity and urgency of fracture types especially those
needed emergency surgical intervention. In comparison, popliteal
artery and branches in calves are the most common involved
arteries in the lower limbs (4, 5, 6, 7) while brachial artery
is the most prevalent in the upper extremities (8, 9, 10, 11).
It is crucial that pedal pulses also to be considered in the
first clinical impression of the surgeons as they reflect the
main early signs of arterial insufficiencies to be confirmed
following the ischemic symptoms. Arterial disruption(74%) then
intimal laceration advocated for the main pathologic site of
injury could be etiologic for micro embolization or total
thrombosis of damaged artery(1,5,7,12). Fractures produced by
direct high energy mechanism such as tibial plateau types, are
responsible for concomitant neuro-vascular damages that endanger
the limb and end to severe complications (13, 14, 15). Delay in
surgery, blunt trauma, extensive soft tissue damages in
combination with orthopedic and vascular injuries are associated
with increased risk of amputation (4, 5, 7, 10, 16, and 17).
Hereby, we describe a patient with this type of fracture in whom
distal foot amputation was performed for his foot gangrene due
to thrombosis of deep plantar arc and toe arteries
Case Report:
A 19-years old man was admitted to our emergency department
after a vehicle road traffic accident. He was an unrestrained
driver who was ejected from his car during his crush accident.
His general condition was stable on admission (GCS 15) and only
complained of severe left thigh and right knee joint pain
without any abrasion, laceration or obvious skin contusion
except for his right hand hematoma and ecchymosis. Pedal pulses
of the both foot were symmetrically normal and also had no any
neurological deficit. Midshaft fracture of the left femur and a
minimal displaced Schatzker type IV fracture of the right tibial
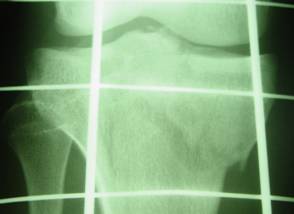
plateau were seen by radiological assessment (fig.1). following
a routine and through examination at emergency department, lower
limbs were splinted; then, he transferred to the orthopedic
department and Enoxaparin ( clexan ) 40 u/daily was injected
subcutaneously. After 36 hours of injury, open reduction and
internal fixation of the left femur and right tibial plateau
fractures was performed (fig, 2). The knee joint was stable
without any sign of instability or dislocation. The day after
operation, we found his right toes pale and cyanotic because of
distal plantar arc thrombosis with complaining of tingling and
coolness. He developed gangrene in spite of prescribed heparin
in 4th days of admission. (Fig, 3, 4). Doppler ultrasound study
identified no abnormal signals in the vascular flow in popliteal
artery and its branches in his calf and proximal foot; but, some
endo-luminal irregularities in distal popliteal artery have been
reported simultaneously. Amputation of three medial toes and
debridement of the necrotic skin of distal planter foot was
performed. The plantar aspect of the foot was repaired in the
form of advanced skin graft two weeks later, because his foot
gangrene was dry and mumificated. MESS (Mangled Extremity
Severity Score) was not applicable.
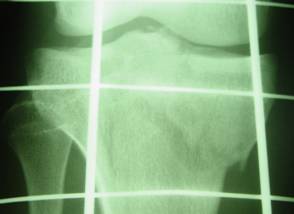
Fig 1. Right tibial plateau
fracture

Fig 2. Fixation of plateau fracture

Fig 3. Ischemia & Gangrene of the toes

Fig 4. demarcated level of foot gangrene 14 days after
injury

Fig 5.
amputation of the toes
Discussion:
Tibial plateau fracture and its severity and complexity in young
adults usually produced by high-energy trauma. This can lead to
comminuted fractures with significant associated ligamentous and
neuro-vascular injuries needed careful clinical assessment of
knee-soft tissue envelope (13, 14, and 15). These fractures are
resulted from a combination of axial loading of the femur on the
tibil condyles with varus or valgus force (19). Thus, the
capsular, ligamentous and meniscal injuries also coexist with
this kind of fracture (20). One and a half percent to 4.6% of
patients hospitalized with blunt extremity trauma have
associated vascular compromise produced by injuries including
knee dislocations, displaced medial tibial plateau fractures,
displaced bicondylar fractures of the knee, and floating joints
(21).These fractures are rare with low energy trauma, but
existing high energy displaced fractures with Schatzker types
“IV, V, VI” carry a high risk of injury to the popliteal artery
and its branching (22).
The most common site of injury is in popliteal/tibio-peroneal
trunk and its variable causes of arterial injury can expectantly
be entrapment, contusion or direct lacerations, internal
traction leading to intimal damages and flapping or intramural
hematoma (5, 6, 23). Mural intra luminal thrombosis which is
unstable in the first hours of formation may become mobile in
the result of fracture site movements persuading distal emboli
to be fixed as an early or late manifestation of limb ischemia.
Even, during elective orthopedic joint surgery and manipulation
of the injured limb there is strong possibility of any unwanted
new arterial damage with thrombosis and involvement of popliteal
artery as the most common abnormality and site of arterial
injury. This kind of associated problem may be represented
clinically with at least more than 24 hours delay in diagnosis
(25% of cases) and also is more common during redo procedures
and in patients with preexisting atherosclerosis (24). Overall,
early considered support consisting of the minimum delay for
admission after injury(=/<3 hours)(1,8,10,18), golden timed
autogenous vein graft vascular repair following by fixation of
fracture site simultaneously and prompt post operative handling
are the best accepted treatment ways; though, the amputation
rate with the about-knee popliteal artery injuries is too high
(4,6,7,11,12,18).
In this patient, the fracture of tibial condyles was minimally
displaced without knee dislocation. We suppose that our patient
sustained a progressive trombosed intimal flap arterial injury
in which there has been strong possibility of an unobstructed
mural thrombosis of popliteal artery damage due to high energy
trauma of the knee joint. It seems the intimal flap injury would
be caused by direct blunt soft tissue trauma, because condylar
fracture of tibia was minimally displaced. Under these
circumstances, knee movement, or elective open reduction and
fixation procedure could force the clot to lodge in deep
arterial arc of right foot in a rare form of traumatic blue toe
syndrome.
Reference :
1- Piatek S, Burger T, Halloul Z, Westphal T,Holmenschlager
F,Winckler S. Arterial vascular injuries in fractures and
dislocations. Zentralbl Chir. 2001; 11(6):962-4.
2- Subasi M, Cakir O, Kesemenli C, Arslan H, Necmioglu S, Eren
N. Popliteal artery injuries associated with fractures and
dislocations about The knee. Acta Orthop Belg. 2001, Jun;
67(3):259-66.
3- Abou–Sayed H, Berger DL. Blunt lower-extremity trauma and
popliteal Artery injuries: revisiting the case for
selective arteriography. Arch Surg. 2002 May; 137(5):585-9.
4- Cakir O, Subasi M, Erdem K, Eren N. Treatment of vascular
injuries Associated with limb fractures. Ann R Coll Surg
Engl. 2005 Sep;87(5):348-52.
5- Lakhwani MN, Gooi BH, Barras CD. Vascular trauma in Penang
and Kuala Lumpur Hospitals. Med J Malaysia. 2002 Dec;
57(4):426-32.
6- Rozycki GS, Trembly LN, Feliciano DV, McClelland WB. Blunt
vascular Trauma in the extremity: diagnosis, management, and
outcome. J Trauma. 2003 Nov; 55(5):814-24.
7- Zhao L, Jie Q, Ye M, Liu Q, Huang Y. Treatment of limb
arterial injuries Caused by traffic accidents. Chin J Traumatol.
2002 Oct; 5(5):303-6.
8- Iriz E, Kolbakir F, Sarac A, Akar H, Keceligil HT, Demirag
MK. Retrospective assessment of vascular injury: 23 years
of experience. Ann Thorac Cardiovasc Surg. 2004 Dec;
10(6):373-8.
9- Brown KR, Jean-Claude J, Seabrook GR, Towne JB, Cambria RA.
Determinates of functional disability after complex upper
extremity Trauma. Ann Vasc Surg. 2001 Jan; 15(1):43-8.
10- Menakuru SR, Behera A, Jindal R, Kaman L, Doley R,
Venkatesan R. Extremity vascular trauma in civilian population:
a seven- years review From North India. Injury. 2005 Mar;
36(3):400-6.
11- Wali Ma. Upper limb vascular trauma in the Asir region of
Saudi Arabia. Ann Thorax Cardiovascular Surg. 2002 Oct;
8(5):298-301.
12- Guraya SY. Extremity vascular trauma in Pakistan. Saudi Med
J.2004 Apr; 25(4):495-501.
13- Berkson EM, Virkus WW. High-energy tibial plateau fractures.
J Am Acad Orthop Surg. 2006 Jan; 14(1):20-31.
14- Pogliacomi F, Verdano MA, Frattini M, Costantino C, Vaienti
E, Soncini G. Combined arthroscopic and radioscopic management
of tibial plateau fractures: report of 18 clinical cases.
Acta Biomed Ateneo Parmense. 2005 Sep; 76(2):107-14.
15- Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS,
Mavrogenis AF. Korres DS, Soucacos PN. Complications after
tibial plateau fracture Surgery. Injury. 2005 Aug 20; [Epub
ahead of print].
16- Palmieri F, Pulcini G, Piardi T, Ottaviani GM, Longobardi U,
Pouche A. Vascular trauma of lower limbs. Minerva Chir. 2000
Dec; 55(12):841-6.
17- Galambos B, Tamas L, Zoldos P, Czigany T, Jakab L, Nemeth J,
Csonge L. Vascular injuries in everyday practice. Zentralbl
Chir. 2004 Apr; 129(2):81-6.
18- Cihan HB, Gulcan O, Hazar A, Turkoz R. Peripheral vascular
injuries. Ulus Travma Derg. 2001 Apr; 7(2):113-6.
19- Shrestha BK, bijukachhe B, Rajbhandary T, Uprety S, Banskota
AK. Tibial plateau fractures: four years review at B & B
hospital. Kathmandu Univ Med J (KUMJ). 2004 Oct-Dec;
2(4):315-23.
20- Zakrzewski P,Orlowski J. Meniscuses and ligaments injuries
in tibial Plateau fractures in comparative evaluation of
clinical, intraoperative and
MR examination. Chir Narzadow Ruchu Ortop Pol.
2005;70(2):109-13.21- Levy BA, Zlowodzki MP, Graves M, Cole PA.
Screening for extremity Arterial injury with the arterial
pressure index. Am J Emerg Med. 2005 Sep; 23(5):689-95.
22- Tracy JW, Donald AW. Fractures of the proximal tibial and
fibula. In: Rockwood C, Green D. Fractures in adults, 5th
edition. Lippincott Company. 2002: P 1834-35.
23- Frykberg ER. Popliteal vascular injuries. Surg clinic North
Am. 2002; 82:67-89.
24- Wilson JS, Miranda A, Johnson BL, Shames ML, Back MR, Bandyk
DF. Vascular injuries associated with elective Orthopedic
procedures. Ann Vasc Surg. 2003 Nov;17(6):641-4. Epub 2003 Oct
13.
|