|
Abstract:
Design: Retrospective study
Objectives: Analyze
short-term effects of Rigid (Group R) Versus Dynamic(Group D)
instrumentation in terms of Subjective evaluation & Patient
oriented outcome.
Materials
and Methods: 50 patients (Male 17: female 33), 25 in each
group. Evaluation based on pre & postoperative Visual
Analogue Scale (VAS) and Oswestry Disability Index (ODI) at
fixed interval at 6 weeks, 6 months, 1 and 2 years.
Results:
Mean preoperative VAS for LBP (Group D) was 6.9, and decreased
at 24 months postoperative to 3.4 and for Group R was 7.6 to
3.7. Mean VAS for leg pain for Group D was from 6.2 to 2.1 at 24
months and for Group R 6.9 to 3.0. Mean ODI for Group D was from
54 to 29 and for
Group R it was 56 to 39, suggesting less improvement in cases
operated with rigid stabilization compare to Dynesys system. ODI
for Group D, follows descending pattern as scores 43.0, 38, 32.5
and 29 , whereas for Group R was 27, 30, 35 and 39 at 6 wks, 6
months, 1 and 2 yrs, respectively. There is no age related
difference in outcome in both systems. Disc prolapse patients
improved significantly with Rigid system, while spine
instability had better outcome with Dynesys.
Discussion:
Rigid fixation, there is no consistent improvement in the ODI,
up to 2 yrs follow up. In rigid fixation system even after
fusion the instrumentation is in place, which contributes to
unfavorable outcome in relation to probably loss of lumbar
lordosis, and progression of degenerative process at adjacent
levels contributing to less favorable clinical outcome.
Conclusion:
Dynesys has better outcome in older age group patients, stenosis
and listhesis. Dynesys can be considered as an effective option
to rigid stabilization systems.
J.Orthopaedics 2007;4(3)e7
Study Design:
Retrospective comparative clinical study on a consecutive series
of 25 patients in each group.
Keywords:
Dynesys
- semi rigid spinal instrumentation system; Rigid fixation -
pedicle screw and rod system with fusion; VAS- Visual Analogue
Score; ODI- Oswestry Disability Index
Background
Data:
Lumbar
spine fusion with rigid instrumentation for degenerative spinal
disorders seems to increase the fusion rate. However, rigid
instrumentation may be associated with some undesirable effects,
such as increased low back pain following decrease of lumbar
lordosis, fracture of the vertebral body and pedicle, pedicle
screw loosening, and adjacent segment degeneration11. The use of
semi rigid and dynamic devices has been advocated to reduce such
adverse effects of the rigid instrumentation and thus to achieve
a more physiologic bony fusion.
Dynesys
is design to preserve intersegmental kinematics and alleviate
loading of facet joints and they’re by preserving articular
function2&3. In the course of degenerative process, during
which the segment undergoes various anatomic alterations, there
are significant changes in both moion characteristics of, and
the load distribution across the affected segments4.
This
new system for treating Lumbar degenerative pathology based on
lumbar stabilization and preservation of articular function, as
opposed to traditional arthrodesis restrictions3
The
concept of spinal fusion originally arose from the notion that a
degenerated motion segment is often”unstable” or shows “
Movement abnormalities,” and that accordingly, the elimination
of motion in the affected segment would prevent it from
undertaking the movements associated with the generation of
pain. Recent thinking, however, suggests that the preservation
of movement per say may not be the most important factor
accounting for the success of fusion.
By
preserving flexibility of a motion segment may allows greater
physiological function7.
Rigid
fixation system for fusion only, has to serve temporary
stabilization until fusion has taken place while on the other
hand, the soft stabilization system has to provide stability
throughout its life8.
This
study is to compare the postoperative effects of a rigid versus
dynamic instrumentation for degenerative spine disease and
stenosis and to investigate if a dynamic spine system can
replace the commonly used rigid systems in order to avoid the
above mentioned disadvantages of rigid fixation.
Objectives:
1)
To analyze the short-term effects of Rigid Versus Dynamic
instrumentation on
lumbar spine surgery.
2)
Subjective evaluation & Patient oriented outcome of the
result.
3)
To evaluate complications rate associated with both system.
Materials And
Methods:
Patients:
This study analyzes series of 50 adult patients (Male 17: female
33), 25 in Group R (Rigid Fixation) and 25 patients in Group D
(Dynesys System) operated at District General Hospital, by same
Surgeon Using Rigid and Dynesys System.
Clinical
evaluation for both groups was based on pre & post operative
Visual Analogue Scale (VAS) and Oswestry Disability Index (ODI)
at Fixed interval at 6 weeks, 6 months, 1 and 2 years. Mean age
of the study Group R was 49 yrs (range 23-74 yrs) and 52yrs
(range 24 – 70 yrs) for group D. We analyzed the outcome of
both Systems in different indications like Lumbar Stenosis, Disc
Prolapse, and Spondylolisthesis and with Degenerative Disc
Disease.
In-group
D, 6 patients and group R 1 patient had pedicle screw Fixation
of more than two levels. All patients were investigated with pre
& postoperative standard X-ray and MRI of Lumbar spine.
Preoperative
evaluation: Preoperative
evaluation included patient history, imaging, and clinical and
neurological evaluation by the treating surgeon.
Surgery:
Both the systems consist of pedicle screws made of Ti-Al-Nb
forge alloy. The screws are connected with a polyethylene
terephthalate cord (Dynesys) / Ti-Al-Nb Rods. Tethering the cord
and selecting the appropriate length of the spacer/rod between
the screws may apply segmental distraction or compression.
The
procedure was performed in prone position. A midline approach,
with dissection of the erector spinae muscles, provided access
to the bony anatomy of the lumbar spine. If indicated
decompression of the spinal canal was performed first. Insertion
of the pedicle screws was carried out under radiologic control
using a C-arm. The polycarbonate urethane spacer was cut
according to the measure distance between the screws, with the
length being chosen to compensate any existing lordosis or
kyphosis. The central cord and the spacer were then locked
within the screw heads. No postoperative brace was given, and
patients were mobilized if safe to do.
Radiologic
and Clinical follow–up:
The first post op x rays were examined and any technical error,
or other complications were documented.
Results:
All
patients were evaluated up to 24 months after surgery. The
results were analyzed based of the clinical Scores of VAS &
ODI system and also study of complications by analyzing the X
ray and MRI as indicated.
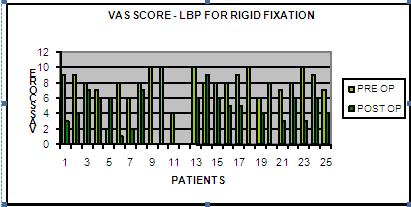
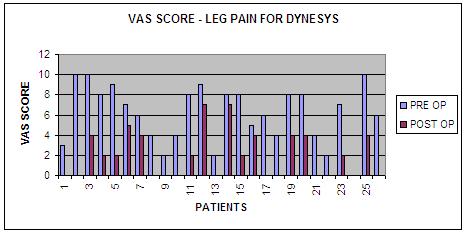
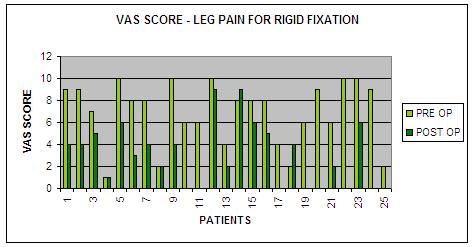
Regarding
VAS scoring system we considered VAS for Low Back Pain (LBP) and
Leg Pain separately for surgical outcome analysis.
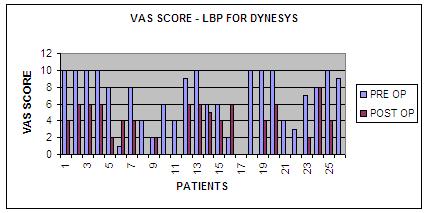
The mean
preoperative scores of Visual Analogue Scale for low back Pain
for (Group D) was 6.9, and decreased after surgery at end of 24
months follow up to 3.4 and for Group R same was 7.6 and post op
score was improved to 3.7.
Similarly
mean scores of Visual Analogue Scale for Leg pain for (Group D)
was decreased from pre op 6.2 to 2.1 at end of 24 months follow
up., and same was improved from 6.9 to 3.0 for Group R.
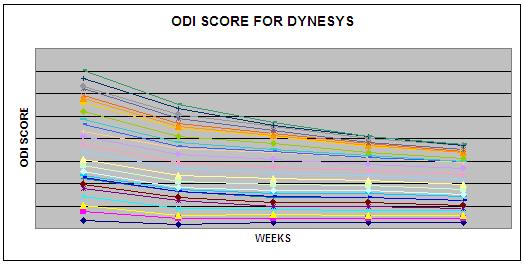
The
final results of ODI scoring for group D were 29 at end of 24
months post operative follow up, with respect to 54 score, prior
to treatment and for group R it was 39 at post op follow up from
pre operative score of 56, suggesting less improvement in cases
operated with rigid stabilization compare to Dynesys system.
The
improvement pattern for ODI score for Group D was observed at
different interval, which follows a descending pattern as 43.0,
38, 32.5 and 29 at 6 wks, 6 months, 1 yr, and 2 yrs,
respectively that represents an improvement of 20%, 29%, 40% and
46%.
The
improvement pattern for ODI score for Group R was observed at
different interval, which follows a different pattern from group
D as 27.0, 30.5, 35 and 39 at 6 wks, 6 months, 1 yr, and 2 yrs,
respectively that represents an improvement of 51%, 46%, 37% and
30%.
In
patients operated for more than two segments of Dynesys fixation
the ODI score was 52, and 35 preop and post op respectively,
which suggests less improvement in clinical outcome when
compared with entire study group.
In
this study we compared clinical outcome in age group more than
50 yrs, (Group A), with those in the age group less than 50 yrs
(Group B).
In
Group A (Dynesys) mean ODI score was 50
and 25, pre and post operative respectively, that suggests
>50 % improvement in clinical outcome.
In
Group A (Rigid) mean ODI score was 52 and 39, pre and post
operative respectively, that suggests >25 % improvement in
clinical outcome.
Group
B (Dynesys) mean ODI Score was 62, and 34, pre and post
operative respectively.
Group
B (Rigid) mean ODI Score was 60, and 39, pre and post operative
respectively
This
suggests there is no age related difference in final clinical
outcome in relation to this both fixation systems.
When
analyzing the final outcome for Dynesys
in relation to different surgical indications, it was
observed that more than 50% improvement in the ODI score, from
49 to 21, pre and post operative respectively in lumbar
instability especially spondylolisthesis and Lumbar canal
Stenosis (post laminectomy).
Final
Outcome for rigid fixation in relation to different surgical
indications was observed with different pattern, Disc prolapse
ODI improved from 76 to 25, for Stenosis from 46 to 37, and for
Listhesis it changed from 50 to 37.
Complications:
With
regard to complications, we would like to point out total 10
(20%) cases, 3 superficial infections, 1 seroma, and 4 cases due
to technical error and 2 cases had nerve root irritation.
|
|
Rigid fixation
|
Dynesys
|
|
Infection
|
1
|
3
|
|
Nerve irritation
|
2
|
0
|
|
Technical error
|
3
|
1
|
Discussion:
This
study shows that Rigid instrumentation applied over a short area
for Disc Prolapse pathology OF lumbar spine has significant
clinical improvement by 70% of both self-assessment and pain
score. But in case of Dynesys instrumentation applied for
indications including Stenosis and Listhesis of lumbar spine has
significant clinical improvement by >50% of both
self-assessment and pain score.
From
this study we infer that VAS system for back pain and leg pain
shows significant improvement in final assessment score at 2 yrs
follow up, using Dynesys system, as a method of dynamic fixation
except in some patients, in whom results are not up to
expectation because of associated post operative complication
like infection and screw malposition. Though our study did not
show any more complications related to this system itself.
As
Dynesys is not a rigid method of fixation and fusion, it has
been observed that, there is gradual improvement of symptoms and
score over a period of two years follow up as per the graph.
It
has been observed that in using Rigid fixation, there is no
consistent improvement in the ODI score, up to 2 yrs follow up.
Though initial period of first 6 wks follow up shows significant
improvement in ODI score, but subsequent follow up scoring shows
increase in symptoms and unfavorable over all long term outcome.
Rigid
fixation system is for fusion only, has to serve temporary
stabilization until fusion has taken place19 while in rigid
fixation system even after fusion the instrumentation is in
place which contributes to unfavorable outcome in relation to
probably loss of lumbar lordosis, and progression of
degenerative process at adjacent levels6.
The
dynamic neutralization obtained using this system, should not be
considered as an arthrodesis, but this device has been advocated
to achieve more physiological bony fusion. With this system NO
bone grafting is necessary therefore donor site morbidity can be
avoided. Dynesys system maintains enough stability to prevent
further progression of spondylolisthesis (instability).
Even
some literature3 supports that dynesys system has limitations in
elderly age group with osteoporotic bone with severe segmental
macro-instability, from our results we imply that, in older age
group Dynesys has better clinical outcome compare to Rigid
fixation.
Conclusion:
This
study supports the belief that the dynamic system can be used
with the same
indications with the rigid in degenerative lumbar spine because
it can offer equally good short-term results regarding clinical
outcome of surgery, while it has been previously mentioned as
per our study, Dynesys has better outcome in older age group
patients, and specific indications like Stenosis and listhesis5.
Dynesys
can be considered as an effective option to rigid stabilization
systems, in terms of patient based clinical outcome, and
avoidance of complications of rigid system like, screw
loosening, fractures of vertebral body, back pain because of
loss of lumbar lordosis , morbidity related to bone grafting.
Because
of similar clinical and radiological data and no significant
rate of complications related to either implant, in both groups
and the relative small number of patients included in each
group, it is difficult for authors to make any definitive
recommendation in favor of any instrumentation.
It
is very essential to have prospective randomized controlled
trial to support practice of evidence-based medicine.
Reference :
-
Dynamic stabilization in addition to decompression for lumbar
spinal stenosis with degenartive spondylolisthesis, Spine 2006,
Feb 15; 31(4): 442-9.
-
Influence of dynamic stabilization system on load bearing of a
bridged disc: an in vitro study if intradiscal pressure, Eur
spine J 2006, Jan 21: 1-10.
-
Posterior Dynamic Stabilization System: DYNESYS, Orthopedic
Clinic Of North America, 2005, July; 36(3): 363-72.
-
Kirkaldy- Willis WH,Farfan H, Instability of the Lumbar spine.
Clin Orthop 982:165:110-23.
-
Application of a dynamic pedicle screw system for lumbar
segmental degeneration- comparison of clinical and radiological
results for different indications, Z Orthop Ihre Grenzgeb
(German), 2004 Mar-April;142(2);166-73
-
Rigid, semi rigid versus dynamic instrumentation for
degenerative lumbar spinal stenosis: a correlative
radiological and clinical analysis of short-term results, Spine,
2004 Apr 1; 29(7): 735-42.
-
Dynamic neutralization system for the spine: a multi center
study of a novel non fusion system, Eur Spine J, 2002, Oct; 11.
- Dynamic stabilization devices in the treatment of Low
Back Pain, Orthopedics
Clinic North America, 2004, Jan; 35(1): 43-56.
|