|
Abstract:
We
report on the case of a 31-year-old man with pain in the
thoracic spine caused by a kick during soccer. Based on typical
radiological features, i.e. a vacuum cleft phenomenon and a
higher density of the vertebral body of T7, which matched the
clinical findings, i.e. the preceding trauma and the
characteristic level of the painful vertebra, the diagnosis Kümmell’s
disease was made. The typical collapse of the traumatised
vertebral body, as to be expected in Kümmell’s disease,
failed to appear. Further examination revealed a primary
lung-carcinoma with several metastases, including vertebra T7.
There is no consensus how to diagnose Kümmell’s disease. This
case report illustrates that even if radiological and clinical
features are typical of Kümmell’s disease, it is necessary to
confirm the diagnosis with a biopsy.
J.Orthopaedics 2007;4(3)e13
Keywords:
Kümmell’s
disease; vertebral osteonecrosis
Introduction:
In
1891, the German surgeon Hermann Kümmell first described a
patient with a delayed collapse of a traumatised vertebral
body.1-4 Since then this rarely reported and poorly understood
phenomenon is called Kümmell’s disease.2,3
It is caused by osteonecrosis of a vertebral body,
probably due to a decreased blood-supply after trauma.1-4
The
clinical presentation will typically be a male of middle age
with backache after a minor trauma. An asymptomatic period will
usually follow. After weeks to months, osteonecrosis of the
vertebral body predictably results in a collapse, which causes
severe pain. Kyphotic deformity and neurologic symptoms may then
occur.1,3,4 The initial radiograph of the spine usually
doesn’t show a fracture of the traumatised vertebral body.2,3
On later radiographs and CT-imaging the intravertebral vacuum
cleft phenomenon (an accumulation of gas in a vertebral body)
combined with a subcortical fracture and hyperdensity of the
vertebral body, are typical for Kümmell’s disease.1,2,4
On MR images the intravertebral gas is of low signal
intensity on all sequences. Although relatively non-specific, a
bone-scan shows early activity.3,4
Histopathology
demonstrates spongiosa with multiple haemorrhages, atrophy of
the bony framework, multiple microscopic fractures, inflammatory
changes and paravertebral fibrosis.1,4
Case
Report :
A healthy
31-year-old man was seen for evaluation of persistent backache
after a kick in his back during a game of soccer two months
previously. Physical examination only revealed pain at the level
of vertebra T7. Radiographs and CT-imaging showed the following
changes of the vertebral body of T7: A higher density of the
vertebral body, a small collapse of the upper endplate, a
subcortical fracture and intravertebral accumulation of gas
(vacuum cleft phenomenon) (figures 1 and 2).

Figure
1: X-ray of T7
Figure
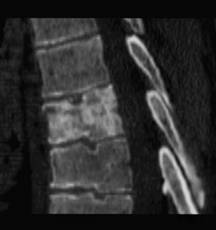
2: Computed Tomography of T7
(Radiograph
and CT-imaging show the following changes of the vertebral body
of T7: A higher density of the vertebral body, a small collapse
of the upper endplate, a subcortical fracture and intravertebral
accumulation of gas (vacuum cleft phenomenon).
)
Based
on the history, clinical examination and these very typical
radiological features the diagnosis Kümmell’s disease was
made. The orthopaedic surgeon prescribed a thoracic brace.
During the following months the pain diminished and the
radiographs taken at two weeks interval showed no further
deterioration of the vertebral body T7. Four months after the
first visit, only slight pain persisted. The patient however
developed a painful sacroiliac joint on the right side. A
radiograph of the pelvis showed an osteolytic lesion of the
right os ilium. A total body bone scan demonstrated an extensive
amount of hotspots throughout the whole skeleton. An extensive
blood-examination demonstrated numerous abnormalities due to
bone metastasis.
A
CT-scan showed a tumour in the upper lobe of the right lung as
well as osteolytic and osteosclerotic lesions in several
vertebral bodies, which were (even retrospectively) not visible
on the x-rays taken earlier. A biopsy of the os ilium revealed a
metastasis of a primary lung-carcinoma.
Discussion :
Several
authors wrote about the intravertebral vacuum cleft phenomenon
as typically for Kümmell’s disease. Maldague et al 5 first
described the intravertebral vacuum cleft phenomenon in 1991.
They and others authors 6 advocate this phenomen to be
pathognomic for Kümmell’s disease or other cases of
spontaneous vertebral osteonecrosis. Bhalla et al 6 conclude
that recognition of the near-certain benign significance of a
linear intravertebral gas collection revealed by radiography may
prevent unnecessary imaging or biopsy in a patient with a
suggestive vertebral compression deformity.
The
radiological features of the intravertebral vacuum cleft sign in
Kümmell’s disease differ according to several authors.
Osterhouse et al 7 demonstrated the dynamic entity of the
intravertebral vacuum in Kümmell’s disease, which is subject
to changes in size and shape. Others found correlation between
shape of the vacuum and its benign or malignant character. 8
While these authors wrote about the typical vacuum cleft
phenomenon in Kümmell’s disease, Dupuy et al 9 demonstrated
atypical fluid collections in vertebral fractures with avascular
necrosis.
Articles
report about intravertebral gas and fluid collections in
osteoporotic fractures. Lafforgue et al 10 hypothesize that the
vacuum sign could simply be the result of migration of an
intradiscal gaseous collection through the fractured endplate of
some osteoporotic collapses. Mirovsky et al 11
found a vacuum sign within 26 of 101 osteoporotic
vertebral fractures in a retrospective research. They reject the
vacuum sign as pathognomic for Kümmell’s disease. The
correlation of vacuum sign with fracture non-union was made in
this article.
McKiernan
et al 12 also
demonstrate intravertebral clefts in osteoporotic vertebral
fractures. They found these radiological features
indistinguishable from Kümmell’s disease. Baur et al 13
described the displacement of intravertebral gas by fluid in
cases of osteoporotic fractures. Naul et al 14 also described
five patients with plain radiographic evidence of a compressed
vertebra containing an intravertebral vacuum cleft. While these
articles demonstrate the occurrence of intravertebral gas in Kümmell’s
disease and osteoporotic fractures of the vertebra, several
articles have been published about the combination of
intravertebral gas and malignancy. Kumpan et al 8
presented a case of intraosseous vacuum in a malignant
vertebral collapse. Baur et al 13 described the displacement of
intravertebral gas by fluid in cases of neoplastic fractures. A
case-report shows a metastatic Ewing’s sarcoma involving the
vertebral spine and mimics Kümmell’s disease.15
Some
authors believe that gas within a vertebral body is even not
diagnostic for osteonecrosis, osteoporotic fractures or
neoplasm. They advise us also to differentiate between spinal
infection, degenerative cysts and Schmorl’s nodes.
In
this patient with backache, we rejected the diagnosis of a
degenerative cyst and an osteoporotic fracture because of his
age. The clinical appearance was not suggestive for an
infectious cause. To make a differentiation between Kümmell’s
disease and a metastasis, a biopsy was recommendable.
Conclusion:
It
is important to be aware of the existence of neoplastic
metastasis, which mimics the clinical and radiological features
of Kümmell’s disease. With the fast development in
radiological equipment, a vertebral biopsy becomes less invasive
with very few complications. The described case, strengthened by
several articles, demonstrates the importance of confirming the
diagnosis of Kümmell’s disease with a biopsy.
Reference :
-
Brower A, Downey E. Kümmell disease: Report of a case with serial
radiographs. Radiology 1981; 141: 363-364.
-
Hermann G, Goldblatt J, Desnick R. Kümmell disease: delayed
collapse of the traumatised spine in a patient with Gaucher type
1 disease. The British Journal of Radiology 1984; 57: 833-835
-
Van Eenenaam P, El-Khoury G. Delayed post-traumatic vertrebral
collapse (Kümmell’s disease): Case report with serial
radiographs, computed tomographic scans and bone scans. Spine
1993; 18: 9: 1236-1241
-
Young WF, Brown D, Kendler A, Clements D. Delayed post-traumatic
osteonecrosis of a vertebral body (Kümmell’s disease). Acta
Orthopaedica Belgica 2002; 68: 1
-
Maldague BE, Noel HM, Malghem JJ: The intravertebral vacuum
cleft: a sign of ischemic vertebral collapse. Radiology 1978,
129: 23-29
-
Bhalla S, Reinus WR. The linear intravertebral vacuum: a sign of
benign vertebral collapse. American Journal of Roentgenology
1998; 170: 6:1563-9
-
Osterhouse MD, Kettner NW. Delayed post-traumatic vertebral
collapse with intravertebral vacuum cleft: a
case report. Journal
of Manipulative and Physiological Therapeutics 2002; 25: 4: 270-5
-
Kumpan W , Salomonowitz E , Seidl G. The intravertebral
vacuum phenomenon . Skeletal Radiology 1986; 15 : 444 – 7
-
Dupuy DE, Palmer WE,
Rosenthal DI. Vertebral fluid collection associated with
vertebral collapse. Am J Roentgenology 1996; 167: 1535-1538
-
Lafforgue P, Chagnaud C, Daumen-Legre V. The intravertebral
vacuum phenomenon. Migration of intradiscal gas in a fractured
vertebral body? Spine 1997; 22: 16: 1885-1891
-
Mirovsky Y, Anekstein Y, Shalmon E, Peer A. Vacuum
Clefts of the Vertebral Bodies. Am. J. Neuroradiology 2005; 1:
26: 7: 1634 – 1640
-
McKiernan FE, Faciszewski , T. Intravertebral Clefts in
Osteoporotic Vertebral Compression Fractures . Arthritis &
Rheumatism 2003; 48: 5: 1414 – 1419
-
Baur A, Stabler A,
Arbogast S. Acute osteoportoic and neoplastic vertebral
compression fractures: Fluid sign at MR Imaging. Radiology 2002;
225: 3: 730-735
-
Naul LG, Peet GJ, Maupin WB. Avascular necrosis of the vertebral
body. Radiology 1989; 172: 219-222
-
Panow C, Valavanis A. A case of aseptic vertebral necrosis in
the context of metastatic lumbar disease. Neuroradiology 2002;
44: 249-252
|