|
Abstract
Over a period of 2 years
thirty-seven patients with dorso-lumbar spine injuries were
operated using the transpedicular approach. This approach
provides adequate cord decompression which was confirmed using
an endoscope. Fusion using iliac crest graft and stabilisation
with transpedicular screws and plates were done through the same
approach. Of the cases treated there was no mortality. One
patient had implant failure while two cases had infection of the
graft donor site.
Key
words: Thoraco-lumbar spine; transpedicular approach;
endoscope.
J.Orthopaedics 2007;4(2)e8
Introduction:
Thoraco-lumbar spine injuries can be operated
through a number of approaches. The posterior decompressive
laminectomy has fallen out of favour with reports now suggesting
that neurological deterioration could result following the
procedure1,2,3. The anterior approach allows for excellent
exposure of the vertebral body. However the procedure is
associated with significant post-operative morbidity and a
second procedure may be needed for posterior stabilization of
the spine4. The transpedicular approach allows for a single
stage vertebral body decompression, graft placement and
fixation. The procedure is cost effective and allows early
mobilisation of patients.
Material and Methods :
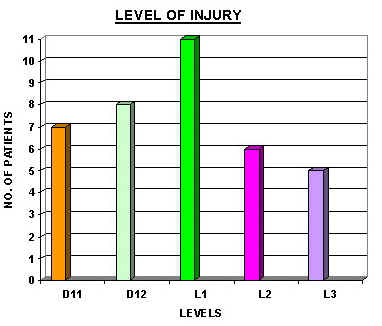
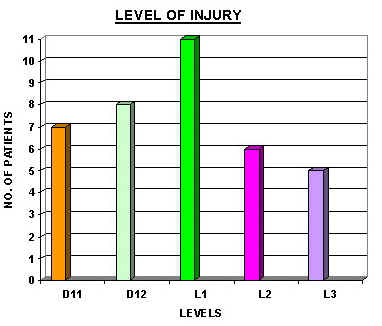
Thirty-seven patients with
thoraco-lumbar spine injuries involving D11 vertebrae and below
were operated via the transpedicular route over a period of two
years. Of these four were female and thirty-three were male. The
patientís age ranged from 17 to 62 years (average age 39
years).[FIGURE I]
Nine patients had no neurological deficit. Of the remaining,
twelve presented with paraplegia and sixteen with paraparesis.
Bladder and bowel involvement was noted in twenty-three patients
and twenty-six patients had diminished sensory perception.
Seventeen patients had associated orthopaedic injuries while
three had chest injuries and two patients had abdominal injuries
which necessitated surgical exploration.
All patients were
investigated with radiographs and CT scans. Eight patients with
no neurological deficit and three patients with neurological
deficit were noted to have no evidence of cord compression. In
the three who had neurological deficit the absence of cord
compression was confirmed with an MRI.
All eleven patients who had
no evidence of cord compression were stabilised using
transpedicular screws and plates5. All twenty-six patients who
had evidence of cord compression were subjected to
transpedicular decompression. A fibre optic nasal endoscope was
used to confirm adequate decompression on table6. In
twenty-three cases iliac crest grafts were used for fusion. All
twenty-six patients were stabilised using transpedicular screws
and plates.
Results :
All nine patients who
presented without neurological deficits remained neurologically
intact after surgery and could be mobilised on a thoraco-lumbar
brace.
Of the twelve patients who presented with complete
paraplegia, four patients improved enough to achieve
mobilisation with callipers and a single crutch. Six patients
were mobilised on callipers and two crutches using a swing
through gait. Two patients could not be mobilised on callipers
and remained wheel-chair bound on discharge.
Seven out of the sixteen
patients who presented with paraparesis improved sufficiently to
allow mobilisation on a thoraco-lumbar brace. Six patients could
be mobilised on callipers and a single crutch. Two patients were
mobilised on two crutches using swing through gait. One patient
could not be mobilised on callipers and was wheel-chair bound on
discharge.
The duration of hospital stay varied form fifteen to
sixty-three days (average twenty-eight days). There was no
mortality in this series of patients. One patient had an implant
failure which necesstated the removal of the implant. Two
patients developed infection at the donor graft site which
responded to antibiotics. Sixteen patients developed bedsores,
all of which could be managed conservatively.
|