|
Abstract:
Schwannoma,
also known as neurilemmoma, is a benign soft tissue tumour
arising from the schwann cells of the nerve sheath. Schwannomas
are usually solitary and encapsulated. Schwannomatosis is a
recently recognized third form of neurofibromatosis that causes
multiple schwannomas without vestibular tumors diagnostic of
neurofibromatosis type 2.
The authors are reporting a case of 33 year old male with
multiple histologically proven schwannomas without radiological
evidence of vestbular tumor and hence the diagnosis of
Schwannomatosis.
J.Orthopaedics 2007;4(2)e37
Case Report:
A 33 year old male presented with history of swelling of the
posteromedial aspect of left arm for the past three years. The
swelling was initially painless to start with later it became
painful. Pain was moderate in intensity with radiation to left
hand along the lateral three fingers in the median nerve
distribution. There was no history of hearing loss, giddiness or
decreased vision. There was no history of recent trauma, fever
or any constitutional symptoms. There was history of multiple
swellings in the neck region, which was operated thrice within
the past 13 years. The swellings were histologically proven to
be neurilemmoma. Investigations in the past Ė Contrast
enhanced CT Brain & Neck revealed no abnormality
intracranially and the swelling in the neck had features
suggestive of neurogenic tumor. Patient was not a diabetic nor
any history suggestive of any chronic medical illness.
|

|
|
Fig.1 MRI shows soft tissue
mass in the right carotid space |
There was a swelling on the posteromedial aspect of left arm
of about 2 cm in diameter globular in shape, nonpulsatile, skin
over the swelling was normal. On palpation, the swelling was
tender to deep palpation, with no local rise of temperature,
globular in shape, well defined, mobile in transverse direction
with limited mobility in vertical direction and the swelling was
nonreducible. There was tingling sensation in the median nerve
distribution area on tapping the swelling. Shoulder, elbow and
wrist movements were normal. There was no distal neurovascular
deficit.
Routine haematological investigations were within
normal limits, haemoglobin-14.2gm%, total leucocyte count-
7,200, differential count-neutrophils-54%, lymphocyte-36%,
monocyte-8%, eosinophil-2%, erythrocyte sedimentation rate- 22mm
in 1 st hour.
Magnetic
resonance imaging of the arm showed well defined densely
enhancing lesion measuring 18 x 17 mm noted in the left arm in
the medial compartment adjacent to the brachial artery and vein-
suggestive of schwannoma likely to be arising from the median
nerve.
|

|
|
Fig.2. Sagittal T2 MRI of left
arm showing Schwannoma |
Provisional
diagnosis of benign nerve sheath tumor was made. ( Schwannoma
was considered based on previous histopathology report). It was
decided to excise the mass. Intraoperatively the tumor was
arising from the median nerve and was eccentric. The mass was
not attached to the surrounding structures and was excised as a
whole by careful intraneural fascicular dissection without
damaging the nerve. Postoperatively there was minimal weakness
of the median nerve distribution. Three months follow-up showed
full recovery of the median nerve.
 |
 |
| Fig.3. Shows intraoperative picture
of the Schwannoma |
Fig.4. Shows excised tumor from the
median nerve |
Gross
findings of the tissue mass revealed single nodular tissue, pale
yellow in color measuring 3
x 1.5 x 1 cms. Outer surface is pale yellow covered by thin
membrane, areas of hemorrhage seen. Cut surface pale yellow
homogenous with specks of hemorrhage.
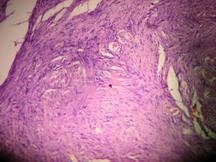
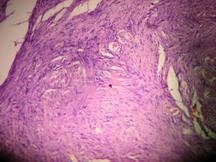
Histopathological examination revealed an encapsulated tumor
composed of spindle shaped cells arranged in fascicles with
regimentation. Antoni A and Antoni B areas are seen. The cells
are spindle shaped with elongated wavy nuclei, and abundant
fibrillar cytoplasm, nuclei are degenerative and bizarre.
|
|
| Fig.5. shows histopathology of
Schwannoma with Antoni Aand Antoni B areas |
Discussion :
Schwannoma
(neurilemmoma) is one of the few truly encapsulated neoplasms of
the human body and is almost always solitary. Itís most common
locations are the flexor surfaces of the extremities, neck,
mediastinum, posterior spinal roots, and cerebellopontine angle.
The nerve of origin often can be demonstrated in the periphery,
flattened along the capsule but not penetrating the substance of
the tumor. Since this is a benign neoplasm every attempt should
be made to preserve the nerve.
The Schwannoma (neurilemmoma) is the most common tumor of
the peripheral nerve, it accounts for 8% of all primary
intracranial tumors and 80-90% of those in the cerebellopontine
angle. The peak incidence is in the third to sixth decades, with
a slight female predominance. Intracranially there is a
predilection for sensory nerves especially the vestibular branch
of the eighth nerve. Rarely, schwannomas occur
intraparenchymally within the brain, cerebellum, or spinal cord:
in such rare instances, they presumably arise from schwann cells
that accompany blood vessels.
Most schwannomas are single sporadic benign lesions.
Bilateral vestibular schwannoma are the classic hallmark of
neurofibromatosis type 2 (NF2), which predisposes to multiple
schwannomas on cranial, spinal, and peripheral nerves and to
intracranial and intraspinal meningiomas and intramedullary
ependymomas. The term schwannomatosis or neurilemmomatosis has
been used to describe patients with multiple nonvestibular
schwannomas with no other signs of NF2.
The microscopic appearance is distinctive. Two different
patterns are recognized as Antoni A
and Antoni B areas. Antoni A areas are quite cellular and
composed of spindle cells often arranged in a pallisading
fashion or in an organoid arrangement (Verocay bodies). In type
B areas, the tumor cells are separated by abundant fluid that
may form cystic spaces.
Neurofibromas are distinct from schwannoma, these tumors
are not encapsulated and have a softer consistency than
schwannomas. In contrast to schwannomas, Verocay bodies,
palisading of nuclei and hyaline thickening of vessel wall are
almost always absent in neurofibromas.
Neurofibromatosis type I has features of multiple
neurofibromas with a genetically determined disorder. It is an
autosomal dominant disease; the responsible gene (NF1) is
located near the centromere of chromosome 17.
Neurofibromatosis type II is characterized by bilateral
vestibular schwannomas or in an individual who has first degree
family relative
with NF 2, is younger than 30 years of age, and presents
with unilateral vestibular schwannoma or two of the follow
ing: meningioma, glioma, schwannoma, juvenile posterior
subcapsular lenticular opacities and juvenile cortical
cataracts. It results from alteration of a gene located in
chromosome 22.
Schwannomatosis is a recently recognized third form of
neurofibromatosis in addition to NF1 & NF 2. The criteria for definite Schwannomatosis is two or more
pathologically sampled schwannomatosis and lack of radiographic
evidence of vestibular nerve tumor on an imaging study performed
after age 18 years. The criteria for presumptive schwannomatosis
is two or more pathologically sampled schwannomas without
symptoms of eighth nerve dysfunction at age more than 30 years
OR two or more pathologically sampled schwannomas in an
anatomically limited distribution without symptoms of eighth
nerve dysfunction at any age.
The proposed criteria for Schwannomatosis is age over 30
years and no evidence of vestibular tumor on high quality MRI
scan, no known constitutional NF2 mutation and two or more non-intradermal
(within or between layers of the skin) schwannomas, at least 1
with histologic confirmation Or One pathologically
confirmed non-vestibular schwannoma plus a first-degree relative
who meets above criteria.
The purpose of reporting this case is for the rarity of
presentation of multiple nonvestibular schwannomas without any
radiological evidence of intracranial tumor in a individual more
than 30 years old and hence the diagnosis of schwannomatosis.
The importance in the patients with multiple schwannomas is to
investigate radiologically for vestibular schwannomas and
careful dissection of the mass preserving the underlying nerve.
Reference :
-
MacCollin, M; Chiocca, E.A.; Evans, D.G.; Friedman, J.M.;
Horvitz, R.; Jaramillo, D.; Lev, M.; Mautner, V.F.; Niimura, M.;
Plotkin, S.R.; Sang, C.N.; Stemmer-Rechamimov, A.; Roach, E.S.
Diagnostic criteria for schwannomatosis. Neurology, 64,
1838-1845, 2005.
-
M.MacCollin; W.Woodfin; D.Kronn; and M.P.Short.
Schwannomatosis: A clinical and pathologic study. American Academy of Neurology 46:
1072-1079, 1996.
-
Matti Tapio Seppala, Markku Alarik Sainio, Matti Jouko
Johannes Haltia, JaakkoJyri Kinniunen, Kirsi Hannele Setala and
Juha Erik Jaaskelainen. Multiple schwannomas: schwannomatosis or
neurofibromatosis type 2?. J Neurosurg, 89, 36-41, 1998.
-
Douglas C. Antony, F.Stephen
Vogel. Pherpheral nervous system. Andersonís Pathology. Tenth
edition. Vol.2 page 2824-2826,
1996.
-
Kang KJ, Shin SJ, Kang ES. Schwannoma of the upper
extremity. Hand Surg Br. 25: 604-607, 2000.
-
Thomas R.Donner, Rand M. Voorhies, and David G. Kline.
Neural sheath tumors of major nerves. J Neurosurg, 81:362-373,
1994.
|