|
Abstract:
Much
research has been published on aspects of back pain adults,
however, there is comparatively little on the condition in
children. This has occurred despite the fact that back pain is a
common reason for presentation at the pediatric orthopedic
department. In children with back pain an organic cause is more
common than in adults. It is therefore important that orthopedic
surgeons are vigilant to the possible ‘serious’ organic
causes of back pain in children. This case report documents a
common presentation in our emergency department of a child with
back pain who has a non-specific history. The back pain is
subsequently found to be caused by a crush fracture occurring
secondary to acute lymphocytic leukemia. A discussion of the
biological causes of back pain in children follows.
Keywords: Spine; Pain; Paediatric; Leukemia
J.Orthopaedics 2007;4(2)e34
Case Report:
An
eight-year girl presented to the emergency department with acute
onset of midline lumbar back pain after minor trauma – a
soccer ball had hit her leg with "force" in the
playground. She had been transferred to hospital by
ambulance as she had been unable to stand initially. She
was reviewed by the orthopaedic registrar on call and a detailed
history revealed that the pain had been present intermittently
for two weeks. There were no specific aggravating movements,
however the pain was exacerbated by general activity and
sneezing. There were no radicular or systemic symptoms.
She gave a vague history of back injury 2 years prior.
On
examination loss of the lumbar lordosis was noted. There
was no tenderness to percussion, but axial compression
exacerbated the mid-lumbar pain. She had a normal straight
leg raise and normal neurological examination.
Plain
radiographs were performed and were thought to demonstrate
subtle loss of height of the L2 vertebral body.
Routine bloods were
normal, and the low back pain resolved in the emergency
department following the administration of oral ibuprofen. A
bone scan was organized with follow-up as an outpatient.
At
a follow-up appointment one week later the patient gave a
history of worsening pain.
Repeat examination revealed tenderness in midlumbar
region, exacerbated by percussion of the lumbar spine.
There were no gross motor, sensory or reflex changes.
Full blood count, electrolytes, erythrocyte sedimentation rate,
and C-reactive protein were once again within normal ranges. The
working diagnosis at this stage was infection or eosinophilic
granuloma.
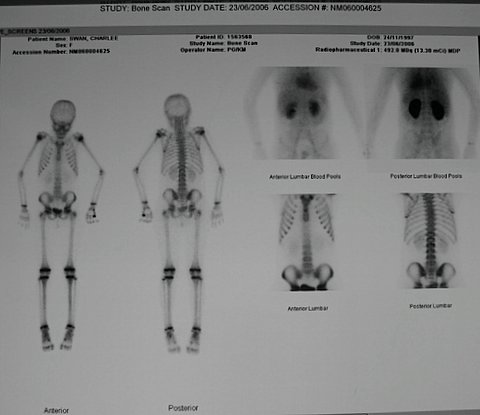
Bone
scan was performed and a subtle abnormality in the superior
aspect of L2 was reported. There was no abnormal blood pool
activity or extension across the disc space. It was concluded
that a diagnosis of discitis was unlikely. Repeat bloods two
weeks after initial presentation were again normal. A renal ultrasound was performed to exclude a renal
cause. An MRI scan
demonstrated an infiltrative process involving several levels at
the lumbar spine. The oncology team was involved and the diagnosis of ALL was
confirmed with bone marrow biopsy.
On retrospective review of initial plain radiographs, it
was agreed that there was osteopenia and pathological fracture
of the superior end plate of L2, consistent with the diagnosis
of an infiltrative process.
Discussion :
The incidence and prevalence of back pain amongst the paediatric
population is not as established as that in adults. A
review of the literature1 found lifetime prevalence rates to
vary between 7-63% in children and adolescents. In the adult
population true bony pathology, aside from degeneration, is
rare. Significantly, in the paediatric population, an acute
organic cause is common2. The differential diagnosis of back
pain in children is included in table 2.
Although occult malignancy is a rare cause of organic back pain
in children, it should form part of the differential diagnosis
of children presenting with musculoskeletal complaints. Atypical
features inconsistent with the provisional orthopaedic diagnosis
should alert the clinician to consider an alternative diagnosis.
Atypical features of a patient’s pain are often known as
‘red flag’ symptoms (see table 3). History taking can be
challenging in trying to establish an adequate pain description
from child. Because of this it is easy to neglect the need to
check for ‘red flag’ symptoms suggestive of serious
pathology. It is essential that children and their parents are
questioned about these symptoms to avoid delays in diagnosis of
a serious condition.
In
a child with red flag symptoms the differential diagnosis would
include.
·
Juvenile rheumatoid arthritis
·
Septic arthritis
·
Osteomyelitis
·
Discitis
·
Acute lymphoblastic leukaemia (ALL)
·
Hodgkin’s lymphoma
·
Langerhans cell histiocytosis
·
Tuberculosis of the spine
·
Seronegative spondyloarthritis
In
our case the patient’s back pain was caused by ALL. Acute
leukaemia is the most frequent malignant childhood disease with
a peak frequency at two to five years of age. 75% of cases are
lymphocytic in origin (ALL as in our case), 15-20% are
myelogenous leukaemias, and 5-10% are of the non-lymphocytic
type.
Patients
may present with ALL in a variety of ways. Symptoms are usually
related to infiltration of leukaemic cells into the bone marrow
leading to suppression of normal marrow activity. Presenting
symptoms are manifestations of the underlying anemia,
thrombocytopenia, and neutropaenia, and may include fever,
pallor, lethargy, and bruising. Bone pain, particularly
affecting the long bones, is considered to be the result of the
massive proliferation of haemopoietic tissue within the
medullary cavity or periosteum.
In
our case, the only clinical feature was musculoskeletal pain due
to acute pathological fracture.
Bone
pain is not an uncommon initial presentation of leukaemia. In a
study5 of 295 children diagnosed with ALL or malignant lymphoma,
7.1% initially presented to the orthopaedic department with bone
pain. Among these patients 25% specifically had spinal pain. Of
concern Jonsson et al6 reported that patient who listed bone
pain, limp, or other musculoskeletal symptoms as their chief
complaint received a significant delay in diagnosis of acute
leukaemia compared with those that had no musculoskeletal
symptoms.
Routine
blood tests, including inflammatory markers such as ESR and CRP,
are not very useful in categorically excluding malignancy in the
paediatric population. In the study by Kobayashi et al5 it
was noted that the majority of patients with ALL presented with
mostly normal full blood counts. In their laboratory data CRP
was the most sensitive indicator at initial presentation. It was
suggested an elevated CRP without leukocytosis may be an
important finding in patients with leukaemia who complain of
musculoskeletal conditions at initial presentation.
A
significant and encouraging finding in a recent multicenter case
control study by Jones et al7 concluded that in children
presenting with musculoskeletal complaints, the three most
important factors that predicted a diagnosis of ALL were low WCC,
low-normal platelet count, and a history of night-time pain. In
the presence of all 3 of these findings the sensitivity and
specificity for the diagnosis of ALL were 100% and 85%
respectively.
It
is imperative to investigate sites of bony pain and tenderness
with an imaging technique. Gray8 recommends that every child
that presents with back pain that cannot confidently be
classified as innocent should have, at least, standing
anterior-posterior and lateral radiographs of the spine.
Findings on pain x-ray suggestive of malignancy are listed in
Table 4. Kobayashi et al5 found that 94% of patients with
ALL had a radiographic abnormality at presentation, the most
common of which was osteopaenia at the symptomatic area. In
contrast Cabral and Tucker9 found that plain x-ray films
provided diagnostic information in only a quarter of patients.
Importantly, however, they noted that nearly two thirds of
either plain x-rays or bone scans, which were initially reported
as normal before the rheumatology consultation, were then found
to have abnormalities on careful re-examination by a paediatric
radiologist.
In conclusion,
musculoskeletal pain is a common presentation of paediatric
malignancy. As discussed above the results of routine
investigations are often non-specific. Therefore, if there is an
index of clinical suspicion one should have a low threshold for
specialist referral, as MRI scanning, peripheral blood smear and
bone marrow biopsy may need to be undertaken.
Reference :
-
Kovacs F, Gestoso M, del Real M, Lopez J, Mufraggi N, Mendez J .
Risk factors for low back pain in schoolchildren and their
parents: a population based study. Pain. 2003;103:259-268.
-
Weinstein J, Boriani S, Campanacci L. Spine neoplasms. In: Weinstein S (ed). The Pediatric Spine: Principles and
Practice. 2nd ed. Philadelphia, PA: Lippincott, Williams, &
Wilkins;2001:685-707.
-
Sumeet G, Dormans J. Tumours and Tumour-like Conditions of the
Spine in Children. Journal of the American Academy of Orthopedic
Surgeons. 2005;13:372-381.
-
Waddell G. The back pain revolution. Edinburgh: Churchill
Livingston; 1998
-
Kobayashi D, Satsuma S, Kamegaya M, Haga N, Shimomura S, Fujii
T, Yoshiya S. Musculoskeletal Conditions of Acute Leukemia and Malignant
Lymphoma in Children. Journal of Pediatric Orthopedics B.
2005;14:156-161.
-
Jonsson OG, Sartain P, Ducore J, Buchanan G. Bone pain as an
initial symptom of childhood acute lymphoblastic leukaemia:
Association with nearly normal hematologic indexes. Journal of
Pediatrics. 1990;117:233-237.
-
Jones
O, Spencer C, Bowyer S, Dent P, Gottlieb B, Rabinovich C. A
Multicenter Case-Control Study on Predictive Factors
Distinguishing Childhood Leukaemia From Juvenile Rheumatoid
Arthritis. Pediatrics. 2006;117:e840-844.
-
Gray A. Back pain in children and adolescents. Medicine Today.
2005;6:27-33.
-
Cabral D, Tucker L. Malignancies in children who initially
present with rheumatic complaints. Journal of Pediatrics.
1999;134:53-57.
|