|
Abstract:
We
report a case of a 59 year-old female patient, who has a history
of restrictive pericarditis, presented as cough, high fever and
dyspnea at admission. Eight days after admission, she complained
of right buttock pain. Diagnosis of tuberculous sacroiliitis was
made by CT-guide aspiration for histology and culture. After
administration of antitubercular agents, symptoms improved
dramatically and the patient discharged. In this case, CT-guide
aspiration plays an important role in patients with atypical presenting symptoms with minimal
intervention. Active tuberculosis was also proved three month
later by acid-fast stain of sputum.
Keywords:
Tuberculosis, sacroiliitis
J.Orthopaedics 2007;4(2)e29
Case report:
A
59 year-old female had medical history of pericardial tumor post
operation, constrictive pericarditis, atrial fibrillation and
congestive liver cirrhosis. Anti-tuberculosis drugs history was
also related. She had been experiencing coughing with yellowish
sputum for 3 weeks. Fever (38.8oC), chills, dyspnea and chest
tightness were also present for several days. Laboratory data
showed progressive inflammation (C-reactive protein 25.64à53.73μg/ml).
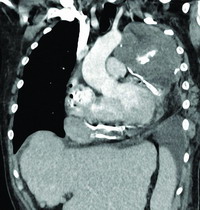
Chest X-ray showed consolidation of the left lung. Chest CT
showed constrictive heart failure and pericardial effusion with
calcifications (Fig 1). She was treated under the impression of
pneumonia. However, fever didnt subside.
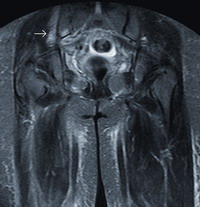
Right
buttock pain was complained at the 8th day after admission. The
plain film revealed widening of right sacroiliac (S-I) joint and
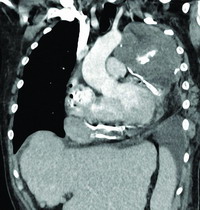
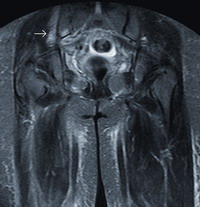
haziness of the subchondral bone (Fig 2). MRI was arranged and
showed edematous change of right iliac bone adjacent to the
right S-I joint (Fig 3).
 |
 |
| Fig 1.Reformatted coronal image of
chest CT revealed constrictive pericarditis with
pericardial effusion and calcifications |
Fig 2.Radiograph of right hip joint
showing mild widening and haziness (arrow) at lower
portion of right sacroiliac joint |
|
|

|
|
Fig 3a.Coronal T2-seighted images
of pelvis showing hyperintensities, representing bone
marrow edema.
Post enhanced T1-weighted coronal |
Fig 3b.showing heterogeneous
enhancement (arrow)
|
Due
to no significant abscess formation being identified in the MRI
study, Ga-67 whole body scan was performed for infectious source
detection and revealed mild active gallium-avid lesions in the
right S-I joint.
With
clinical correlation, CT-guided aspiration was performed for
right S-I joint and a small amount of turbid fluid was
aspirated. Histology showed PMN, lymphocytes and histiocytes.
Smear of the fluid showed no acid-fast bacilli. However, growth
of bacilli in Lowenstein-Jensen established the diagnosis of
tuberculosis sacroiliitis.
Fever,
chills, cough, dyspnea and chest tightness were relieved after
administration of anti-tuberculosis agents. Follow-up CRP was
also decreased in level (53.73à14.65μg/ml). The
patient was discharged with some complications caused by
anti-tuberculosis agents (dizziness, anorexia, GI upset,
elevated GOT/GPT) and general condition was stable.
Discussion :
Tuberculosis
is the most common infectious disease in the world, especially
in South-East Asia [2]. According to World
Health Organization (WHO), the
prevalence of tuberculosis globally is about 0.23% [2].
Extra-pulmonary tuberculosis accounts for 1530% of cases [4-5]. In
all tuberculosis cases, bone and joint involvement account for
about 1~5% [1]. In
bone invasion, about half involve the spine, mainly the
thoracolumbar junction.
The S-I joint is rarely involved, in only 3~9.7% of these
cases. Tuberculous
in S-I joint is frequently missed because of the vague symptoms
and poor localizing signs [3]. Therefore, increased vigilance is
required for diagnosis.
Difficult walking, buttock pain, nerve root pain in the
lower limbs [7], and low back pain may occur as onset
symptoms in sacroiliac tuberculosis. It is difficult to diagnose
due to the vague and non-specific presentations. Thus, the mean
time from symptom onset to diagnosis is 5.5 months in the
literature [8]. In our case, fever, cough and dyspnea without buttock pain were present at first. Misdiagnosis
of pneumonia was made according to symptoms, laboratory data and
chest X-ray. Finally, buttock pain was complained about after
eight days and X-ray for right hip was performed.
In the earliest stage of sacroiliac tuberculosis, X-ray
may not show any abnormalities. Mild haziness and widening of
the S-I joint, especially in the lower part, can be the earliest
changes followed by bone erosion. In a subacute or indolent
case, sclerotic change of subchondral bone is common in later
stages [9]. Bone scan is helpful for early detection of the
lesion with increase uptake [10]. CT shows more delicate anatomy
than X-ray, and MRI provides differential diagnosis between soft
tissue tumor and pyogenic arthritis [11].
In our case, subtle changes such
as haziness at lower portion of right S-I joint were noted. Non-specific edema with minimal fluid accumulation
adjacent to right S-I joint also made diagnosis difficult.
Nevertheless, buttock pain and history anti-tuberculosis agents
were the key points to aim our direction of diagnosis to
tuberculosis sacroiliitis. CT-guide aspiration provides a method
with minimal invasive for diagnosis.
Tuberculosis in S-I joint is often associated
with tuberculous lesions elsewhere, and it commonly originates
from a tuberculous psoas muscle abscess or tuberculous
spondylitis [6], which was not shown in our case. However,
tuberculous pericarditis, though not proved, was suspected as
the site of primary origin.
The CA125 level of our patient has been
persistently high (>500 U/ml, normal range<35U/ml) for
several years. However, there was no evidence of gynecologic
malignancy after general survey by pelvic CT. Yilmaz
reported that CA 125 is beneficial in the determination of
tuberculosis activity and in differentiation between active and
inactive pulmonary tuberculosis [12]. In our case, active
tuberculosis was proved three months later by acid-fast stain of
sputum, though it was negative at admission.
Except for the
high CA125 level, history of constrictive pericarditis was also
present in our patient. No direct evidence of tuberculous
pericarditis was present after biopsy. However, inspissated
fragments, debris and blood clots, indicating a chronic
inflammatory process of the pericardium. Furthermore, in the
report of Nakanishi Y, significant elevation of serum
CA125 was noted in patients with tuberculous pleurisy [13]. It
also offered an indirect evidence of tuberculous pericarditis in
our case.
Conclusion:
Though tuberculous
sacroiliitis is hard to diagnose due to vague
symptoms and poor localizing signs. In patients that with
atypical presenting symptoms, images, such as MRI, and CT-guide
aspiration biopsy are good diagnostic method with minimal
intervention. It is also important to survey the tuberculous lesions elsewhere.
Reference :
-
Davies
PD, Humphries MJ, Byfield SP, Nunn AJ, Darbyshire JH, Citron
KM, Fox W: Bone and joint tuberculosis. A survey of
notifications in England and Wales. J Bone Joint Surg Br
1984;66(3):326330
-
Http://www.who.int/mediacentre/factsheets/fs104/en/#global
-
Gordan
G, Kabins SA: Pyogenic sacroiliitis. Am J Med 1980;
69:5056
-
Hopewell
PC: A clinical view of tuberculosis. Imaging of tuberculosis
and craniospinal tuberculosis. Radiol Clin North Am
1995;33:64153.
-
Sharif
HS, Morgan JL,AI Shahed MS,AI ThagafiMY: Role of CT and MR
imaging in the management of tuberculous spondylitis. Radiol Clin
North Am 1995;33:787804.
-
Kim
NH, Lee HM, Yoo JD, Suh JS: Sacroiliac joint tuberculosis.
Classification and treatment.Clin Orthop 1999;358:215222
-
Chen
WS: Chronic sciatica caused by tuberculous sacroiliitis. A
case report. Spine 1995;20:11946.
-
Gonzalez-Gay
MA, Garcia-Porrua C, Cereijo MJ, Rivas MJ, Ibanez D, Mayo J:
The clinical spectrum of osteoarticular tuberculosis in
non-human immunodeficiency virus patients in a defined area
of northwestern Spain. Clin Exp Rheumatol 1999;17:663669.
-
Delbarre
F, Rondier J, Delrieu F, Evrard J, Coyla J, Menkes J, et al:
Pyogenic infection of the sacroiliac joint. J Bone Joint Surg 1975;57:819.
-
Salomon
CG, Ali A, Fordham EW: Bone scintigraphy in tuberculous
sacroiliitis Clin Nucl Med 1986; 11(6):407408
-
Hong
SH, Kim SM, Ahn JM, Chung HW, Shin MJ, Kang HS: Tuberculous
versus pyogenic arthritis: MR imaging evaluation. Radiology
2001; 218(3):848853
-
Yilmaz
A, Ece F, Bayramgurler B, Akkaya E, Baran R., Int J Tuberc
Lung Dis. 2002
-
13.
Nakanishi Y, Hiura K, Katoh O, Yamaguchi T, Kuroki S, Aoki
Y, Yamada H: Clinical significance of serum CA125 in
patients with tuberculous pleurisy. Kekkaku. 1991
Aug;66(8):525-30.
|