|
Abstract:
Introduction:Bilateral
septic arthritis of the hip is not very common clinical problem
as compared to unilateral septic arthritis of the hip. Diagnosis
is difficult and if not treated in time may lead to permanent
damage to the joint. Salvage procedures are technically
difficult and dose not yield good results.
Case Report:A patient with bilateral hip joint septic
arthritis secondary to olecrenon bursitis is presented. He was
managed in ITU because of his sepsis and septic arthritis was
treated with antibiotics and joint washouts.
Conclusion:Outcome from septic hip arthritis can be
improved if the condition is diagnosed early and treated
appropriately. Delay in treatment is associated with poor
outcome
Key
Words: Hip, Septic, Arthritis, Bilateral.
J.Orthopaedics 2007;4(2)e14
Introduction:
Unlike
septic arthritis of the knee, sepsis in the hip is much more
difficult to diagnose. High index of suspicion, with clinical
findings of hip pain and reduced movements, help in the early
diagnosis. Raised inflammatory markers help to confirm the
diagnosis. X-rays in the early stage may not show any changes.
Early diagnosis is essential to prevent long-term sequelae and
to improve the outcome especially in children1 and young adults.
Good outcomes are associated if sepsis in the hip is drained
surgically within 4 days of onset of symptoms in children.
Presence of osteoarthritis of the hip complicates the picture
thus causing delay in diagnosis. Knight et al suggested that
septic arthritis should be considered in any patient with acute
exacerbation of pain in an osteoarthritic joint, particularly if
there is a possibility of coexisting infection elsewhere in the
body2.
Bilateral hip
septic arthritis is a rare entity and to date only one case has
been reported associated with radiotherapy of the hip. We
present a case of bilateral septic arthritis of hip in an
immunocompromised patient.
Case report:
58
year old gentlemen presented to A&E with few hours’
history of sever right anterior thigh pain, radiating to his
toes. He was unable to weight bear on his right leg. There was
no history of any acute trauma to his right leg. He also
complaint of feeling of being unwell for a day. He had a
background history of type II diabetes mellitus controlled with
glicalzide, asthma controlled with steroid inhalers and
bilateral osteoarthritis of hips left worst than the right. He
was already on a waiting list for a left total hip replacement.
He had a very recent history of right olecrenon bursitis and was
on oral flucloxacillin.
Clinical
examination revealed sinus tachycardia with a heart rate of 130
beats/min, low blood pressure of 80/60 mm of Hg and a
temperature of 38.3. He was maintaining his saturation at 99%
with 2 L of oxygen. Systemic examination was unremarkable except
moderate abdominal distention. He was unable to move his right
leg therefore right hip movements were difficult to access.
His
inflammatory markers were raised with C-reactive protein of 36
and a while cell count of 16.9. He also had deranged renal
functions test with raised urea and creatinine on admission. He
was put on intravenous flucloxacillin and ceftriaxone.
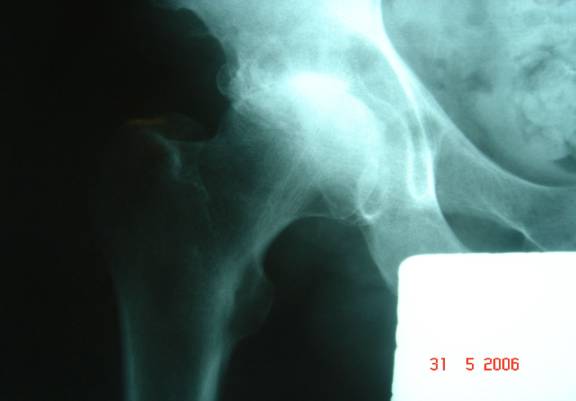
X-ray
of his both hips and right femur did not show any acute bone
trauma but there were osteoarthritic changes in his right hip
with avascular necrosis of left head of femur [Fig 1,2].
Initially he was admitted under medical care without any
definitive diagnosis. Orthopaedic review was arranged the same
day and on examination by the orthopods the possibility of
septic arthritis right hip could not be ruled out. Right hip
aspiration was done and specimens were sent for cultures and
gram staining. Clindamycine was added to his antibiotics upon
discussion with the microbiologist.
|
|
In
the mean time he developed septic shock and was shifted to ITU
for intensive monitoring and management. He was put on
ionotropes and hydrocortisone in the ITU to maintain his blood
pressure. Because of progressive septic shock a decision was
made to washout his right hip joint, which was carried out
through posterior approach to the hip. Further specimens were
sent for culture and gram staining from the hip. He subsequently
grew group B streptococci from his blood and cultures, hip and
wound swab from the olecrenon bursa and therefore was commenced
on benzylpenicilline.
Despite
the right hip washout, his blood pressure did not pick up and he
started becoming increasingly acidotic with increased lactate,
decreased PCO2 and decreased bicarbonate. On examining him again
his left hip movements were restricted and painful this time
with satisfactory right hip wound and slightly increased
movements in right hip. A diagnosis of septic arthritis of left
hip was made this time and left hip was washout was arranged.
Hip was approached through posterior approach. Left hip joint
was found to be totally destroyed with avascular necrosis.
Deformed femoral head was removed, specimens were sent for
culture and gram staining and hip was washed out with saline.
The culture from left hip also grew group B streptococci.
Postoperatively
his acidosis started improving and his renal functions became
normal. He was finally weaned off from ionotropes on second
postoperative day. Within a week he was out of ITU and started
mobilising.
All
the three strains of streptococci isolated from olecrenon bursa
and both hips were subjected to PCR series and gene probing
which showed that all three isolates were indistinguishable from
one another. This essentially means that all the three isolates
were similar and bilateral hip sepsis was secondary to
streptococcus group B infection within the olecrenon bursa.
Discussion And Review of Literature:
Septic
arthritis is inflammation of a synovial membrane with purulent
effusion into the joint capsule, usually due to bacterial
infection. Incidence of septic arthritis is 2 to 10 per 100,000
of general population [3]. Septic arthritis used to be a life
threatening condition prior to antibiotic era. Although the
mortality has certainly decreased with antibiotics but the
morbidity is still very high. Residual damage to the articular
cartilage of the involved joint leads to long-term consequences
such as osteoarthritis. 25 to 50% will develop irreversible
joint destruction [4]. Septic arthritis of the hip can occur at
any age group, including infants and children. Certain risk
factors causes increased incidence of this potentially fatal
problem. These include chronic rheumatoid arthritis, systemic
infections, certain types of cancer, diabetes mellitus, sickle
cell anemia, systemic lupus erythematosus (SLE),
haemochromatosis, intravenous drug abusers, alcoholics, and
after prosthetic joint replacements. Recent history of joint
injury, surgery or patients receiving medications is also on a
predisposing factor for septic arthritis. Women and male
homosexuals are at greater risk for septic arthritis than are
male heterosexuals.
The
pathophysiology of septic arthritis of the hip is essentially
the same as for any other joint. Bacteria usually gain access to
the hip joint either through the blood or a break in the skin.
Direct injury to the joint resulting in haematoma formation can
predispose to infection. Spread of infection can also occur from
an adjacent osteomyelitis or soft tissue infection. Once
bacteria cross the synovial membrane they trigger an
inflammatory reaction that is manifested by the presence of
plasma proteins and polymorhonuclear cells within the joint,
producing an effusion. This stage is still reversible if treated
because of intact articular cartilage. However if left
untreated, proteolytic enzymes initiate articular cartilage
destruction and permanent joint damage.
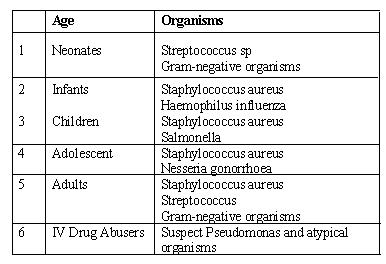
The
pattern of particular bacterium causing the infection varies
considerably with the age of the patient [Table 1]. In all age
groups staphylococcus aureus and streptococcus is the most
common organism causing septic arthritis of the hip [5]. In
neonates’ staph aureus, streptococcus and gram-negative
anaerobes are responsible for majority of the infections. Staph
aureus and Haemophilus influenzae are the main infecting
organisms in infants. In children staph aureus along with
salmonella become the most important organisms causing septic
arthritis. Nesseria gonorrhoeae should always be suspected in
younger adults and teen age.
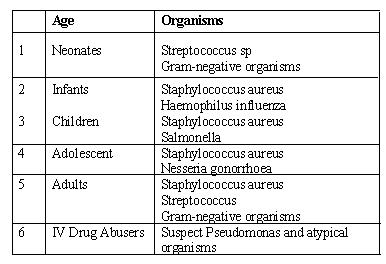
Table
1: Common bacteria causing septic arthritis in different age
groups
In
the early stage of progression, it is very difficult clinically
to diagnose septic arthritis of the hip. The diagnosis however
becomes clearer in more advance stage when joint effusion is
detected clinically. Diagnostic clinical clues include fever,
red, hot, swollen hip joint with marked groin tenderness and
decreased active and passive range of movements. Infants and
children present diagnostic challenge, as the diagnostic signs
of joint infections may not be obvious clinically. There may be
no fever and symptoms like anorexia, nausea, vomiting, decreased
appetite, abdominal distention and irritability may easily
confuse the clinician and lead to incorrect diagnosis. In
infants, the affected limb is usually flexed, abducted and
externally rotated at the hip in order to relieve the pressure
on the capsule. A search should be made clinically to exclude
distant infections in children.
Full
blood count shows increased leucocyte count and erythrocyte
sedimentation rate. C-reactive protein is also diagnostic and
serial measurement will help to monitor the course of treatment.
Blood cultures are positive in only half of the patients with
staph aureus infections. Anteroposterior and lateral plain
radiographs of the hip are often normal in early stages. A
periosteal reaction usually becomes visible at about 10 days and
is a non-specific sign of infection. Ultrasound examination is
sensitive in detecting joint effusion and therefore
differentiates septic arthritis from other conditions such as
soft tissue abscess and tenosynovitis. It also helps to guide
joint aspiration. Gordon et al reported a 5% false negative rate
of ultrasound in diagnosing septic arthritis of the hip [6].
Isotope bone scanning can diagnose acute joint infections with
significant accuracy. Technetium-99m labeled phosphate compound
has accuracy in excess of 80% [7]. Because the diagnosis is
clinical in cases of hip joint, therefore it is not necessary to
request an isotope scan in every patient. It can however be done
in cases where the diagnosis is not clear and patient is
clinically not unwell.
Aspirating
the joint and culturing the aspirate achieve definitive
diagnosis. Immediate gram stain can identify the organisms even
before the results of cultures are known and guide the nature of
antibiotic therapy. Aspiration is done under local anaesthetics
and with the help of image intensifier. The advantages of joint
aspiration are that it may be the diagnostic and therapeutic
procedure in majority of the patient. Joint decompression may
help to relieve the pain and increase range of joint movements.
Antibiotics
should be withheld until the joint has been aspirated and
specimens have been sent for culture and gram staining. Gram
staining can direct the use of appropriate antibiotics,
otherwise antibiotics on best guess basis or according to local
hospital policy can be started. About 2 decades ago clinicians
advocated the use of antibiotics and repeated aspirations for
the treatment of septic arthritis [8].
However treatment of choice in septic arthritis of the
hip now is arthrotomy, drainage of pus and lavage. Other
techniques of draining the hip has been described in literature
but are not very popularly used. Repeated closed suction and
drainage of the joint has been advocated by some authors but
with associated increased incidence of complications [9].
Arthroscopic drainage of the hip has the advantage of a very
small scar and early mobilization but it is technically very
demanding, doses not achieve complete drainage and is time
consuming [10].
The
prognosis of septic arthritis of the hip depends upon the
urgency with which definitive treatment is started. A poor
outcome is associated with infancy, delay in treatment of
greater than 4 days and proximal femoral osteomyelitis.
Conclusion:
Septic arthritis of hip is an orthopaedic
emergency with good potential of cure if diagnosed and treated
early. Delay in treatment adversely affects the outcome and
results in permanent joint destruction. Arthrotomy, drainage and
lavage of the affected joint remain the gold standard treatment
for septic arthritis of the hip. Reconstructive surgery in
infants and children after acute septic arthritis is difficult
and associated with increased morbidity. Total hip replacement
is the treatment of choice in older patients after septic
arthritis of hip.
References :
-
Bennett OM, Namyak SS: Acute septic arthritis of the hip
joint in infancy and childhood. Clin Orthop 281:123-132, 1992.
-
Knight J, Gilbert FJ, Hutchison JD, Lesson of the Week:
Septic arthritis in osteoarthritic hips. BMJ 1996; 313:40-41
-
Kaandorp CJE, Van Schaardenburg, Krijnen P, Habbema JDF,
van de Laae MAFJ. Risk factors for septic arthritis in patients
with joint disease: a prospective study. Arthritis Rheum 1995;
38: 1819-1825.
-
Goldenberg DL, Reed JI. Bacterial arthritis N Engl J Med
1985; 312: 764-771.
-
Chen CE, Ko JY, Li CC, Wang CJ. Acute septic arthritis of
the hip in children. Arch Ortop trauma Surg 2001; 121: 521-526.
-
Gordon EJ, Huang M, Dobbs M, Luhmann SJ, Szymanski DA,
Schoenecker PL. Causes of false-negative ultrasound scans in the
diagnosis of septic arthritis of the hip in children. J Pediatr
Orthop 2002; 22:312-316.
-
Goldschmidt RB, Hoffman EB. Osteomyelitis and septic
arthritis in children. Current Orthopaedics 1991; 5:248-255.
-
Wilson N I L, Di Paola M. Acute septic arthritis in
infancy and childhood. J Bone Joint Surg 1986; 68-B: 584587.
-
Letts R M, Wong E. Treatment of acute osteomyelitis in
children by closed-tube irrigation: a reassessment. Can J Surg
1975; 18:60-63
-
Chung WK, Slater G L, Bates WH.
Treatment of septic arthritis of the hip by arthroscopic lavage. J Pediatr
Orthop 1993; 13: 444--446.
|