Abstract:
Purpose: To assess the feasibility, effectiveness and safety of a 2-portal arthroscopic subacromial decompression (ASD) technique for chronic impingement syndrome. This technique uses only the anterior and posterior arthroscopic portals and does away with the lateral subacromial portal
Methods: We performed a retrospective cohort study on patients with chronic impingement syndrome (Neers stage 1 and 2) who had failed at least 6 months of conservative management which included rest, oral non-steroidal anti-inflammatory medication, physiotherapy and subacromial steroid injections. These patients underwent a 2-portal ASD procedure and were followed up at least 2 years after surgery. We compared patients’ pre-operative and post-operative UCLA and Simple Shoulder Scores and assessed patients’ satisfaction with their surgery.
Results: Mean simple shoulder scores improved from 5.15 (pre-operative) to 10.9 (post-operative) (112% improvement) (p<0.001), Mean UCLA shoulder rating score improved from 15.9((pre-operative) to 31.5 (post-operative) (98% improvement)(p<0.001). Surgery was rated as excellent in 60% of patients and good in 25%. There were no complications encountered and overall 96.8% of patients were satisfied with their surgery.
Conclusions: This study has shown the 2-portal ASD technique to be feasible, effective and safe for patients with Neers 1 and 2 chronic shoulder impingement syndromes.
J.Orthopaedics 2012;9(4)e2
Keywords:
arthroscopic subacromial decompression, 2-portal technique
Introduction :
Subacromial impingement occurs as a result of chronic repetitive microtrauma of the rotator cuff and subacromial bursa as the shoulder is abducted. The supraspinatus tendon passes through the narrow space called the supraspinatus outlet before inserting into the humeral greater tuberosity. In 1972, Neer introduced the term ‘impingement syndrome’ which described the repetitive trauma to the supraspinatus tendon as it passes beneath the coracoacromial ligament and the anterior one third of the acromion1. He described three stages in rotator cuff impingement: Stage 1 commonly affected patients younger than 25 years old and is depicted by acute inflammation, oedema, and haemorrhage in the rotator cuff. This stage usually is reversible with non-operative treatment. Stage 2 usually affe
cts patients aged 25 to 40 years old and is characterised by fibrosis and tendonitis which commonly requires surgical intervention. Stage 3 typically affects patients older than 40 years old and often leads to mechanical disruption of the rotator cuff tendon and changes in the coracoacromial arch with osteophytosis along the anterior aspect of the acromion. Non-outlet impingement may also occur due to thickening of the subacromial bursa and rotator cuff tendons.
Impingement syndrome commonly causes chronic shoulder pain and weakness, particularly in the lateral, superior and anterior aspects and is typically worsened by overhead activities.
Arthroscopic subacromial decompression (ASD) is a surgical technique pioneered by Ellman in 1985 aimed at relieving any compression or irritation on the rotator cuff by removing subacromial bony spurs and all soft tissue irregularities such as bursitis or synovitis2.
This increases the size of the subacromial area which helps prevent impingement on the supraspinatus tendon. ASD involves debriding inflamed bursa and synovitis, cutting through the coracoacromial ligament and shaving away subacromial bone spurs to enable the supraspinatus muscle to abduct the shoulder without any impingement. ASD has been shown to produce good results which are comparable to those of open decompression surgery3,4,5.
Aim
The aim of this study is to assess the feasibility, effectiveness and safety of a 2-portal ASD technique, doing away with the lateral arthroscopic portal. We hypothesise that the 2- portal ASD technique will produce results comparable to those of the 3-portal ASD technique.
Materials and methods:
We performed a retrospective study on patients with chronic impingement syndrome (Neer stage 1 and 2) who had surgery between 2006 and 2009. All patients had positive impingement signs, unimproved pain after a course of conservative treatment comprising rest, non-steroidal anti-inflammatory medications, physiotherapy and subacromial steroid injections. All patients were assessed pre-operatively using the University of California-Los Angeles (UCLA) Shoulder Rating Scale (Table 1) and Simple Shoulder Test (Table 2).
All patients underwent the 2-portal ASD surgery performed by a single surgeon. We repeated the UCLA shoulder rating scale and the simple shoulder test about 2 years after surgery, assessing their level of function, range of motion and strength. We also assessed our patients’ general satisfaction with the surgery. Patients excluded from our study were those who had concurrent ASD with rotator cuff debridement or repair and those who underwent arthroscopic repair of labral tears.
The pre-operative and post-operative Simple Shoulder and UCLA shoulder scores were analysed via the paired-T test to determine the significance of improvement using the Statistical Package for the Social Sciences (SPSS) software (version 17; SPSS, Inc., Chicago, IL).
Table 1: UCLA Shoulder Rating Scale (Max score 35, ³ 27 = good, < 27 = poor) |
Pain |
Active Forward Flexion |
|
|
Points |
|
|
Points |
1 |
Present all the time and unbearable; strong medication frequently |
1 |
1 |
150 degrees or more |
5 |
2 |
Present all of the time but bearable; strong medication occasionally |
2 |
2 |
120 to 150 degrees |
4 |
3 |
None or little at rest, present during light activities; salicylates frequently |
4 |
3 |
90 to 120 degrees |
3 |
4 |
Present during heavy or particular activities only, salicylates occasionally |
6 |
4 |
45 to 90 degrees |
2 |
5 |
Occasional and slight |
8 |
5 |
30 to 45 degrees |
1 |
6 |
None |
10 |
6 |
< 30 degrees |
0 |
Function |
Strength of Forward Flexion (manual muscle testing) |
|
|
Points |
|
|
Points |
1 |
Unable to use limb |
1 |
1 |
Grade 5 (normal) |
5 |
2 |
Only light activities possible |
2 |
2 |
Grade 4 (good) |
4 |
3 |
Able to do light housework or most activities of daily living |
4 |
3 |
Grade 3 (fair) |
3 |
4 |
Most housework, shopping and driving possible; able to do hair and dress and undress, including fastening brassiere |
6 |
4 |
Grade 2 (poor) |
2 |
5 |
Slight restriction only; able to work above shoulder level |
8 |
5 |
Grade 1 (muscle contraction) |
1 |
6 |
Normal activities |
10 |
6 |
Grade 0 (nothing) |
0 |
Patient Satisfaction |
|
|
|
Points |
1 |
Satisfied and better |
5 |
2 |
Not satisfied and worse |
0 |
Table 2: Simple shoulder test (1 point per question, Yes or No answers, Max score 12) |
1 |
Is your shoulder comfortable with your arm at rest by your side? |
7 |
Can you lift a 3kg dumb-bell to the level of the top of your head without bending your elbow? |
2 |
Does your shoulder allow you to sleep comfortably? |
8 |
Can you carry a 10kg bag of rice at your side with the affected extremity? |
3 |
Can you reach the small of your back to tuck in your shirt with your hand? |
9 |
Do you think you can toss a tennis ball underhand 10m with the affected extremity? |
4 |
Can you place your hand behind your head with the elbow straight out to the side? |
10 |
Do you think you can throw a tennis ball overhand 20m with the affected extremity? |
5 |
Can you place a coin on a shelf at the level of your shoulder without bending your elbow? |
11 |
Can you wash the back of your opposite shoulder with the affected extremity? |
6 |
Can you lift a basket ball to the level of your shoulder without bending your elbow? |
12 |
Would your shoulder allow you to work full-time at your regular job? |
3-Portal Arthroscopic Subacromial Decompression Technique
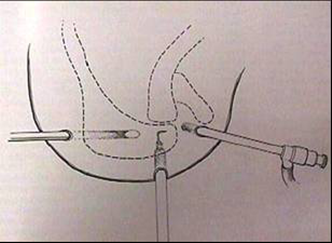
The traditional 3-port arthroscopic technique involves arthroscopic portals inserted through the posterior, anterior and lateral aspects of the shoulder (Fig 1). The posterior portal is located 2cm inferior and 1cm medial to the postero-lateral margin of the acromion. After a skin incision is made over the marked spot, an 18 gauge spinal needle is inserted into the glenohumeral joint and distended with normal saline. After a trocar and cannula are inserted into the posterior portal, the trocar is removed and an arthroscopic camera with an inflow of saline solution attached is then inserted through the cannula. The anterior portal is next established while observing the triangular intra-articular landmarks (glenoid, long head of biceps tendon, subscapularis tendon) via the arthroscopic camera.
After a spinal needle has been used to determine the correct entry point of the anterior portal, a cannula is then inserted into the glenohumeral joint via the anterior portal. A lateral arthroscopic portal is made through the subacromial region; about 3 cm distal from the lateral acromial border. The debriding instrument is inserted through the lateral portal to perform the bursectomy and to release the coracoacromial ligament from the edge of the acromion. The debriding instrument is also used define the antero-lateral border of the subacromial spur by identifying the lateral gutter. This is a crucial step as it helps prevent inadequate decompression of the spur but is often technically difficult to execute. A surgical bur is then inserted via the lateral portal and tilted anteriorly to address the antero-lateral acromial spur. We have found in our experience that insertion of the debriding instrument and burr via the lateral portal followed by anterior tilting of these instruments make it difficult to adequately address the antero-lateral subacromial spur and demarcate the lateral gutter. This increases the risk of inadequate subacromial decompression.
2- Portal Subacromial Decompression Technique
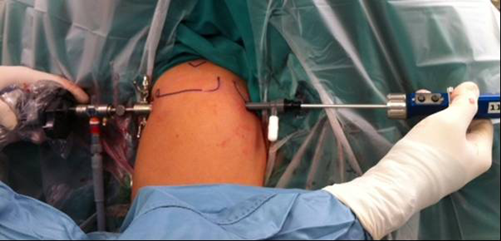
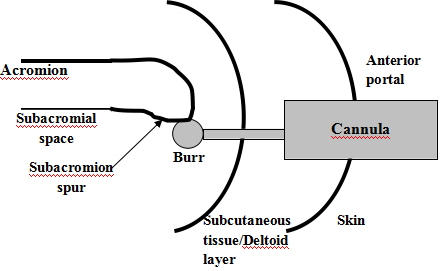
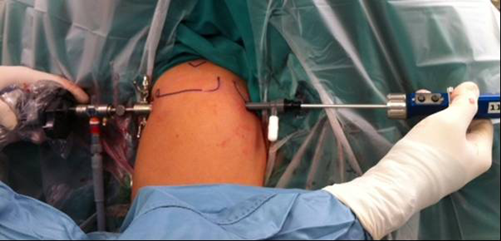
This procedure involves only two arthroscopic portals in the anterior and posterior aspect of the shoulder joint. The technique of establishing the posterior and anterior portals is the same as those of the 3-portal technique described above. The arthroscopic camera is inserted via the posterior portal while the debriding instrument or burr is inserted via the anterior portal (Fig 2). This enables the bone spur to be addressed head on rather than from an awkward angle (Fig 3).
Fig 2: Photo of the 2-portal ASD technique. |
|
Fig 3: Arthroscopic view of the subacromial spur through the anterior portal |

|
Fig 4: Schematic drawing of the cannula and burr insertion through the anterior portal. |
|
The cannula that holds the debriding instrument or burr is initially fully inserted into the subacromial space to create a tunnel for the instrument but is then withdrawn into the subcutaneous layer (Fig 4). The debriding instrument or burr is left in the subacromial space and is easily manoeuvred in an anterior-posterior or medial-lateral direction to ensure that the surgeon does not miss any part of the acromioplasty. As the burr is advanced into the subacromial space via the tunnel created by the cannula, care is taken to ensure it does not cause any soft tissue damage. This technique saves the need for a lateral arthroscopic portal which goes through the deltoid and may be painful for the patient. As the debriding instrument and burr are able to address the subacromial spur directly from the anterior portal, it is easier to define the antero-lateral borders of the spur and adequately burr it away.
Results:
Over a period of 36 months, 20 patients underwent ASD surgery and 20 shoulders were operated on. 20 out of 20 patients (100%) were satisfied with the outcome of their surgery. There were zero post-operative complications reported. Patients had a mean pre-operative Simple Shoulder score of 5.15 while their mean post-operative score was 10.9, showing a 112% improvement (p<0.001).
The maximum UCLA Shoulder Rating Score is 35. Scores of 33-35 are graded as excellent, 28-32 as good, 21-27 as fair and 0-20 as poor (Table 3). All of the patients included in the study had poor (90%) to fair (10%) UCLA shoulder scores prior to the procedure whereas the post-operative scores were mostly in the excellent range (60%). One patient had a poor outcome at 6 months due to recurrence of pain and subsequently defaulted follow up at our hospital. On average, there were significant improvements in all components of the UCLA score in our patients (Table 4).
Table 3: Post-operative UCLA Shoulder Rating scores |
|
Pre-operative |
Post-operative |
Excellent (33-35) |
0 |
12 (60%) |
Good (28-32) |
0 |
5 (25%) |
Fair (21-27) |
2 (10%) |
2 (10%) |
Poor (0-20) |
18 (90%) |
1 (5%) |
Table 4: Pre and post operative average UCLA component scores |
|
Max score |
Pre-op Score |
Post-op Score |
p-value |
Pain |
10 |
2.5 |
8.2 |
<0.001 |
Forward Flexion |
5 |
3.05 |
4.65 |
<0.001 |
Function |
10 |
5.50 |
9.00 |
<0.001 |
Power |
5 |
4.60 |
4.95 |
0.005 |
Satisfaction |
5 |
0.25 |
4.75 |
<0.001 |
Total UCLA |
35 |
15.90 |
31.55 |
<0.001 |
Discussion
Patients experiencing symptoms of subacromial impingement often have shoulder pain, reduced range of movement and weakness. The x-ray investigations for their symptoms should include an anterior-posterior, Y-scapular and supraspinatus outlet view of their shoulder. The supraspinatus outlet view allows the subacromial bony spur to be clearly seen and this allows better preoperative planning which will enable the surgeon to predict how much subacromial bone needs to be burred away. These patients should be given a trial of conservative management with non-steroidal anti-inflammatory analgesia, physiotherapy, modification of activities as well as subacromial injections for 6 to 12 months before being considered for surgery.
Other cause of shoulder pain such as rotator cuff or labral tears should be excluded before the patient undergoes ASD.
In 1985, Ellman first described the 3-portal arthroscopic subacromial decompression technique2. Since then there have been many debates comparing arthroscopic and open subacromial decompression surgery. Advocates of the open technique often cite technical simplicity and shorter operating times while advocates of the arthroscopic technique claim better cosmesis, deltoid preservation, faster recovery and the ability of the surgeon to inspect the glenohumeral joint.
Several studies have shown that both open and arthroscopic subacromial decompression have very similar outcomes3, 4, 5. Spangehl performed a prospective randomised blinded study comparing arthroscopic versus open acromioplasty3. He found that there was no significant difference between the two procedures in terms of post-operative visual analogue scores, patient satisfaction, UCLA shoulder scores or shoulder strength.
However the open procedure was found to be superior to the arthroscopic procedure in terms of post-operative pain and function. Lindh found similar functional outcomes for both groups of patients undergoing open and arthroscopic decompression after 2 years but the arthroscopic technique required less surgical time, resulted in earlier restoration of motion and a reduction of time off work4. Similarly Sachs found a more rapid recovery in their patients undergoing arthroscopic procedure but by 3 months the open group achieved the same result5. The results for pain, function motion and strength were equivalent in both groups.
In our experience performing arthroscopic subacromial decompression via this 2 portal technique, it was easier for the debriding instrument and burr to reach the antero-lateral subacromial spur, and to appreciate the full extent of the spur. These instruments also had greater range of movement in both the antero-posterior and medio-lateral directions to effectively excise the antero-lateral acromial spur and reduce the risk of inadequate acromioplasty. The 2-portal decompression technique obviates the need to incise the deltoid laterally with possible decrease in post-operative pain.
We compared our data with those published for 3-portal ASD and found our figures comparable to these data (Table 3)7,8,9. All patients showed significant improvement in their function, pain and strength of their shoulder.
Table 3: Comparisons between our 2-portal ASD technique data and data from other 3-portal ASD technique studies. |
UCLA Shoulder Rating Scale |
Poor (0-20) |
Fair (21-27) |
Good (28-33) |
Excellent(34-35) |
Our Study |
1(3.2%) |
5 (16.1%) |
13 (41.9%) |
12(38.7%) |
Lim et al (7) |
7% |
10% |
50% |
33% |
Ellman et al (8) |
4.6% |
6.2% |
53.8% |
35.4% |
Kim et al (9) |
0 |
15% |
54% |
31% |
One of the weaknesses with our study is the small number of patients recruited (n=20). A cohort study with a much larger sample size and a longer follow up would give a clearer assessment of the true effectiveness of our 2-portal ASD technique. A prospective study to directly compare this 2-portal and 3-portal technique would also significantly contribute to our hypothesis.
Conclusions
This study has shown that the 2-portal arthroscopic subacromial decompression technique is feasible, effective and safe for patients with Neers 1 and 2 chronic shoulder impingement syndromes.
References.
Neer CS II. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am 1972, 54:41-50
Ellman H. Arthroscopic subacromial decompression: analysis of one to three year results. Arthroscopy 1987; 3: 173-81
Spangehl MJ, Hawkins RH, McCormack RG et al. Arthroscopic versus open acromioplasty: A prospective randomised, blinded study. J Shoulder Elbow Surg 2002; 11: 101-107
Lindh M, Norlin R. Arhtroscopic subacromial decompression versus open acromioplasty. A two-year follow up study. Clin Orthop 1993; 174-6
Sachs RA, Stone ML, Devine S. Open vs Arthroscopic acromioplasty. A prospective, randomised study. Arthroscopy 1994; 10: 248-54
Fieman BG, Fenlin JM Jr. Anterior acromioplasty: effect of litigation and workers’ compensation. J Shoulder Elbow Surg 1995; 4: 175-81
KK Lim, HC Chang, JL Tan, BK Chan, Arthroscopic subacromial decompression for stage-II impingement. J Orthop Surg 2007;15(2):197-200
Ellman H, Kay SP. Arthroscopic subacromial decompression for chronic impingement. Two- to Five-year results. J Bone Joint Surg Br. 1991 May; 73(3):3958.
Kim JS, Lee JQ, Kim BS. Arthroscopic decompression for subacromial impingement syndrome. J Korean Med Sci. 1997;12(2):123-7 |