|
Abstract:
Introduction
Despite advances in orthopaedic surgical techniques, management of infected non-unions of long bones still poses a great challenge for any orthopaedic surgeon. This may include a radical debridement of the septic bone and soft tissue, thereby creating a big defect at the non-union site. Routine procedures for fracture fixation generally fail and special techniques may have to be employed.
Methods
A prospective study was undertaken to evaluate the efficacy of Ilizarov ring fixator for the treatment of infected non-union of tibia and femur. Thirty patients with an average age of 37.63 ± 11.54 years (range, 25 64 years) with infected non-union of tibia and femur were included in the study. All patients were treated with thorough debridement of the infected non-union site, followed by Ilizarov external fixator application. The fixator was kept of an average period of 6.67 ± 0.80 months (range, 5 8 months). Patients were followed up for a mean period of 7.87 ± 1.78 months (range, 6 14 months).
Results
The outcome was assessed by the criteria dictated by Association for the Study and Application of the Method of Ilizarov (ASAMI). Five patients (16.6%) had excellent results, 17 patients (56.6%) had good results, five patients (16.6%) had fair results and three patients (10%) had a poor result.
Conclusion
Treatment of infected non-unions of tibia and femur by Ilizarov technique offers a very effective and reproducible method of therapy.
J.Orthopaedics 2012;9(3)e8
Keywords:
Infected non-union; Femur and Tibia; Ilizarov ring fixator
Introduction:
Management of infected non-union is a challenge for orthopaedic surgeons. The literature endows several methods for the treatment for infected non-union like bone grafts, extensive debridement and local soft tissue rotational flaps, packing of the defects with Papineau-type open cancellous bone grafting, bony synostosis and free microvascular soft tissue and bone transplants and many more.1,2 None of the previously mentioned techniques afford the surgeon ability to correct the deformities, eliminates prolonged pre and post-operative intravenous antibiotic therapy, regenerates new bone tissue without the use of bone grafts, progressively lengthens the extremity and allows weight bearing during the treatment period.3 In addition, stabilizing the fracture in presence of infection is a real challenge, as most implants cannot be used when there is significant infection locally.4
Patients with such diagnoses have usually been treated by a series of different surgical treatments, including sequestrectomies, drainage, and massive cancellous bone grafts. These techniques are often unsuccessful because the infection is difficult to eradicate due to poor vascularization of the bone.5, 6 Application of Ilizarov ring fixator method allows all these problems to be addressed simultaneously.7 Difficult or resistant infections usually require a radical debridement of the septic bone and soft tissue in addition to the application of stable fixation to enhance soft tissue healing and bone union.3,8 Bone defects in this situation can be filled up either by acutely shortening the bone or gradually transporting a segment to fill in the defect.
Methods ::
A prospective study was carried out at our Institute between July, 2008 and October, 2011. A total of thirty patients of infected non-union of femur and tibia were included in this study. Patients below 18 years of age were excluded from the study as in this age group, the chances of bony union is high even with conventional methods of treatment. Eight patients had been managed initially in our department; the other 22 had been managed elsewhere initially and were subsequently referred to our institution for treatment of non-union and infection. All patients were followed up for a mean period of 7.87 ± 1.78 months (range, 6 14 months).
There were 24 males (80%) and 6 females (20%) with mean age of 37.63 ± 11.54 years (range, 25 64 years). Of these, 21 patients (70%) were in the age group of 21 to 40 years. Twenty one non-unions (70%) were located in tibia and the rest in femur. Road traffic accidents were the cause in 25 patients (83.3%), falls in three (10%) and pathological fracture due to osteomyelitis of the involved bone leading to infected non-union in two patients (6.6%), with the right side affected in 25 patients.
Twenty two of the non-unions had developed after an open fracture and eight, after a closed fracture, initially. Mean time of presentation since initial injury was 13.67 ± 2.88 months (range, 9 19 months). Majority of patients (18 patients) presented to us within 15 months of sustaining injury. But this difference was not statistically significant (p = 0.2733). The patients had an average of 3.23 ± 1.33 operations (range, 1 6 operations) for treatment of original fracture, infection or non-union. Eleven patients had undergone four or more surgical procedures prior to admission to our institution. A fracture was considered to be infected non-union, if after 6 months from the initial injury, there was clinically apparent motion at the site of fracture along with formation of a sinus, indicating presence of dead bone or sequestration; or extensive osteomyelitis; or if there was an exposed dead bone or metal.
At the time of presentation, ten patients had chronic discharging sinus in relation to the infected non-union site, one had knee flexion contracture and five patients had fixed equinus deformities at the ankle. Staphylococcus aureus grew on culture from specimens obtained from infected non-union site of 21 patients. Streptococcus pyogenes was the next most common organism isolated, followed by Pseudomonas aeruginosa and others. In one patient, no organism could be isolated, perhaps due to coverage provided by broad spectrum antibiotics. The mean pre-operative shortening was observed to be 2.36 ± 0.45 cm (range, 0 3 cm).
Eight patients (26.7%) with infected non-union had shortening of up to 2.5 cm. Only three of them (10%) had lost more than 2.5 cm of bone prior to surgical intervention.
Majority of patients (27 patients, 90%) were managed by applying compression at the fracture site through the Ilizarov apparatus. These were managed with excision of intervening fibrous tissue and infected dead bone to expose fresh bleeding bone ends, which were approximated and acutely compressed with the Ilizarov fixator. The average bone defect after debridement was 2.30 ± 0.66 cm. Two patients developed significant bone defect after debridement. Lengthening was performed in these patients in a staged fashion, so that final limb length discrepancy was minimised. The Ilizarov frame was applied in static mode for the entire course of treatment, in one patient. Average resultant bone defect after debridement was 2.28 ± 0.66 cm (range, 0 4 cm).
Post operatively, appropriate antibiotics were administered to all patients according to the bacterial culture taken intra-operatively from the bone and surrounding tissues. Analgesics and anti-inflammatory drugs were given as required. Limb elevation and active toe movements were advised as soon as pain subsided. Once patients general condition improved he was advised to walk with the help of crutches. Wire tension and frame integrity was checked regularly, on a daily basis. Pin tract infections were managed with appropriate antibiotics and dressings. All patients were encouraged to move around in hospital surroundings to create an atmosphere of wellbeing. Neighboring joints were mobilized to prevent joint stiffness with the help of physiotherapist. Compression-distraction was done at regular intervals at the rate of 1 mm/day in four sittings every day. This was done for a mean period of 2.73 ± 0.52 months (range, 2 4 months). The frame was then kept in static mode for the regenerate to consolidate for an average of 3.93 ± 0.74 months (range 3 5 months). Therefore, total time in frame for all the patients in our study was 6.67 ± 0.80 months (range, 5 8 months).
Results :
Of the total of 30 patients, union was achieved in all patients. The mean time to union was 7.41 ± 1.01 months (range, 6 9 months). A case study is shown in Figures 1 to 4. Two patients developed wound infection which required repeated debridement and dressings along with prolonged broad spectrum antibiotic cover. Four patients had pin tract infections which were managed by local dressings and oral antibiotics. Five of them developed pin loosening during the course of treatment. Despite established infection at the beginning of the treatment, the rate of complications by the Ilizarov method was significantly low with p < 0.01. Average deformity at the fracture non-union site at the end of treatment was 6.40Ί ± 4.05Ί (range, 0Ί - 15Ί). Mean shortening at the time of final follow-up was 3.36 ± 0.99 cm (range, 0 to 5 cm). Sixteen patients had more than 3 cm limb length discrepancy (p = 0.7153). This was accepted as a price to pay for achieving union at the non-union site by compression.
The results were based on the classification of Association for the Study and Application of the Method of Ilizarov (ASAMI) which include observation of four clinical criteria: fracture union, infection, residual deformity and limb length discrepancy at final follow-up.9
This classification is applicable for tibial and femoral infected non-unions. An excellent result was defined as a union with no infection, deformity of less than 7° and a limb length discrepancy of less than 2.5 cm. A good result was defined as a union with any two of the other two criteria. A fair result was defined as a union with any one of the other criteria. A poor result is defined as a non-union or refracture during treatment or as a union but with none of the remaining three criteria satisfied.
In the present study, each patient was graded using this protocol and the final result was depicted as excellent, good, fair and poor. Five patients (16.7%) had excellent, 17 patients (56.7%) good, five patients (16.7%) fair and three (10%) had poor results. Excellent and good results were considered to be acceptable. Therefore, 22 patients were labeled as having acceptable results. This was significant statistically, with p = 0.0106.
Discussion:
The problem of non-union has been known to orthopaedic surgeons since they have started treating fractures. Fractures fail to unite as a result of damage from the initial injury and mechanical instability, which are further compounded by bone loss, osteomyelitis, multiple surgical procedures, disuse osteoporosis, soft tissue atrophy and decreased arterial blood flow. Non-union of long bones with infection has always been a challenge for orthopaedic surgeons. Secondary procedures are often required for correction of bone defects and deformity. This eventually results in multiple surgeries and scarring of tissues with joint stiffness and oedema, which interfere with an optimal limb function. The challenge is compounded by additional factors like presence of deformity, loss of bone, leg length discrepancy and soft tissue damage.
Bone union in these situations is not obtained until infection is eradicated.7
Many studies have suggested multidisciplinary approach in the management of these patients.10 A vast majority of patients during the course of treatment tend to be depressed and need to be counselled repeatedly. The reasons for depression were mainly due to the multiple failed attempts at union, pain, and financial and social constraints. Despite adequate counselling few patients inevitably discontinue the treatment and opt for amputation.
In 1951, G.A. Ilizarov and his colleagues in the Siberian city Kurgan developed a technique for the treatment of chronic osteomyelitis and bone defects created by extensive debridement known as distraction osteogenesis.11
Over the years, the method proved to be so widely applicable and effective that the Association for the Study and Application of the Methods of Ilizarov (ASAMI) was established in Lecco, Italy, in 1982.12 Ilizarov discovered that living tissue, when subjected to slow steady traction, becomes metabolically activated in both the biosynthetic and proliferative pathways, a phenomenon dependent on vascularity and functional use.11 Application of this method allows the problems of non-union, infection, shortening, deformity and osteoporosis to be addressed simultaneously.7 Ilizarovs method has proved its efficacy in the treatment of post-traumatic infected non-unions of long bones where other types of treatment have failed.
Final result of treatment is usually assessed by the criteria given by ASAMI group. These include four parameters: bone union, infection, deformity and limb length discrepancy at the time of final follow up. Most studies in the literature have shown about 70 90% acceptable results.3,7,13, 14,15 (Table 1) Rose et al, had a 50% favourable result, but since they studied a very small group of patients (eight in number), their results were not statistically significant.13 In the present study, 30 patients with established infected non-union of tibia and femur were evaluated. Union was achieved in all the patients at an average time of 7.41 ± 1.01 months. An acceptable result of 73.33%, was observed which is comparable to various other studies published in the literature.
Infected non unions are fairly common in the younger age group, which is the most productive age of life. Loss of income due to prolonged recumbency inherent in the conventional treatment results in grave financial crisis for the patient. Most patients, who eventually develop infected non-union, have an open fracture at the beginning. Inadequate management of such injuries leads to the development of infected non-union. Compression at the non-union site by Ilizarov fixator achieves best results.
Ilizarov treatment ensures that there is micro motion at the site of fracture non-union, which stimulates new bone formation. Treatment by this method allows the patient to bear weight and pursue his / her job responsibilities, even while undergoing treatment. Ilizarov method gives consistently good results even in the presence of established infection, where other conventional methods of treatment fail. It is therefore a very effective and reproducible method of treatment for infective non unions of long bones.
References:
- Edward CC, Simmons SC, Bowner BD, Weigle MC. Severe open tibia fractures. Results treating 202 injuries with external fixation. Clin Orthop Relat Res 1988;230:98-115
- Tucker HL, Kendra JC, Kinnebrew TE. Tibia defects: Reconstruction using the method of Ilizarov as an alternative. Orthop Clin North Am 1990;21(4):629-37.
- Hosny G, Shawky MS. The treatment of infected non-union of the tibia by compression-distraction techniques using the Ilizarov external fixator. Pan Arab J Orth Traum 1998;1:11-6
- .
Farmanullah, Khan MS, Awais SM. Evaluation of management of tibial non-union defect with Ilizarov fixator. J Ayub Med Coll Abbottabad 2007;19(3):34-6.
- Green SA, Dlabal TA. The open bone graft for septic non-union. Clin Orthop Relat Res 1983;180:11724.
- Reckling FW, Waters. Treatment of non-unions of fractures of the tibial diaphysis by posterolateral cortical cancellous bone-grafting. J Bone Joint Surg Am 1980;62:93641.
- Dendrinos GK, Kontos S, Lyritsis E. Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg Am 1995;77(6):83546.
- Heppenstall RB. The present role of bone graft surgery in treating non-union. Orthop Clin North Am 1984;15(1):11323.
- Association for the Study and Application of the Method of Ilizarov Group: no- union of the femur. In: Bianchi-Maiocchi A, Aronson J, editors. Operative principles of Ilizarov. Fracture treatment, non-union, osteomyelitis, lengthening, deformity correction. Baltimore: Williams and Wilkins; 1991.
- Marsh DR, Shah S, Elliott J, Kurdy N. The Ilizarov method in non-union, malunion and infection of fractures. J Bone Joint Surg Br 1997;79:273-9.
- Ilizarov GA: The principle of Ilizarov method. Bull Hosp Joint Dis Orthop Inst 1998;48(1):1-11.
- Rang M. The story of Orthopaedics. Philadelphia: WB Saunders Company; 2000.
Rose REC, Palmer O. The Ilizarov method in infected non-union of long bones. West Indian Med J 2007;56(3):246-51.
- Maini L, Chadha M, Vishwanath J. The Ilizarov method in infected non-union of fractures. Injury 2000;31(7):50917.
- Pruthi KK, Sahu SC, Chandra H, Dhawan S. Treatment of non-union of tibia by Ilizarov technique. Indian journal of orthopaedics.1994 May;28(2):10-15.
TABLES
Study |
Acceptable
(Excellent + Good) |
Not acceptable
(Fair + Poor) |
p-value |
Hosny et al3 [n=11] |
8 |
3 |
0.7193 |
Dendrinos et al7 [n=28] |
24 |
4 |
0.4017 |
Rose et al13 [n=8] |
4 |
4 |
0.4047 |
Maini et al14 [n = 30] |
24 |
6 |
0.7600 |
Pruthi et al15 [n=28] |
26 |
2 |
0.1053 |
Present series [n=30] |
22 |
8 |
--- |
Table 1: Comparison of results of various studies of treatment of infected non-unions with Ilizarov fixators
FIGURES
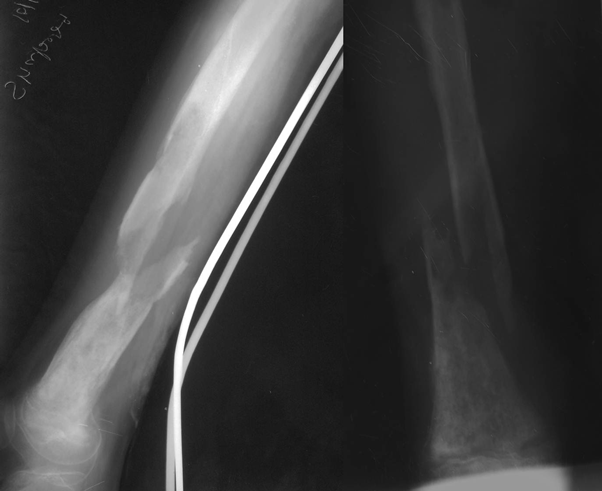
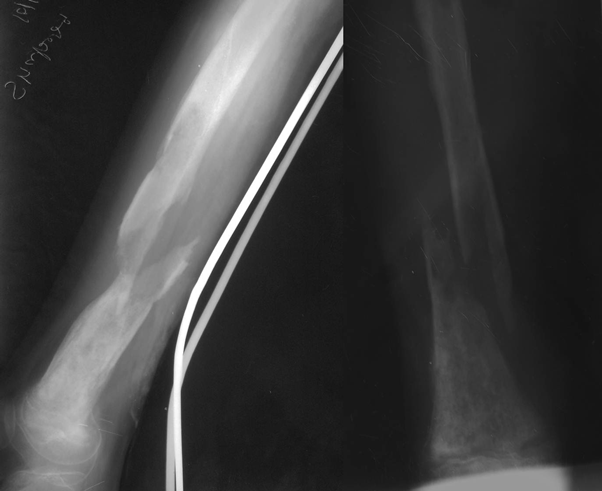
Figure 1: Radiographs at presentation showing infected non-union of femur

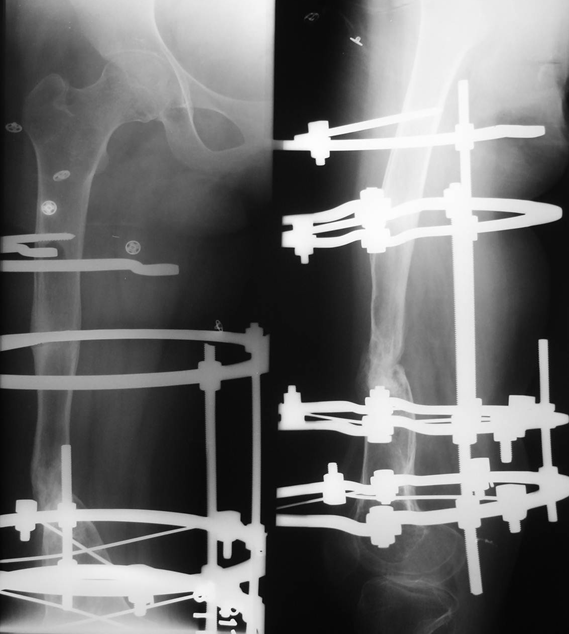
Figure 2: Radiographs after debridement, primary docking and Ilizarov ring fixator application
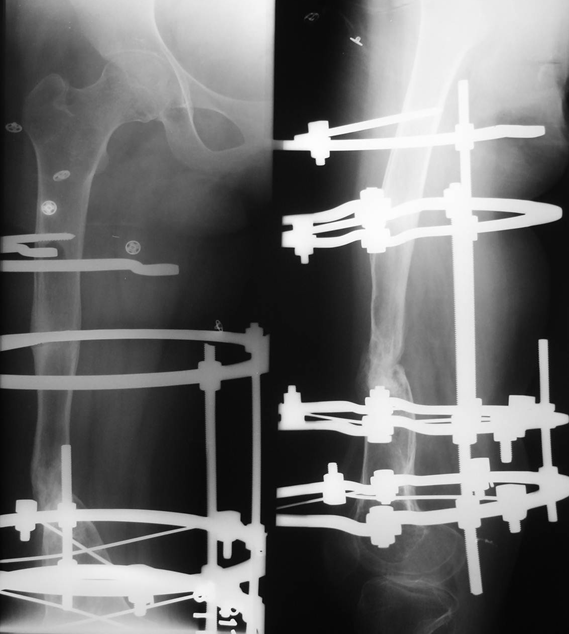
Figure 3: Radiographs showing union at fracture site with Ilizarov fixator in situ


Figure 4: Radiograph at the time of last follow-up, showing fracture union
|