Abstract:
Word Count: 3316 A research grant in support of this work was received from Synthes Spine.
Study Design:Spondylolysis was created in an in vitrocalf spine model. Three constructs were applied to stabilize the defects created. Intervertebral rotation and pars defect displacement were studied after stabilization.
Objective: To quantify the effect of pars defects on intervertebral rotation and the stability of three repair techniques utilizing cervical implants which might be useful in small stature individuals.
Summary of
Background Data: Previous work has demonstrated the efficacy of lumbar pedicle screw hook rod (PSHR) techniques and the Buck screwin the stabilization of spondylolysis. The mechanical behavior of lower profile cervical implants used to create PSHR, hybrid cable plate constructs, and titanium mini-plating has not previously been described.
Methods: Calf lumbar spines (L2-L6) were utilized for testing (n=27). Intervertebral rotation was measured in the intact spines across the L4-5 segment before and after creation of bilateral pars interarticularis defects. Defects were then stabilized with one of three repair techniques, PSHR, mini-plate, or cable plate (CP) constructs. (n=9). Rotational torque (5Nm) was applied in flexion extension, lateral bending and axial rotation. Defect displacement was measuredunder flexion extension and lateral bending modes.
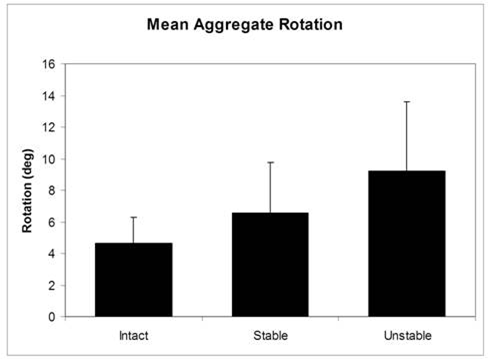
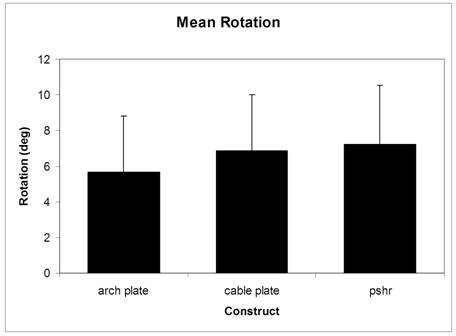
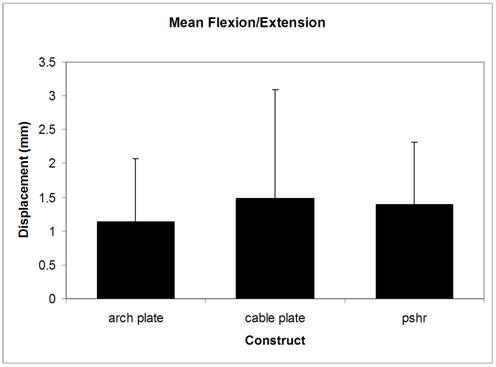
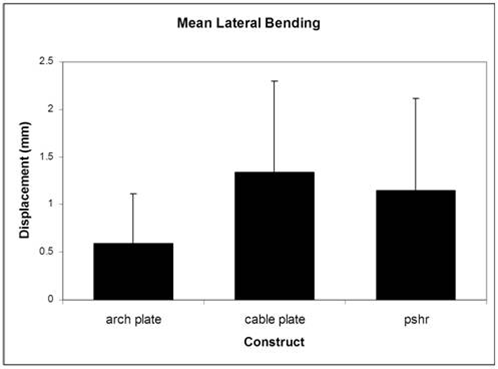
Results:Osteotomy of the pars interarticularis increased intervertebral rotation from 4.6° to 9.2° (p<.05). The three techniques of repair reduced intervertebral rotation without statistical superiority of one method. In lateral bending the mini-plate was most effective in reducing pars defect displacement (0.6mm, p<0.05). Although the mini-plate provided better stabilization of defect displacement in flexion extension and axial rotation, these differences were not statistically significant.
Conclusions:Bilateral mini-plate fixation demonstrates superiority in restoring stability in lateral bending as compared to pedicle screw hook rod techniques and cable plate constructs. In flexion extension and axial rotation, it was as effective as a PSHR method. Consideration of anatomic plate designs warrants consideration.
J.Orthopaedics 2012;9(2)e5
keywords: Spondylolysis, Biomechanical testing, pars interarticularis, spinal&nb
Mini Abstract
This investigation quantified biomechanical effects of experimentally induced pars defects with three different repair techniques using cervical implants in a cadaveric benchtop model.Pars osteotomy significantly increased intervertebral axial rotation. The three methods compared reducedintervertebral rotation. Mini-plate fixation provided better defect stabilization in lateral bending than cable plate or PSHR.sp;stability
Introduction:
Spondylolysis is an acquired stress fracture of the pars interarticularis, which occurs in childhood or adolescence. Unilateral or bilateral lesions may be associated with pain, however, as only bilateral lesions progress to spondylolisthesis, greater clinical concern is reserved for bilateral defects. A radiographic survey of first graders in North America documented bilateral spondylolytic defects in5% of the study population. Risk factors associated with an increased incidence of spondylolysis include age , sex , , , race , family history , and participation in sports. While spondylolysis develops more commonly in boys; spondylolisthesis occurs more commonly in girls. A genetic susceptibility to spondylolysis is supported by the varying frequency of occurrence amongst different ethnic groups. The highest prevalence of spondylolysis has been reported in Inuit Eskimos of whom approximately 25% have pars defects. In contrast, blacks are less likely to be affected than whites. , There is a 15%-70% association of the disease in first degree relatives of affected individuals. ,
A classification scheme has been proposed by Herman and Pizzutillo, which may have prognostic implications regarding the healing potential of the lesions. Within the traumatic subtype of this classification, there are acute and chronic types. The acute type is generally considered the result of a single high-energy traumatic event and hence has a distinctly different biological behavior than the more common type, which is felt to arise from repetitive microtrauma. The chronic types are divided into stress reactions, stress fractures, and spondylolytic defects. Intraosseous edema with surrounding sclerosis of the pars, lamina, or pedicle without cortical or trabecular disruption is termed a stress reaction. When encountered at this stage, most defects heal with rest and immobilization. Disruption of the trabecular or cortical bone of the pars without a bony gap or is termed a stress fracture. Complete disruption of the
pars interarticularis with a gap and surrounding sclerosis at the edges of the defect is defined as a spondylolytic defect or nonunion of the pars. Painful nonunions associated with bony defects are the subtype most likely to benefit from operative intervention.
When the lumbar spine is extended, pressure is transmitted from the superior vertebra’s inferior articular process to the inferior vertebra’s pars interarticularis. , Stress fractures can develop over time with repetition. Sports such as tennis, gymnastics, football, and swimming, require more lumbar hyperextension leading to a higher percentage spondylolysis in these populations. , , , , ,
For the child or young adult with disabling symptoms, which preclude participation in vigorous activity, or with significant pain with activities of daily living, surgical intervention may be warranted. Surgical options for repair of the pars interarticularis parallel those used for repair of any pseudoarthrosis. Debridement of fibrocartilaginous debris from a typical defect results in the creation of a segmental bony defect, which must be filled. A structural autologous bone graft has been advocated in several series to bridge the defect and to prevent iatrogenic shortening of the pars interarticularis during the application of compression across the nonunion site.
Multiple methods of internal fixation have been described as a means of stabilization of the spondylolytic defect. One of the earliest techniques described is the Scott Technique, which consisted of a wire looped around the spinous process and lamina, stabilized to the transverse process. This technique has largely been abandoned due to the difficulty of the technique and the development of better options. Bilateral screw fixation placed across the lamina and into the pedicle base (Buck’s technique) is inherently appealing given the capacity to provide compression across the defect. The difficulty of achieving an appropriate screw trajectory combined with the risk of screw fatigue has prompted a search for more effective means of repair. Use of a hook screw has been described with a laminar hook applied to the caudal end of the lamina and anchorage into the junction of the superior facet and lamina on the same side. The use of bilateral pedicle screws attached to a V-shaped rod applying cranially oriented compression force to the spinous process has been described.
Finally, bilateral screw fixation attached to laminar hooks via longitudinal rods has been described combined with structural bone grafting of the debrided pseudoarthrotic defect. This technique of repair has been shown in biomechanical studies to have equivalent mechanical performance in stabilization of the pars interarticularis defect when compared to the Buck technique.
The existence of a plethora of stabilization techniques provides an insight into the problems associated with pars defect repair. While the aforementioned methods provide varying degrees of stability, all have some inherent drawbacks. In an attempt to improve upon the existing methods, we sought to investigate the utilization of smaller implants to lessen the likelihood of implant prominence. In addition, we propose that the technique of repair include a buttress effect using a plate applied dorsal to the lamina and pars to prevent dorsal migration of an applied structural bone graft.
Materials and Methods
Biomechanical Study.
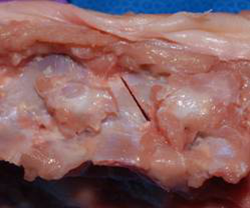
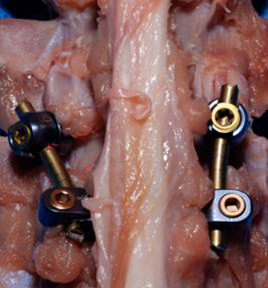
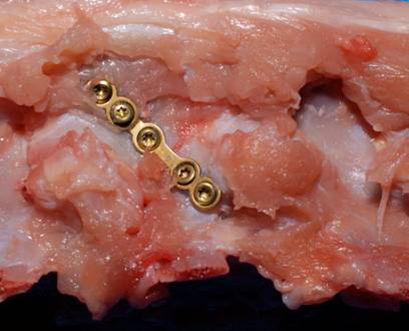
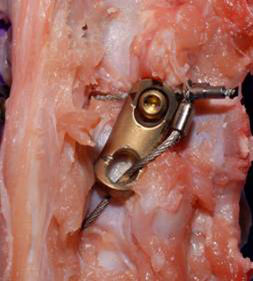
Twenty-seven fresh frozen calf lumbar spines (male Holstein species, aged 7-14 days, average weight 50kg at harvest) were obtained and stripped of unnecessary muscle tissue while maintaining all ligaments and joint capsules. L2 and L6 were embedded in polymethylmethacrylate allowing motion at L2-3, L3-4, L4-5, and L5-6. Rotational testing was performed on specimens before and after creation of bilateral spondylolytic defects in L4 using an oscillating saw (Figure 1). Subsequently, 3 repair techniques—pedicle-screw-hook-rod, arch plate, and cable plate constructs—were applied with nine spines per group (Figures 2,3,4).
Biomechanical Testing. L2 and L6 were attached to custom grips for attachment to the Instron. Loads were applied using an Instron 1122 Materials Testing Machine (Instron Corporation, Norwood, MA) with a spine testing fixture described in previous publication from our laboratory.
Testing was performed in axial rotation, lateral bending, and flexion/extension using an applied load of 5 Nm with a 50-N compressive preload to simulate the effects of the in vivo muscular envelope. Specimens were subjected to two preconditioning load cycles with data collected from the third cycle used for analysis. Intervertebral rotation was measured across the L4-5 motion segment using a custom rotational transducer. The rotational transducer was rigidly fixed to the L4 and L5 vertebral bodies using K-wires and a mini vertebral halo ring (Figure 5). In addition, displacements across the defects on each side were measured by linear extensometers and were averaged. Data acquisition was continuous throughout each test ata sampling rate of 10Hz and stored in a computer data file. Data analyzed included intervertebral rotation at L4-5 under torsional load (axial rotation), displacement across the fixated defect in lateral bending, and flexion/extension.
Statistical Methods.
One-way analysis of variance (ANOVA) was used to test for any significant differences (p<0.05 significant) between spine condition (intact, unstable, or repaired) and treatment groups (pedicle-screw-hook-rod, arch plate, or cable plate) in axial rotation, flexion/extension, and lateral bending. Post-hoc Fisher’s protected least squares difference (PLSD) tests were performed to detect pair-wise differences when appropriate. A pretest power analysis predicted that twenty-seven specimens were required to reach statistical significance.
Results
Specimens were generally of the same size and shape. Catastrophic failure did not occur in any of the motion segments or in any of the instruments all through the biomechanical testing. All needles holding the extensometers in the spinal elements were confirmed stable after each series of testing.
Intact spines refer to spines without the spondylolytic defects. Unstable spines refer to spines with bilateral spondylolytic defects but without fixation devices. Stabilized spines refer to spines with bilateral spondylolytic defects with fixation devices. The three fixation devices utilized in this study as mentioned above are the arch plate, cable plate, and pedicle-screw-hook-rod.
Results in Axial Rotation
Prior to osteotomy of the pars interarticularis, an average of 4.6 degrees of intervertebral rotation was measured across the L4-5 segment (n=27, SD=1.6, SE=0.314). Bilateral osteotomy of the pars interarticularis increased the mean intervertebral rotation to 9.2 degrees (n=27, SD= 4.3, SE=0.843) When examined in aggregate, all three methods combined reduced intervertebral rotation to a mean of 6.5 degrees (n=27, SD= 3.17, SE=0.843) (Figure 6). The difference between all means was statistically significant using
Fisher’s exact test.
The titanium mini plate (arch plate) was most effective at reduction of intervertebral rotation with reduction of intervertebral rotation to 5.6 degrees (n=9, SD=3.17, SE=1.057). The cable plate method reduced intervertebral rotation to 6.86 degrees (n=9, SD=3.1, SE=1.05) and the pedicle screw-hook-rod method was least effective in the reduction of intervertebral rotation to normal values with a mean intervertebral rotation of 7.2 degrees (n=9, SD=3.3, SE=1.11). While the mini-plate method showed the greatest trend towards reduction of intervertebral rotation, the differences between the mean values was not statistically significant. The mean values seen with each stabilization method used are depicted in Figure 7 below.
Flexion Extension Results.
All fixation methods resulted in some degree of displacement across the stabilized pars interarticularis defect when subjected to flexion extension rotational torque. As we recorded data from the left and right pars interarticularis defects in flexion extension and lateral bending, 9 sets of paired data or 18 data points were available per construct tested. The titanium miniplate (arch plate) was most effective in reducing spondylolysis gap displacement with a mean displacement of 1.14 mm (n=18, SD=0.93, SE=0.22). The cable plate construct and PSHR methods showed greater degrees of gap displacement with the cable plate technique allowing 1.48 mm of gap displacement (n=18, SD=1.61, SE=0.38) and the PSHR method allowing 1.39 mm gap displacement (n=18, SD=0.92, SE=0.22). The differences between the mean values recorded did not reach statistical significance. The mean values noted are depicted in Figure 8.
Lateral Bending Results
When subjected to rotational torque in lateral bending the arch plate was significantly more effective in reducing pars defect displacement than the cable plate or PSHR methods. The arch plate demonstrated a mean gap displacement of 0.59mm (n=18, SD=0.52, SE=0.12), while the cable plate method allowed a mean of 1.34 mm gap displacement (n=18, SD=0.96, SE=0.23) and the PSHR method allowed 1.15mm gap displacement. The mean difference between the arch plate and cable plate was statistically significant (p<0.05) while the difference between the arch plate and PSHR approached statistical significance (p=0.052). Results in lateral bending are depicted graphically in Figure 9.
Discussion
Axial Rotation Testing
.
Using our testing methodology, an average of 4.6 degrees of intervertebral rotation was recorded at the L4-5 segment in intact spine specimens (n=27). Deguchi et al42 in contrast reported 3.25 degrees mean intervertebral rotation in their intact bovine spine group. These values compare favorably to human and calf spine biomechanical data published by Riley et al who reported a mean axial rotation of 2.08 degrees in a bovine model and 4.7 degrees in a human cadaveric model. The previous authors, however, reported an average calf age of 19 weeks and 200kg weight at harvest. Similarly, Wilke et al reported a mean axial rotation at L4-5 of 1.3 degrees in their bovine lumbar spine model. Again in their series, the average calf age at spine harvest was 16 weeks with an average subject weight of 179kg. In our study population, the average calf age was less than 2 weeks with an average calf weight of 50kg. The diminutive size and mass of the spines in our test series is likely responsible for the slightly increased rotation recorded in our series. Clearly the specimen size and mass in other authors’ series would not accurately model a small statured pediatric population. Rather, we propose that our mean calf weight of 50 kg more closely simulates a smaller juvenile human spine.
After creation of bilateral defects, we recorded an increase in axial rotation at L4-5 to 9.2 degrees. This result again compares favorably to the results of previous authors who noted an increase in L4-5 axial rotation to 8.01 degrees from an intact spine baseline mean of 3.25 degrees.42 In our series no construct type returned axial rotation at L4-5 to baseline values. In terms of rank order efficacy, however, the titanium miniplate (M=5.6°, SE=1.057) was more effective than the cable plate method (M=6.86°, SE=1.05), which was more effective than the pedicle screw hook rod device (M=7.2°, SE=1.11). While the above differences did not demonstrate statistical significance, the aggregate reduction in mean of all methods combined was significantly different than the mean of all destabilized.
In previous comparisons of technique42, a modified Scott’s technique—pedicle screw with wire loop around the lamina—was noted to reduce rotation more so than hook rod, Buck and classic Scott’s technique—transverse process/laminar looped wire. Ulibarri et al reported stiffness data (Nm/deg) rather than angular displacement (degrees axial rotation) after repair of the spondylolytic defect. They rank ordered repair stiffness in axial rotation of different constructs noting that pedicle screw cable methods and an intralaminar link construct were stiffer than the intact spine, which was stiffer than a pedicle screw cable system. In their series, the Scott wiring technique was significantly less stiff than the intact spine in axial rotation.45
Flexion Extension Differences.
In our series there was no significant difference between the method of repair used and the magnitude of defect displacement measured when subjected to flexion extension moments. Mean gap displacements when rank ordered least to most were titanium miniplate (M=1.14 mm,SE=0.22),pedicle screw hook rod (M=1.38mm, SE=0.38), and cable plate (M=1.48, SE=0.22). Ulibarri et al similarly did not find significant differences in spondylolysis gap displacement in flexion extension testing. However, in their series an intralaminar link construct and pedicle screw hook construct were more effective than a pedicle screw cable construct.45
Lateral Bending Differences
Interestingly, previous authors have not reported the effect of stabilization of the simulated pars defect subjected to lateral bending moments, confining their testing protocols to axial rotation and flexion extension modes only.45, It was in this mode of testing, however, that we demonstrated the greatest difference between the plating method and cable or hook rod technique.There was significantly less defect displacement in the titanium miniplate group with a mean displacement of 0.59 mm, then with means of 1.15mm and 1.34mm for the PSHR and cable plate methods, respectively. Clearly, lateral bending movements are essential to activities of daily living and upon return to athletic activity. Hence, the favorable effect of miniplate fixation in this mode of loading may have a positive clinical effect.
Study Limitations
With this study we have attempted to compare two novel methods of pars defect repair to a previously established gold standard stabilization method. While nondestructive testing is described, we have not analyzed the effects of cyclic loading and the capacity of these methods to withstand a million cycles of load which might be experienced during the first three to four months of bone healing.
Conclusions
While pedicle screw rod techniques have previously shown mechanical superiority to other methods of pars interarticularis repair stabilization, titanium miniplate and hybrid cable plate techniques warrant further investigation and clinical application given their comparative efficacy in prevention of spondylolysis gap displacement and intervertebral rotational displacement. .
Figure legends
Figure 1. Bilateral spondylolytic defects in L4 using an oscillating saw.
Figure 2. Pedicle-screw-hook-rod construct applied over spondylolytic defects.
Figure 3. Arch plate construct applied over spondylolytic defects.
Figure 4. Cable plate construct applied over spondylolytic defects.
Figure 5. Rotational transducer rigidly fixed to L4 and L5 vertebral bodies using K-wires and a mini vertebral halo ring.
Figure 6. Osteotomy of the pars interarticularis doubled the amount of intervertebral rotation (p<0.05). Stabilization of the pars interarticularis produced a significant reduction in the amount of intervertebral rotation (p<0.05)
Figure 7. The arch plate was the most effective in reducing intervertebral rotation. This trend was not statistically significant
Figure 8. There were no significant differences in fracture gap displacement between the 3 constructs tested in flexion extension
Figure 9. In lateral bending, the titanium miniplate was significantly better in reducing gap displacement when compared to the PSHR and cable plate (p<0.05)
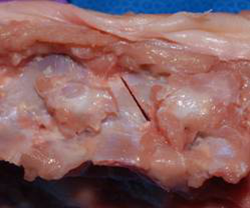
Figure 1. Bilateral spondylolytic defects in L4 were created using an oscillating saw.
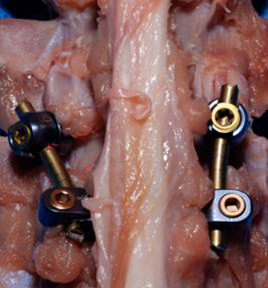
Figure 2.Pedicle-screw-hook-rod construct applied over spondylolytic defects.
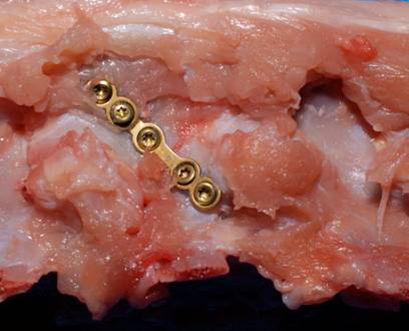
Figure 3.Side view of mini plate construct applied over spondylolytic defect.
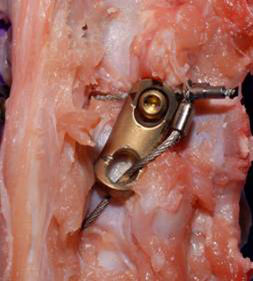
Figure 4.Side view of Cable plate construct applied over spondylolytic defects.

Figure 5. Rotational transducer rigidly fixed to L4 and L5 vertebral bodies using K-wires and a mini vertebral halo ring.
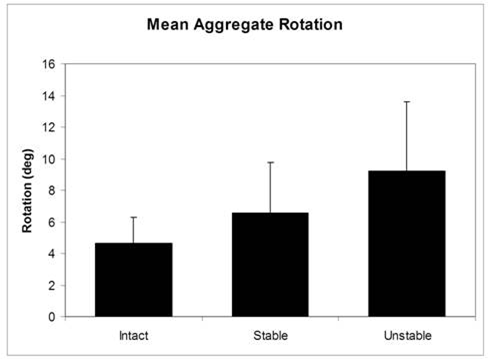
Figure 6. Osteotomy of the pars interarticularis doubled the amount of intervertebral rotation (p<0.05). Stabilization of the pars interarticularis produced a significant reduction in the amount of intervertebral rotation (p<0.05)
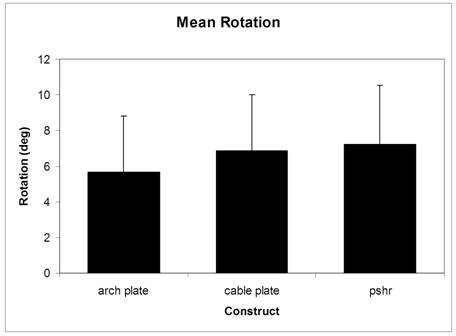
Figure 7. The arch plate was the most effective in reducing intervertebral rotation. This trend was not statistically significant
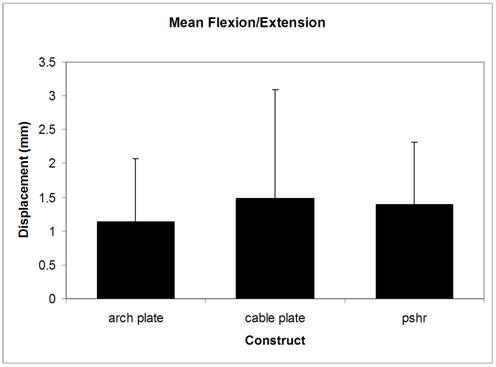
Figure 8. There were no significant differences in fracture gap displacement between the 3 constructs tested in flexion extension
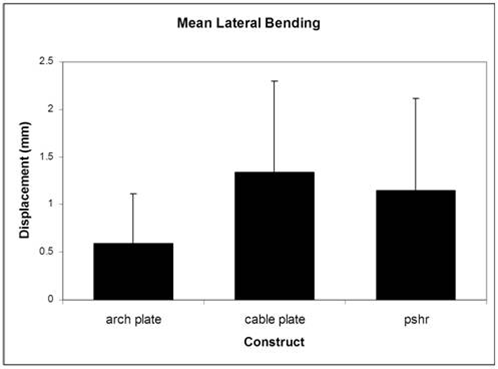
Figure 9. In lateral bending, the titanium miniplate was significantly better in reducing gap displacement when compared to the PSHR and cable plate (p<0.05)
References
Fredrickson BE, Baker D, McHollick WJ, Yuan HA, Lubicky JP. The natural history of spondylolisthesis and spondylolysis. J Bone Joint Surg Am 1984;66:669-707.
Baker DR, McHollick W. Spondyloschisis and spondylolisthesis in children. J Bone Joint Surg 1959;38:93–4.
Tower SS, Pratt WB. Spondylolysis and associated spondylolisthesis in Eskimo and athabascan populations. Clin Orthop Relat Res 1990;250:171–5.
Wiltse LL. The etiology of spondylolisthesis. J Bone Joint Surg [Am] 1962;44:539–60
Simper LB. Spondylolysis in eskimo skeletons. Acta Orthop Scand 1986;57:78–80.
Stewart T. The incidence of neural-arch defects in Alaskan natives, considered from the standpoint of etiology. J Bone Joint Surg Am 1953;35:937-50.
Albanese M, Pizzutillo PD. Family study of spondylolysis and spondylolisthesis. J Pediatr Orthop 1982;2:496-9.
Roche MB, Rowe GG. The incidence of separate neural arch and coincident bone variations; a summary. J Bone Joint Surg Am 1952;34:491-4
.
Stewart T. The incidence of neural-arch defects in Alaskan natives, considered from the standpoint of etiology. J Bone Joint Surg Am 1953;35:937-50.
Fredrickson BE, Baker D, McHollick WJ, Yuan HA, Lubicky JP. The natural history of spondylolisthesis and spondylolysis. J Bone Joint Surg Am 1984;66:669-707.
Baker DR, McHolick W. Spondyloschisis and spondylolisthesis in children [abstract]. J Bone Joint Surg Am 1956;38:933-4.
NeAlbanese M, Pizzutillo PD. Family study of spondylolysis and spondylolisthesis. J Pediatr Orthop 1982;2:496-9.
JoFriberg S. Studies on spondylolisthesis. Acta Chir Scand 1939:Supplementum 55.
Herman MJ, Pizzulitto PD. Spondylolysis and spondylolisthesis in the child and adolescent: a new classification. Clin Orthop Relat Res 2005; 434:46-54
Farfan HF, Osteria V, Lamy C. The mechanical etiology of spondylolysis and spondylolisthesis. Clin Orthop Relat Res 1976;117:40-55
Wiltse LL, Widell EH Jr, Jackson DW. Fatigue fracture: the basic lesion in isthmic spondylolisthesis. J Bone Joint Surg Am 1975;57:17-22.
Rossi F, Dragoni S. Lumbar spondylolysis: occurrence in competitive athletes. Updated achievements in a series of 390 cases. J Sports Med Phys Fitness 1990;30:450–3
Hoshina H. Spondylolysis in athletes. Phys Sportsmed 1980;8:75–7.
Ichikawa N, Ohara Y, Morishita T, et al. Aetiological study on spondylolysis from a biomechanical aspect. Br J Sports Med 1982;16:135–41
Jackson DW, Wiltse LL, Cirinciole RJ. Spondylolysis in the female gymnasts. Clin Orthop Relat Res 1976;117:68–73.
Kotani PT, Ichikawa MD, Wakabayashi MD, et al. Studies of spondylolysis found among weightlifters. Br J Sports Med 1971;6:4–8
.
Soler T, Calderon C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med 2000;28:57–62.
Brigham CD. Direct repair of lumbar spondylolysis in athletes. Oper Tech Sports Med 2005;13:108-113.
Hu SS, Tribus CB, Diab M, et al. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am, 2008;90:656-71.
Scott JHS. The Edinburgh repair of isthmic (Group II) spondylolysis [abstract]. J Bone Joint Surg Br 1987;69:491
Buck J. Direct repair of the defect in spondylolisthesis: preliminary report. J Bone Joint Surg Br 1970;52:432-7.
RReitman CA, Esses SI. Direct repair of spondylolytic defects in young competitive athletes. Spine J 2002;2:142-4.
Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of hook screw. Arch Ortho Trauma Surg 1984;103:175-8.
YGillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis using a rod screw construct and bone grafting of the pars defect. Spine 1999;24:1252-9.
Tokuhashi Y, Matsuzaki H. Repair of defects in spondylolysis in segmental pedicular screw hook fixation: a preliminary report. Spine 1996;17:2041-5
Deguchi M, Zdeblick T. Biomechanical comparison of spondylolysis fixation techniques. Spine 1999;24:328-33.
Mermelstein LE, McLain RF, Yerby SA. Reinforcement of thoracolumbar burst fractures with calcium phosphate cement: a biomechanical study. Spine 1998;23:664-70.
NUlibarri J, Anderson P. Biomechanical and clinical evaluation of a novel technique for surgical repair of spondylolysis in adolescents. Spine 2006;31:2067-72
Wilke HJ, Krischak S, Claes L. Biomechanical comparison of calf and human spines.J Orthop Res 1996;14:500-3.
Riley L. A biomechanical comparison of calf versus cadaver lumbar spine models.Spine2004;29:217-220.
|